
According to a World Health Organization (WHO) survey in 2020, the pandemic has disrupted mental health services in over 90 percent of countries globally. More than 60 percent of countries also reported disruptions to mental health services for vulnerable people, including children, adolescents, older adults, and women requiring antenatal or postnatal services. Estimates (2020) by the Lancet on the impact of the pandemic on global health suggest a rise in major depressive disorders by 28 percent and anxiety disorders by 26 percent. Mental health is estimated to cost the world economy US$6 trillion by 2030. Every dollar invested in evidence-based care for depression and anxiety returns US$5 in better health and productivity. Also, mental health is integral to achieving the Sustainable Development Goals (SDGs), particularly goal 3 (good health and well-being). Therefore, mental health needs to be prioritised from human rights and economic perspectives.
Widespread impacts
The pandemic has heightened the demand for mental health services, with fear, isolation, and the loss of lives and income triggering mental health conditions or aggravating pre-existing ones. Across societies, the effects of social isolation and the economic fallout have led to mental health distress. People are experiencing increased anxiety, depression, loneliness, and sadness because of the fear of infection, death, losing family members, losing incomes or livelihoods, or being socially isolated and separated from loved ones. In addition, individuals with preexisting mental illnesses or established mental illnesses and substance-use disorders are at an increased risk of infection with COVID-19 and have a higher risk of adverse physical and psychological effects. Unfortunately, 75 percent to 80 percent of the population suffering from mental disorders in middle-to-low-income countries never receive the necessary help.
According to the World Happiness Report 2021, mental health is one of the biggest casualties of the pandemic and the resulting lockdowns. Women, the young, and poor people have been the worst affected, thus, increasing the existing inequalities in mental wellbeing.
Children’s mental state has also been affected by forced confinements. Moreover, children, including adolescents, are at particular risk of abuse during the pandemic. The closure of schools combined with restrictions on movement has limited the scope for children to interact and access learning opportunities, taking a toll on their mental health. A UK-based study on young people with a history of mental health found that 32 percent of the respondents agreed that the pandemic had worsened their mental health. Family’s health, school and university closures, loss of routine and loss of social connection were causes of concern. Studies show changes in behaviour, with many being irritable and restless and an increased lack of concentration among school-going children. Stress and social isolation impact brain health and development, which increases the risk of developing lifelong challenges in children.
Women are at a greater risk of suffering mental health problems, with increased stress and anxiety due to their lower socioeconomic position relative to men, a heavier burden of daily chores, and a larger role in managing household food security. Sixty-six percent of women compared to 34 percent of men reported stress and anxiety during the pandemic in India. During the COVID-19 crisis, pregnant and new mothers are certainly more anxious due to potential difficulties in accessing services and social support and fear of infection. Lack of women’s empowerment, denial of decision-making capabilities, and domestic violence play a big role in the incidence of poor mental health conditions among women in developing countries. Similar findings have been reported for women in developed countries, and there have been calls to enact policies that prioritise women and their mental health during the pandemic.
Lack of women’s empowerment, denial of decision-making capabilities, and domestic violence play a big role in the incidence of poor mental health conditions among women in developing countries.
Frontline workers are also at high risk of internal ill health, including suicide attempts and the threats of collapse and stigmatisation. Studies among healthcare workers indicate increased depression, distress, insomnia, and the need for psychosocial support. Reports from Chile, Italy, Spain, the Philippines, the United Arab Emirates, the UK and the US document how dedicated teams provide mental health support for healthcare workers.
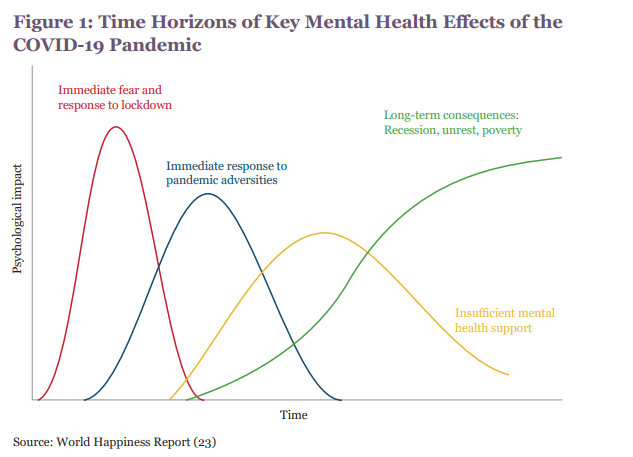
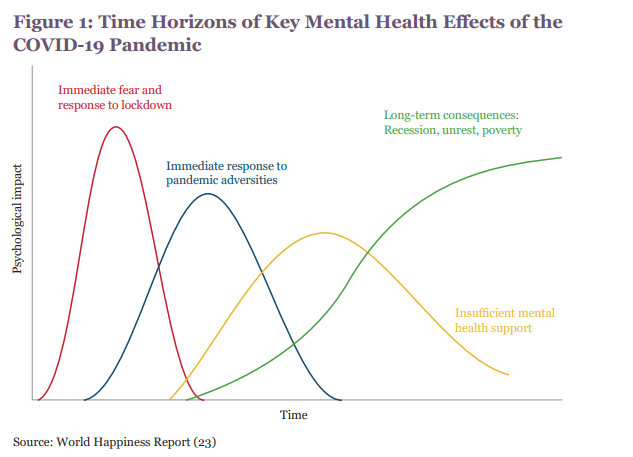
The impact of the pandemic on mental health is both short- and long-term and has been further aggravated by disruptions to mental health services and support during lockdowns(see Figure 1). Additionally, this negative impact can exacerbate the mental health crisis and cause a parallel pandemic that may last longer.
Investing in mental healthcare
“The extraordinary increase in mental health needs is taking its toll on already overburdened mental health services, which are under-funded and under-resourced in many countries on every continent affected by the COVID-19 pandemic. COVID-19 has exposed the serious gaps in mental health care, and now more than ever world leaders need to prioritise and ensure that quality mental health support is accessible to everyone, everywhere,” said Ingrid Daniels, President for the World Federation for Mental Health, in 2020.
School-based interventions that address anxiety, depression and suicide provide a return of US$21.5 for every US$1 invested over 80 years. Indeed, mental health services worldwide were already underfunded even before the pandemic hit, with countries spending lower than 2 percent of their public health budgets on mental health and struggling to meet their populations’ needs. In some of the world’s poorest countries, governments spend less than US$1 a person treating mental health conditions. Notably, the negative profitable consequence or inaction in treating mental illness is higher than the cost of treatment.
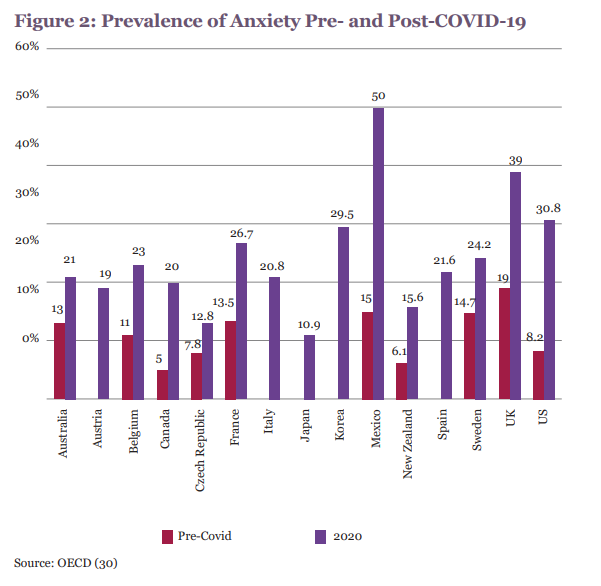
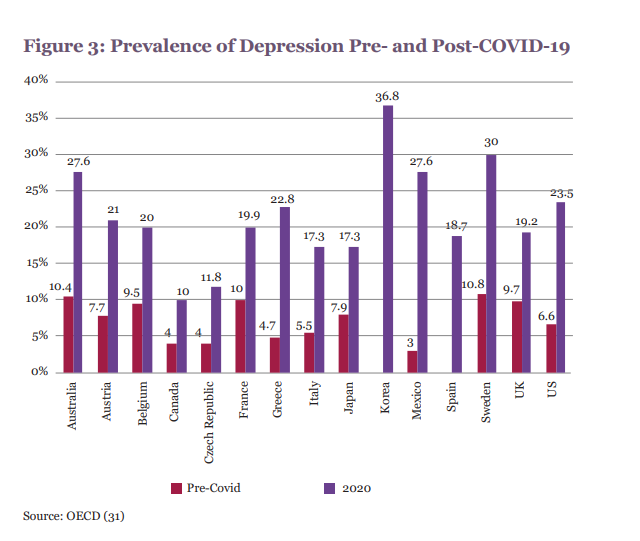
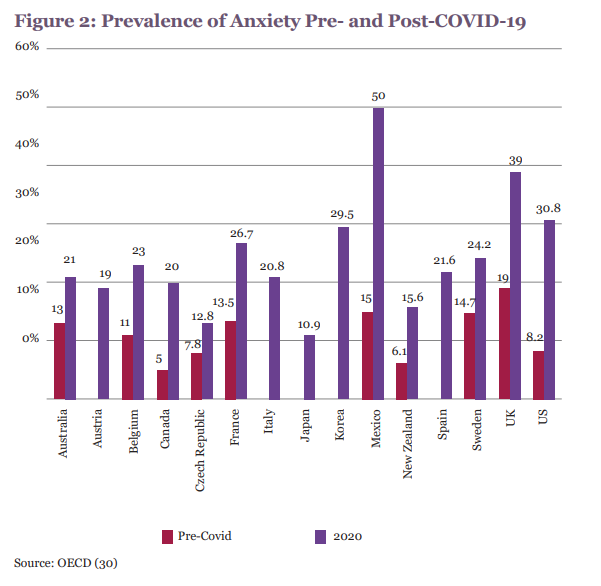
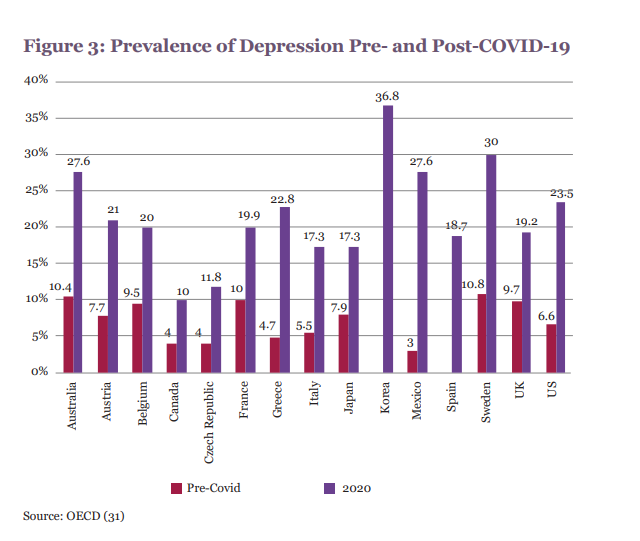
The prevalence of mental health conditions has been unchanged for decades; however, the COVID-19 crisis has increased the need for mental healthcare. The prevalence of anxiety increased significantly amid the pandemic (see Figures 2 and 3).
Middle-income countries are particularly affected by the COVID-19 pandemic due to several factors: a shortage of human resources, insufficient financial health, lack of personal protective equipment, and insufficient beds and supplies for treatment, such as mechanical ventilators. Many low- and middle-income countries lack adequate mental health resources to lessen the effects of job losses, income shocks and food insecurity caused by the pandemic. In addition, there are significant gaps in health budgets for mental health, with a high of 3 percent for higher-income countries to less than 0.5 percent in developing countries.
Poor mental health support in developing countries can lead to adverse socioeconomic outcomes and unescapable psychological distress.
Poor mental health support in developing countries can lead to adverse socioeconomic outcomes and unescapable psychological distress. In developing countries, medium- and small-scale businesses have been massively affected, while support from the government is often inadequate, and those reliant on the informal sector have experienced income loss and food insecurity. Governments in low- and lower-middle-income countries have yet to prioritise mental health in regular health systems. For example, while states in the US mandated mental health awareness in schools even before the COVID-19 pandemic, more than 75 percent of adolescents in India have never attended a mental health awareness session.
Public, perceived, and self-stigmatising attitudes to mental illness have been identified as critical barriers to mental healthcare-seeking behaviours. Mental health stigma prevents individuals from using mental health services or receiving treatment. Internalised stigma—shame and embarrassment and fear of disclosing one’s mental health conditions—also acts as deterrents. A 2018 survey reported that 42 percent of respondents cited high cost and poor insurance coverage as crucial walls to accessing mental healthcare, with one in four people being forced to choose between mental health treatment and essentials. Because of this prohibitive pricing, lack of insurance coverage, and the social stigma still associated with mental and substance use disorders, most people with behavioural health issues cannot access treatment.
Evidence from developing countries indicates higher stress levels and mental health issues in women with household food insecurity. A comparative study among seven middle-income countries on mental health in the general population during the pandemic highlights the risk factors for adverse mental health, including age (less than 30 years), high education, single and separated status and worrying about COVID-19. The lower-middle-income countries in Africa and Asia face the risk of an exacerbated burden of mental health issues due to weak health systems and the lower socioeconomic status of their populations. Access to healthcare services and governments’ responses to the pandemic on public safety measures were crucial in lowering levels of anxiety and depression in some developing countries.
The Way Forward
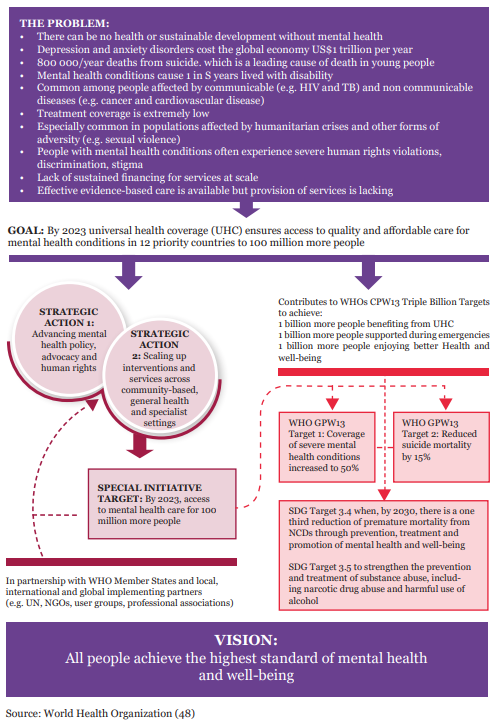
Mental health is integral to meet the SDGs, which calls for interdisciplinary and intersectoral solutions. Amid the pandemic, the WHO recommended the dedicated allocation of resources for mental healthcare in national response and recovery plans for countries to maintain mental health services. The WHO has also established a Special Initiative for Mental Health, which centres on scaling-up mental healthcare as part of universal health coverage and leaving no one behind by increasing quality interventions and services for individuals with mental health conditions.
Mental healthcare must be integrated into universal health coverage worldwide. For resource-constrained nations, low-cost scalable solutions are needed to address the mental health situation.
Figure 4: The WHO Special Initiative for Mental Health – Theory of Change
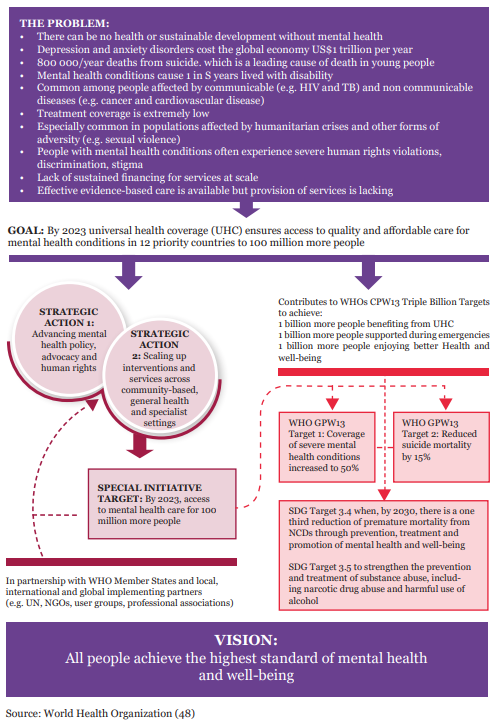
As adaptation towards telehealth increases across the globe, low and lower-middle income countries can leverage the technological shift by actively combating the gender/area digital divide, especially for women and racial minorities. Indeed, psychiatry has shown the highest adaptation among telehealth services globally. Mental healthcare must be integrated into universal health coverage worldwide. For resource-constrained nations, low-cost scalable solutions are needed to address the mental health situation.
The psychological impact of the pandemic has highlighted the vulnerability of people and the need for additional mental health support around the world. This momentum can be seen as an opportunity to address the unmet needs of the vulnerable groups by considering effective ways of investing in mental health support to improve overall wellbeing. Mental health issues should be incorporated within general health policies and plans and should be carefully monitored and evaluated to achieve the desired outcomes.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.




 PREV
PREV


