-
CENTRES
Progammes & Centres
Location
 PDF Download
PDF Download 
Oommen C Kurian and Shoba Suri, “Weighed Down by the Gains: India’s Twin Double Burdens of Malnutrition and Disease”, ORF Occasional Paper No. 193, May 2019, Observer Research Foundation.
Introduction
Research published in the reputed medical journal, Lancet in 2016 showed that the world has transitioned from an era when underweight prevalence was more than double that of obesity, to one in which more people are obese than underweight.[i] Countries like India, however, are at that phase of the transition where public policy challenges of overnutrition[1] are adding to, instead of replacing those posed by undernutrition. Undernutrition remains a leading cause of childhood morbidity and mortality in India and in many parts of the world, and thus, the World Health Organization (WHO) has launched the United Nations Decade of Action on Nutrition, 2016-2025.[ii]
India’s record of high economic growth over the past decade has not transformed the nutritional status of its population to the extent necessary: latest research shows that despite doubling the rate of stunting reduction in the past 10 years from the previous decade, India still has the largest share of the world’s undernourished population.[iii] The World Bank (WB) has declared that with 40 percent of its workforce having experienced stunting[2] as children, India is simply not going to be able to compete in the future economy.[iv] Indeed, the Global Hunger Index (GHI) ranked India at 103 among 119 countries in 2018, in view of the prevalent undernutrition situation.[v] At the same time, overnutrition is emerging as a silent epidemic in many parts of the country, and the current healthcare delivery system is barely equipped to deal with this additional policy challenge. The WHO groups India—with over 10 percent of under-five children overweight—with Thailand and Indonesia in the region, both of which have much higher per capita incomes. The proportion of overweight children is less than three percent in countries like Bangladesh, Myanmar, Nepal and Sri Lanka.[vi]
This paper explores the interaction between the country’s nutritional and epidemiological transitions, and maps appropriate policy responses. In the wake of urbanisation, globalisation and economic growth, there has been a major shift in the nutrition profile of the population. This shift is characterised by high rates of undernutrition alongside high and increasing rates of overweight and obesity. Simultaneously, the proportion of diet-related non-communicable diseases (NCDs) is increasing as a major cause of death even as the communicable, maternal, neonatal and nutritional causes (referred to as “Millennium Development Goals (MDG) conditions”) are coming down.
India has witnessed significant progress towards the MDGs; however, progress has been inconsistent, and even in states where absolute levels of “MDG conditions” are still very high, the NCD proportion is growing fast. The imperative is for greater integration between health and nutrition policy at every level of governance. Sustainable Development Goals (SDG) gives India the opportunity[vii] to broaden nutrition policy from the limiting focus on women and children, and fully harness the benefits of its demographic dividend. The paper suggests that it is time to re-visit an earlier proposal for a joint Ministry of Health and Nutrition, and start a national conversation.
Nutrition in India: Current situation
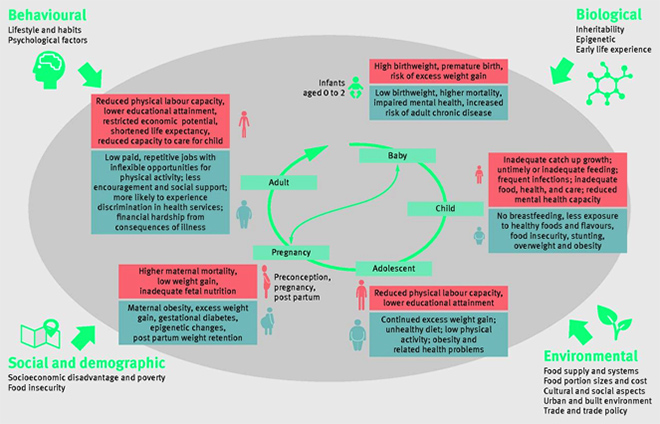
The United Nations Children’s Fund (UNICEF) considers nutrition as a pillar of human development and recommends concrete, large-scale programming not only to reduce the burden of undernutrition and deprivation in countries, but also to advance economic progress. There is no dearth of evidence to show that almost every perceivable development challenge is made worse by malnutrition.[viii] In India’s case, along with undernutrition and micronutrient deficiencies, the last decade also saw the emergence of overweight and obesity, contributing to the disease burden just as undernutrition does. A 2018 study covering children aged 6–19 years from rural or urban schools found that one in every nine schoolchildren suffer from overnutrition.[ix] (See Figure 1 for an illustration of the pathways to multiple forms of malnutrition, particularly in a low-income setting.)
Figure 1: Pathways to the multiple forms of malnutrition
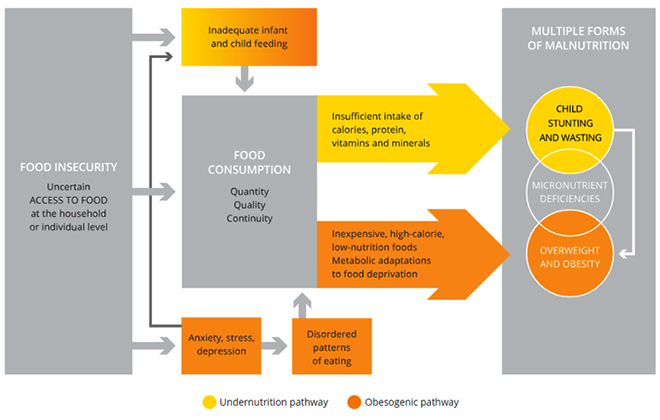
The challenge to India’s policymakers is that fighting malnutrition is increasingly requiring a two-pronged approach. Such strategy will need to be modulated at the state level or below, according to the ground reality.
A 2016 Global Burden of Disease Study by Lancet ranked the risk factors according to attributable burden of disease for India. For 2015, out of the top ten risk factors in terms of disability-adjusted life-years, six were linked to nutrition (i.e., hypertension, high glucose, childhood undernutrition, high cholesterol, iron deficiency, and lack of whole grains in diet).[x] Following a global trend, the proportion of deaths in India due to infectious diseases, direct nutritional causes as well as maternal and child deaths have declined, whereas mortality from indirect nutritional causes through NCDs have risen on average. [xi]
Stunting and wasting
The Global Nutrition Report[xii] found that India has the world’s largest number of stunted (46.6 million) and wasted children (25.5 million). Two percent of its under-five children are overweight. Twenty-three percent of women and 20 percent of men age 15-49 are underweight, and almost the same percentage are overweight or obese (21 percent of women and 19 percent of men). The proportions have doubled in the last decade. The latest national data available on nutrition suggests that over the last decade, the incidence of undernutrition has reduced rather slowly and not commensurate to the country’s economic growth.[xiii]
According to the National Family Health Survey (NFHS) 4 (2015-16), the percentage of under-five children who are stunted declined to 38.4 percent from 48 percent a decade ago. Barring Puducherry, Delhi, Kerala and Lakshadweep, all other states have a higher proportion of stunted children in rural areas than the urban. Meanwhile, the percentage of children under-five who are wasted[3] increased over the last ten years, from 19.8 percent to 21 percent. The proportion of children who are severely wasted also increased from 6.4 percent to 7.5 percent between 2005-06 and 2015-16.
Latest data[xiv] show that stunting prevalence tends to increase with age, peaking at 18-23 months. Timely interventions of breastfeeding, age-appropriate complementary feeding, full immunisation and vitamin A supplementation have been proven to be effective in improving outcomes in children. Almost double the prevalence of stunting is found in children born to mothers with no schooling as compared to mothers with 12 or more years of schooling. Stunting also shows a steady decline with increase in household income/wealth quintile. The inter-generational cycle of malnutrition is to be tackled with effective interventions for mother (pre- and post-pregnancy) and child to address the high burden of stunting, especially in rural areas.
Stunting is more prevalent in children from Hindu and Muslim backgrounds than those from Christian, Sikh or other religions. Stunting was equally prevalent in Adivasi (Schedule Tribes) and Dalit (Schedule Castes) communities. In terms of geographical regions, Bihar (48 percent), Uttar Pradesh (46 percent) and Jharkhand (45 percent) have the highest rates of stunting, breaching the national average of 38. While stunting has improved across all states, inter-state variability still remains extremely high. The most significant decline has been noted in Chhattisgarh with over a 15-percentage point drop in the last decade. Tamil Nadu has had the least progress.[xv]
Figure 2: Prevalence of wasting in India
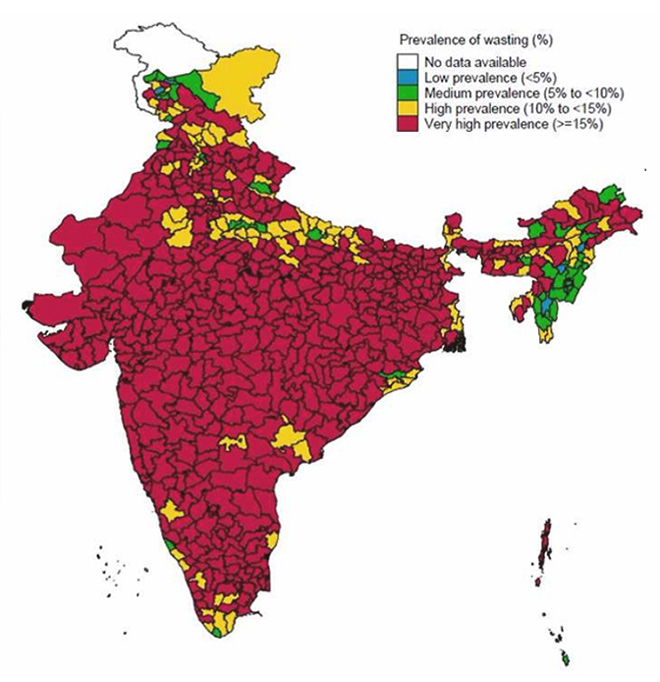
India has nearly halved the proportion of its stunted children (38.4 percent) from what it was in the late 1980s (66.2 percent). However, this gain is offset by the regression in wasting, which is currently at the level it was three decades ago (21 percent).[xvi] Wasting is widespread in India (See Figure 2) and has worsened in the last decade from 20 to 21 percent. The country accounts for the largest number of wasted children in the world (25.5 million) which is almost half of the total.[xvii] Unlike stunting, there is no stark variation in wasting prevalence across rural and urban areas, nor by gender. However, higher rates have been observed among the Adivasi (27.4 percent) community and the “Other” category of religion (29.2 percent). Among the children defined as wasted, more than one-third are six months of age (31.9 percent), with the proportion slowly declining to 17.7 percent among the five-year-olds.14 The poorest quintile households show highest wasting (23.5 percent) above national average.
It is worrisome that states like Tamil Nadu and Goa, whose stunting levels are relatively low, are among the “worst performers” in reducing wasting.[xviii] In fact, Goa has a higher rate of wasting than of stunting, a peculiar situation similar to Sri Lanka. [xix] Between 2005 and 2015, the proportion of children and pregnant women who are anaemic across India have come down by 11.1 and 8.5 percentage points, respectively. More than a third (35.7 percent) of children were underweight in 2015—this marks a slow decline from the 2005 levels (42.5 percent), considering that this was a time when the government appeared to be paying greater attention to food security policy.[xx]
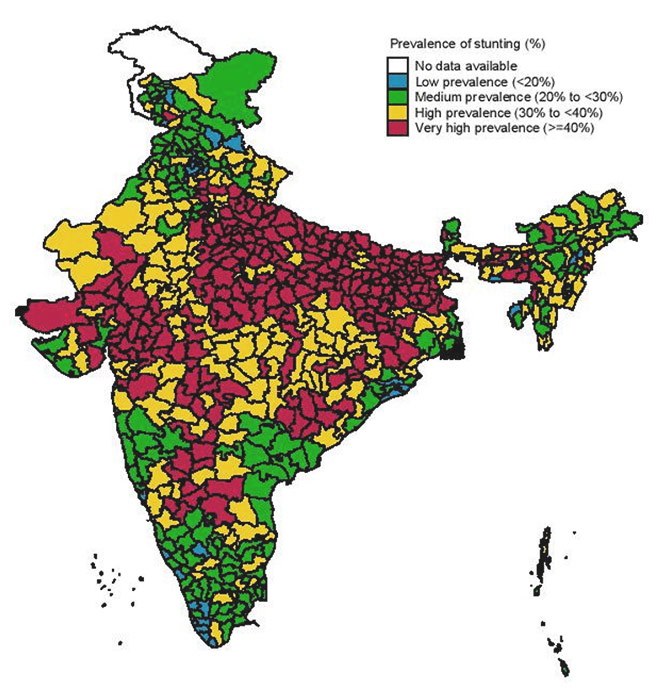
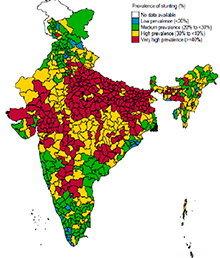
Analysis by the International Food Policy Research Institute (IFPRI) has shown that 239 districts in India have stunting rates above 40 percent. Stunting shows wide regional differences as well (See Figure 3): the best performing district in India has only 12.4 percent children stunted, but on the other end, there is a district with a proportion of 65.1 percent stunted children. For anaemia among women, the range is from nine percent to 83.2 percent. Similarly, while India has a district with only 1.8 percent of children wasted; there are at least seven districts where the proportion is more than 40 percent. The India average for wasting is 21 percent. [xxi]
Figure 3: Stunting across India
Interventions for malnutrition
An observational study suggests that a medium-term strategy for preventing and managing acute malnutrition should involve primarily mobilisation of women’s groups for action on nutrition, as well as direct services through a general village-based childcare programme. These are effective interventions in terms of mortality reduction, and the cost, degree and pace of improvements. [xxii]
Undernutrition sets in during the first two years of life, at the time when the brain develops about 85 percent of its full capacity.[xxiii] UNICEF has repeatedly called attention to the critical windows of opportunity for preventing undernutrition: the first two years of a child’s life; the adolescence years for girls; and pregnancy and lactation for mothers. These are the periods of time when proven nutrition interventions offer children the best chance to survive and reach their optimal growth and development. Optimal infant and young child feeding practices include initiation of breastfeeding within one hour of birth; exclusive breastfeeding for the first six months of the child’s life; and continued breastfeeding for two years or more, together with safe, adequate and appropriate complementary foods starting at six months of age. [xxiv]
Breastfeeding plays a role in decreasing the mother’s risk for breast cancer and protecting against overweight and diabetes for the child.[xxv] Breastfeeding also helps increase the child’s IQ[xxvi] and promotes a strong bond between the mother and infant. Finally, breastfeeding is directly linked to attainment of at least four of the Sustainable Development Goals (SDGs) i.e. health, nutrition, poverty reduction and inequity reduction.[xxvii] According to WHO,[xxviii] suboptimal breastfeeding (specifically, non-exclusive breastfeeding) and inadequate complementary feeding contribute to stunting, wasting and childhood overweight. The potential impact of optimal breastfeeding is evident in not only developing countries, but in developed countries as well.[xxix]
India has made significant progress in promoting breastfeeding since the decline of the practice in the 1970s and ‘80s.[xxx] The NFHS 4 (2015-16) showed that India’s rate of early breastfeeding within an hour is 41.5 percent, increasing from 23.4 percent in NFHS 3 (2005-2006), marking an increase of 1.7 percent per year. The NFHS 4 also showed that 21 percent of newborns receive pre-lacteal feeds.[4] It is important to note that only 41.5 percent of children are suckled within an hour of birth, when 79 percent of mothers had institutional delivery. This shows that every second mother delivering in health facilities did not begin breastfeeding within one hour of birth.[xxxi]
Overall, 54.9 percent of mothers exclusively breastfeed their infants, marking a gain of one percent per year as compared to NFHS 3. Only 1 out of 2 women are able to practice exclusive breastfeeding for the first six months of their infant’s life. Complementary feeding rates after six months is 42.7 percent. Between NFHS 3 and 4 there has been a 10-percent decline in infants receiving complementary feeds in six to eight months. Adequate complementary feeding and minimum acceptable diet among 6-23 month-old children is alarmingly low at 9.6 percent (or 1 of every 10) children have received minimal acceptable diet[5]. Data from NFHS 4 indicate that 10 percent of infants are introduced to complementary feeding before six months, and 58 percent after eight months, when both too early and too delayed are detrimental to their health.[xxxii]
Despite a 55-percent exclusive breastfeeding rate in children below six months, some 99,499 children under five die each year as a result of diarrhoea and pneumonia—both of which could have been prevented through early initiation of breastfeeding, exclusive breastfeeding for the first six months, and continued breastfeeding beyond.[xxxiii]
Creeping obesity epidemic
The importance of acknowledging that undernutrition is still a predominant problem cannot be overemphasised enough. However, obesity is also emerging as a stiff policy challenge. Parallel to the slow decline of undernutrition is the rapid increase of overweight and obesity numbers across the country. The proportion of overweight or obese women (15-49) increased from 13 to 21 percent, and from nine to 19 percent for men. In addition, there has been an increase in the mean BMI from 20.5 in 2005-06 to 21.9 in 2015-16.
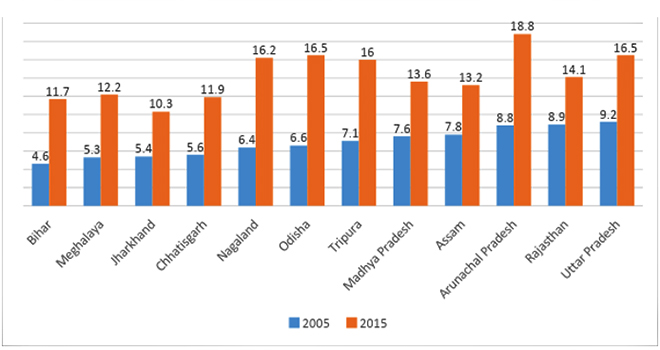
In 2005, out of 30 states and union territories for which data were available, 12 had a proportion of obese or overweight women under 10 percent. Meanwhile, 17 out of 30 states had a proportion of obese or overweight men under 10 percent. After ten years, in 2015, out of 36, the number of states and UTs with less than 10 percent of obese or overweight women and men is zero.[xxxiv] What is often called “the overnutrition epidemic” has been historically more visible in richer states and in urban areas in particular. However, a study by the Institute of Health Management Research in 2015 showed that for the richer states in India, the problem of overweight in women has widened from urban and well-off to the poor and rural. However for the poorer states, overweight and obesity have remained mostly among the urban and richer sections of the population.[xxxv]
It is just a matter of time, given the current rates of increase in overweight/obesity numbers, before India has more people suffering from over nutrition than undernutrition. The following Figure 4, based on an exercise focusing on the states with under 10 percent levels of overweight/obesity in 2005, demonstrates the pace at which the incidence of obesity is increasing. In each of the low-prevalence states of 2005, overweight/obese population have shown a dramatic increase over the last decade. In seven of these 12 states, the proportion more than doubled. These also happen to be states with a relatively higher burden of undernutrition as well. Overall, 11 out of 36 states and UTs in India currently have more than 30 percent women who are in the obese/overweight category, and eight out of 36 states and UTs have more than 30 percent men who are obese/overweight.[xxxvi]
Figure 4: Women who are currently (2015) overweight/obese in States with low burden in 2005
These numbers may in fact be understated, given the issues with global definitions and thresholds. A WHO expert consultation in 2004 proposed different cut-offs for overweight (23.0-26.9 BMI) and obesity (> 27.0 BMI ) for Asians on the basis of available data which suggests that Asians have a higher percentage of body fat than, say, European populations, which makes them vulnerable to NCDs even at a lower level of BMI.[xxxvii] Studies have shown that South Asians in particular, have more severe inflammation, insulin resistance, and liver fat even when non-obese by the BMI standards used for Caucasians.[xxxviii]
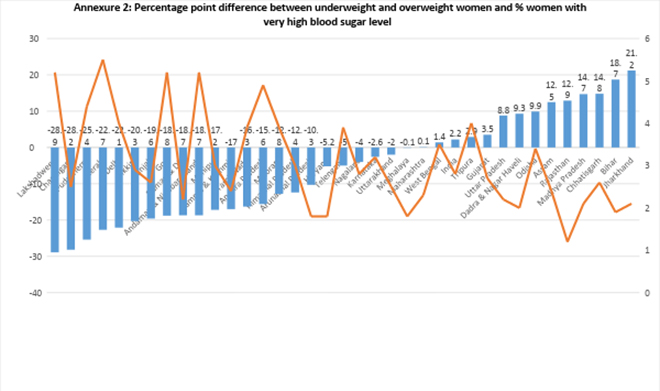
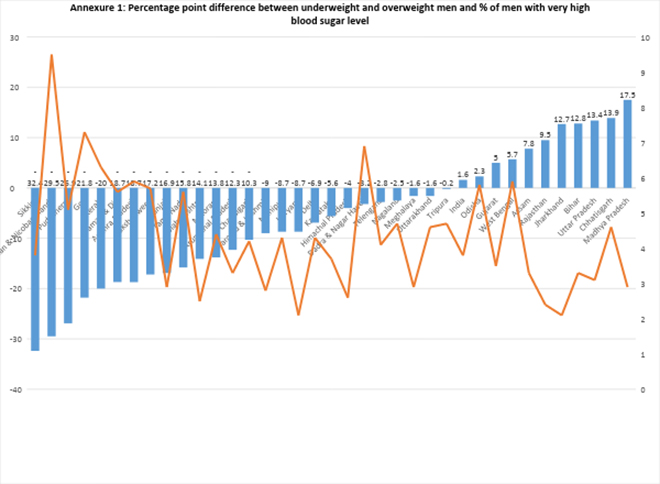
This would mean a drastic upward revision of India’s overweight/obesity estimates, as NFHS factsheets calculate overweight/obesity numbers using the 25.0 BMI threshold. If 23.0 were to be used instead, the estimates would be considerably higher. Given that even with the 25.0 cut-off, India has 23/36 states and UTs with more overweight/obese than underweight women, with a lower minimum, India may already have more overweight/obese women than underweight (See Annexure 1). India’s 26/36 states also happen to have more overweight/obese men than underweight (See Annexure 2).[xxxix] According to consensus statement on the revised BMI for Asian Indians it will have implication on the number of underweight as well, as the cutoff point will be shifted from 18.5 to 18, which may bring down the number of underweight further, and amplifying the relative significance of overweight/ obesity as a public health issue.[xl]
Studies have shown dramatic changes in the magnitude of obesity/overweight in Indian population when the BMI cut-off is shifted from 25.0 to 23.0. For example, a 2017 study by ADB using DLHS 4 data show that if a lower BMI cutoff of 23 were to be used, in states such as Kerala, the prevalence of overweight or obesity in 2012–13 would go up from 30 to 48 percent.[xli] A study on implication of the revised consensus BMI for Asian Indians, showed significant increase in prevalence of obesity and overweight pregnant women and shift in women with normal BMI being reclassified as overweight.[xlii]
An analysis [xliii] on the trend in data in the prevalence of overweight/ obesity among women from NFHS 1 to NFHS 4 has shown the rise from only six states (Punjab, Haryana, Delhi, Gujarat, Kerala, and Goa) in 1998-99 to 20 states in 2015-16 where prevalence of overweight/obesity among women was more than 15 percent. States like Delhi, Goa, Andhra Pradesh, Kerala, Punjab, and Tamil Nadu in 2015-16 raises serious concerns where more than 30 percent women were overweight/obese. Another study based on analysis of NFHS data from a decade ago found that when using Asian population-specific cut-offs, 11 states in India could be classified as “double burden states”; however, following traditional categorisation, only less than half the number qualified.[xliv] This means that a more realistic assessment of overnutrition will need to be conducted at the earliest so that the government’s efforts at fighting NCDs can be evidence-based and effective.
India’s epidemiological, nutritional, and demographic transitions
The causes of the double burden of malnutrition in India are related to a sequence of epidemiological changes known as the nutrition transition, the epidemiological transition and the demographic transition. (Figure 5 shows the biological, environmental, social and behavioural factors that drive the double burden of malnutrition.)[xlv] The Health Survey and Development Committee was established in 1943 by the British colonial government under the leadership of Sir J W Bhore. In its final report in 1946, the committee suggested that the annual loss of human capital in India because of malnutrition and preventable morbidity would be so startling that “the whole country would be aroused and would not rest until a radical change had been brought about.”[xlvi] However, no “radical change” was to be and, as enunciated by Dreze and Sen, the neglect and its far-reaching consequences have received scant attention in public discussions in post-independence India.[xlvii]
Figure 5: Drivers of India’s double burden of malnutrition
India is indeed undergoing simultaneous transitions. Research has shown that the multiple burdens of persistent undernutrition, micronutrient deficiencies, and rising overnutrition contributing to disease load are mere manifestations of the ongoing economic, social, lifestyle, demographic, nutrition as well as epidemiological transitions in India.[xlviii] Demographically, India is undergoing a slow transition from a regime of high birth and death rates to one of low birth and death rates, on the average, with a rise of about 10 years in the average life expectancy every two decades.[xlix] The epidemiological transition involves a double burden of communicable diseases (tuberculosis, malaria, HIV/AIDS, leprosy, dengue, diarrhoeal diseases) and fast increasing non-communicable diseases (heart and lung diseases, stroke, cancer, diabetes). In parallel, a nutritional transition is emerging, and India’s historical problem of undernutrition is being compounded by overnutrition.
The interaction between these transitions at multiple levels can be complex and seemingly counterintuitive. For example, studies show that in developing economies, undernutrition among children and overnutrition among adults can often co-exist within the same household; the phenomenon is known as intra-household dual burden of malnutrition. Almost 10 percent of households in many African and Asian countries have a stunted child and an overweight mother,[l] and analysis based on IHDS data for 2011-12 (using the lower BMI threshold of 23 kg/ m2) showed that India had five percent and eight percent of such households in the rural and urban areas, respectively.[li]
Malnutrition and disease
The WHO Global Report on Diabetes (2016)[lii] observed that mirroring the global increase in the number of people who are overweight or obese, diseases like diabetes have expanded substantially. The spread of diabetes has been faster in low- and middle-income countries than in high-income ones. WHO’s conceptual framework (See Figure 6) shows the interlinkages between disease and malnutrition.
Figure 6. WHO’s conceptual framework of the double burden of malnutrition
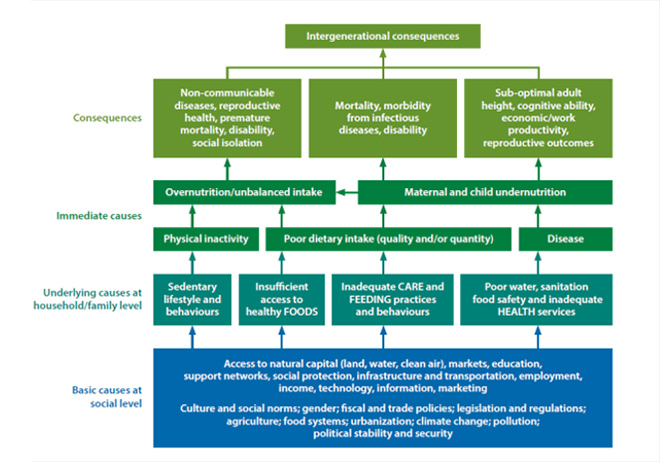
A Working Group appointed by the Ministry of Women and Child Development in 2006 as part of the 11th Five Year Plan(2007–2012) exploring the possibility of integrating nutrition with health had called nutrition and health as two sides of the same issue and that these are therefore, inseparable.[liii] The primary difficulty in assessing the disease burden in India is lack of adequate and reliable data. India does not have reliable regular numbers on the disease burden, despite having multiple national surveys dealing with health. India’s Health Management Information System does not cover the private sector adequately, and as a result, there are massive upward revisions at regular intervals on the disease burden. The number of estimated deaths by tuberculosis (TB) in India was doubled in 2015–480,000 deaths, up from 220,000 deaths in 2014.[liv] In 2013, a Government of India committee reportedly found that the actual number of malaria deaths in India would be at least around 20-30 times higher than earlier estimates.[lv]
Undernutrition and disease conditions interact at multiple levels. In India, it contributes heavily to the mortality and morbidity burden. Despite the launch of many health programmes and slow improvement, Infant mortality rate (IMR) was at 34 per thousand live births in 2016 and Under-5-mortality rate (U5MR) was at 43 per thousand live births in 2015. Both IMR and U5MR came down from 55 in 2007 and 55 in 2011, respectively. Analysis based on NFHS 4 [lvi]showed that childhood undernutrition accounts for 45 percent of U5MR alone and remains a key public health challenge in India. If a child is undernourished, the chances of deaths due to respiratory infections, diarrhoea, malaria, measles, and other infectious diseases are increased considerably.[lvii] Earlier studies have shown that more than half of child deaths from malaria (57 percent), diarrhoea (61 percent) and pneumonia (52 percent), as well as 45 percent of deaths from measles are associated with protein-energy malnutrition and micronutrient deficiencies in India, where child malnutrition is responsible for 22 percent of the country’s overall burden of disease.[lviii] While the disease burden due to child and maternal malnutrition has dropped in India substantially since 1990, it is still responsible for 15 percent of the total disease burden in India in 2016.[lix]
On the other hand, infections are known to contribute to existing burden of undernutrition too. In the case of anaemia, Malaria is among the prominent causative factors, along with iron, folic acid and Vitamin B12 deficiencies. [lx] According to a report on India’s state level disease burden, child and maternal malnutrition contributes to disease through increasing the risk of neonatal disorders, nutritional deficiencies, diarrheal diseases, lower respiratory infections, and other common infections.[lxi]
Malaria also adds as a contributor to India’s burden of undernutrition. India accounts for six percent of all malaria cases in the world, and six percent of the resultant deaths.[lxii] Latest data[lxiii] show that even as India has progressed in reducing malaria cases by 24 percent, it still contributes to 80 percent of the global malaria burden. A majority of malaria cases in India are reported from the eastern and central parts of the country and from forest, hilly and tribal areas. These states include Odisha, Chhattisgarh, Jharkhand, Madhya Pradesh, Maharashtra, and some north-eastern states like Tripura, Meghalaya and Mizoram.[lxiv]
India launched its five-year National Strategic Plan for Malaria Elimination in 2017 with shifted focus from malaria “control” to “elimination” and provided a road-map with targets to end malaria in 571 districts out of India’s 678 districts by 2022.[lxv] The drop in malaria cases in India is attributable partly to Odisha, where innovations in improving healthcare worker skills, expanding access to diagnostics and treatment and strengthening data collection have led to a pathbreaking decline of incidence. [lxvi]
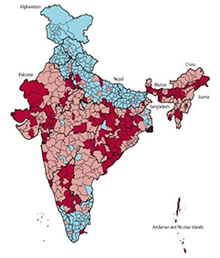
Malaria and Malnutrition frequently co-exist.[lxvii] Studies have shown that children with Malaria are more likely to become malnourished, and that these two have a synergistic relation. [lxviii]–[lxix] While it is established that malnourished children are less likely to survive an attack of severe falciparum Malaria, and that infections like Malaria can cause anaemia and undernutrition, the impact of chronic or recurrent malaria on malnutrition is not well studied in India. However, there are practitioners who work closely with communities where what is called ‘Malaria-Induced Malnutrition’ is high, and treatment for malaria has shown dramatic improvement in the nutritional status growth pattern of the children.[lxx] Interestingly, as Figure 7 shows, district-level maps of India showing malaria-endemic areas as well as high levels of chronic malnutrition among children show a considerable overlap.
Figure 7: Spread of Chronic Malnutrition (Stunting), Malaria and Underweight in India
 |
 |
 |
|
Sources: Map 1 showing levels of stunting by district in 2015-16 : http://poshan.ifpri.info/2017/05/09/how-are-indias-districts-doing-on-maternal-infant-and-young-child-nutrition-insights-from-the-national-family-health-survey-4/ Map 2 showing districts with Plasmodium falciparum endemic areas (pink) and 10% or greater chloroquine-treatment failure (red) in any study between 1978 and 2007 within those districts: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3068018/ Map 3 shows level of underweight by district in 2015-16 http://niti.gov.in/content/nutrition-charts |
||
Some studies from Africa have shown a risk association between falciparum Malaria and subsequent poor incremental weight gains, negative impacts height as well as weight for age among children.[lxxi]A systematic review on the complex interaction between Malaria and malnutrition has found existing evidence to be inconclusive.[lxxii] An expert consultation in Bhubaneswar (2019) titled “Current Advances in Malaria Management and Implications for Malnutrition” concluded that there is a statistically significant correlation between Malaria and malnutrition, and that the Mal-Mal linkage theory is right. It also suggested screening of Malaria in malnourished children under five in Malaria endemic regions as an essential intervention for reduction of morbidity and mortality due to malnutrition. [lxxiii]
Figure 8: Prevalence of anemia among women (NFHS 4)
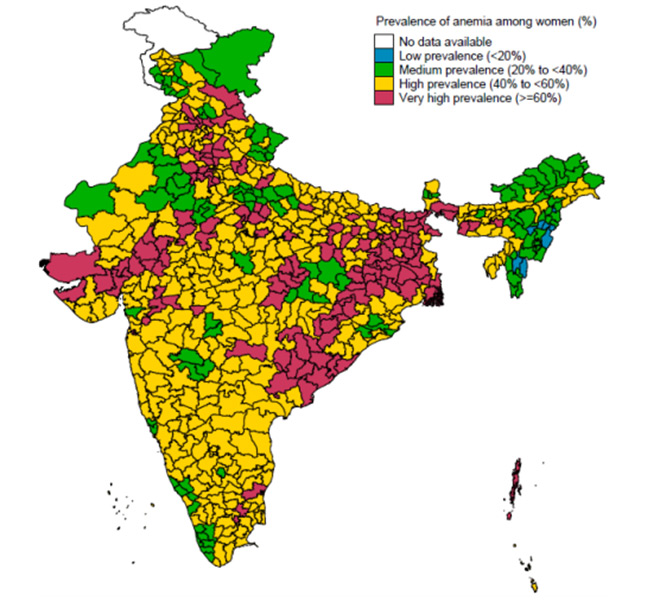
As 13/36 states and UTs in India have more than 60 percent children anaemic, and 14 states have more than 50 percent of the pregnant women anaemic (Figure 8), Malaria control should be part of nutrition policy as much as it is of health policy, given that Malaria is an established cause of anaemia. However, the relationship between chronic, recurrent Malaria and different forms of malnutrition needs to be systematically explored in India, particularly in areas that show a high overlap of both. As Malaria mortality rates are seen to be proportionate to the degree of malnutrition, policies informed by such studies will help reduce the burden of malaria as well as malnutrition.[lxxiv]
Similar to Malaria, undernutrition and Tuberculosis (TB) are also closely linked and have a two way causal association, as being underweight is both a cause and consequence of the disease.[lxxv] The impact of nutritional status on the occurrence, morbidity and mortality pattern in infectious diseases like Diarrhea, Tuberculosis (TB) and HIV has been well documented. [lxxvi] Many of these communicable diseases arise of poverty and are often co-morbid with undernutrition. A study in 2018 suggested that undernutrition impairs innate and adaptive immune responses needed to control Tuberculosis infection. [lxxvii] Predictably, a higher BMI is associated with lower mortality risk in Indian TB patients.[lxxviii] The aggregate numbers can be substantial: India alone accounts for 27 percent of global TB cases, and undernutrition is a key mortality risk factor along with smoking, as the WHO ten year review of 2017 observed. [lxxix] Available data suggest that more than a million TB patients in India are also suffering from undernutrition.[lxxx]
Non-communicable diseases
The rise of non-communicable diseases (NCDs) – heart disease, cancer, diabetes, and chronic respiratory diseases is putting pressure on the capacities of developing country health systems, which are geared towards dealing with infectious diseases and other “MDG conditions”. NCDs are aptly termed by the WHO as the ‘slow-motion disaster’ of our times. [lxxxi] Unhealthy diets, physical inactivity, excessive drinking and tobacco use are driving the global NCD epidemic, and India is no exception. More than half of all deaths in India today are caused by NCDs. As seen in Figure 9—based on an Indian Council of Medical Research-India Diabetes (ICMR-INDIAB) study[lxxxii] on diabetes—patients with NCDs can have substantially enhanced risks for comorbidities, which complicates treatment options and undermines wellbeing. It is estimated that heart diseases, stroke and diabetes are projected to cost India US$237 billion over the decade 2005-2015.[lxxxiii]
Figure 9: Prevalence of coronary artery disease (CAD) among subjects with and without diabetes
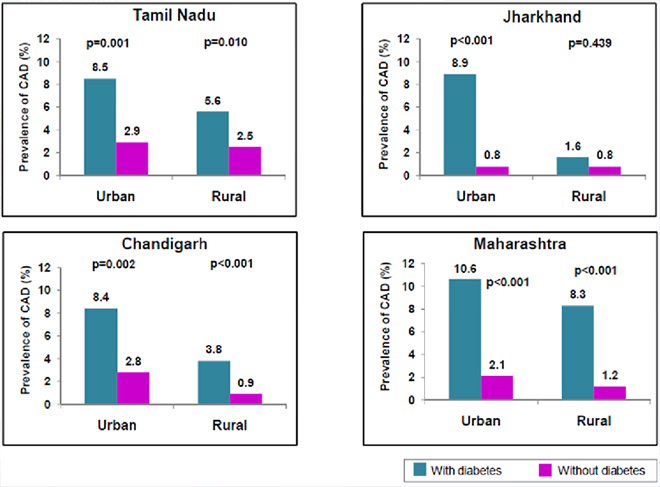
Results from the study also show that increasing levels of physical inactivity is a major risk factor in India, with only fewer than 10 percent regularly engaging in recreational physical activity. The study estimated the number of inactive individuals in India to be 392 million. The prevalence of physical inactivity was significantly greater in urban areas (65.0 percent) compared to rural areas (50.0 percent) and among females (63.0 percent) compared to males (45.7 percent).[lxxxiv] These numbers are in line with the overweight/obesity trends from the latest NFHS round, where women and urban areas reported higher levels of overweight and obesity than men and rural areas.[lxxxv] Lack of physical activity predisposes one to diabetes and makes its management more difficult.[lxxxvi]
Nutritional transition
Diseases and malnutrition interact across the spectrum. Undernutrition largely affects communicable diseases, and NCDs are largely affected by overnutrition. Those undernourished are more likely to experience disease and are more likely to die if they do contract a disease. The overweight and the obese are at a higher risk of NCDs. NFHS 4 gives evidence of higher incidence of obesity and overweight in the working age as well. Currently, cardiovascular diseases are by far the biggest cause of death in 30-69 years age group accounting for almost every third death. It is bound to increase in the coming years.
In short, chronic undernutrition increases the incidence of respiratory infections, Diarrhoea, Malaria, Measles, and other communicable diseases at one end of the spectrum[lxxxvii], and on the other end, overnutrition and unhealthy diet increases the chance of developing non-communicable diseases. In addition, the poor population, typically exposed more to communicable diseases due to living and working conditions have an additional handicap vis-à-vis NCDs as low birth weight and undernutrition during early childhood are associated to increased risk of diabetes and cardiovascular diseases later in life.[lxxxviii]
Current mortality trends
The National Health Policy 2017 (NHP) acknowledged the rapidly changing disease patterns as part of India’s health transition. According to NHP, communicable diseases currently contribute only to 28 percent of the entire disease burden, while non-communicable diseases (60 percent) and injuries at (12 percent) now constitute the major part.[lxxxix]
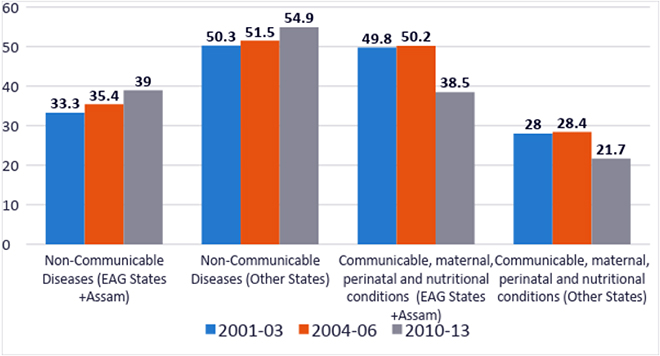
The Sample Registration System (SRS) provides one of the most reliable sets of data in terms of causes of death, and as multiple data points are available to track trends, it will be used for the following analysis.[xc] Causes of death can give an indicative picture of the change in the composition of the disease burden in India. In India, as shown in figure 10, over the last one decade the proportion of NCDs are increasing and the communicable, maternal, neonatal and nutritional causes (referred to as “MDG conditions”) are reducing. In 2002, the expectancy of life at birth was 63.37, which improved to 64.56 in 2005 and further to 67.38 in 2012, according to World Bank data, and some part of this shift is reflective of the demographic transition, and the resulting ageing population.[xci]
Figure 10: The changing disease composition of India
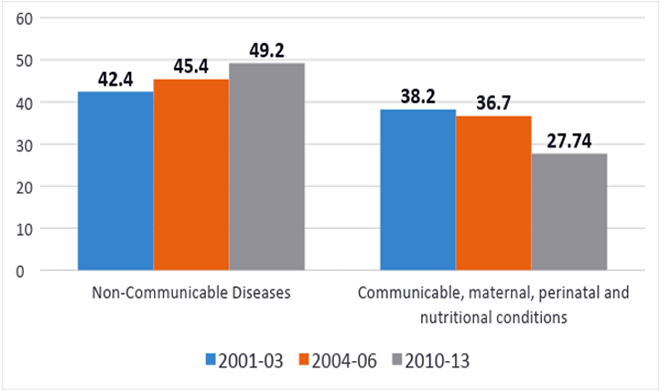
While the national levels across time show a clear trend, there are stark regional differences as well. The absolute levels of “MDG conditions” are still high in the less developed states. The levels are different between the less developed and developed states, but even in the less developed states, the trends are similar. The NCD proportion is growing fast and it is just a matter of time before there is a convergence of NCD numbers across the country (Figure 11). In the interim, however, most of the Indian states have the dual responsibility of having a health system well prepared to handle the preventive, curative, promote and rehabilitative aspects of this double burden.
Figure 11: Regional variations in causes of mortality
It can be argued that as the Indian population ages, an increased proportion of deaths due to NCDs is just a consequence of having a bigger population of the elderly. However, data on the top 10 causes of untimely death[xcii] -of people within the 30-69 age group- shows that the NCD proportions are exceedingly high, as shown in Table 1. Even within the EAG states[6] and Assam, cardiovascular diseases accounted for a high 24.4 percent of all deaths within the 30-69 age group. In other states, cardiovascular diseases accounted for 34.4 percent and the national average was 31.8 percent.
|
Table 1: Top 10 causes of death in age 30-69 years in India (2010-2013) Source: http://www.censusindia.gov.in/vital_statistics/causesofdeath.html |
||||
| Rank | Cause of Death | Deaths (%) | ||
| Male | Female | Person | ||
| 1 | Cardiovascular diseases | 33.4 | 29.2 | 31.8 |
| 2 | Cancers | 8.7 | 12.7 | 10.2 |
| 3 | Respiratory diseases | 7.5 | 8.3 | 7.8 |
| 4 | Digestive diseases | 9.0 | 5.0 | 7.5 |
| 5 | Tuberculosis | 6.9 | 4.9 | 6.1 |
| 6 | Unintentional injuries: Other Than Motor Vehicle Accidents | 4.3 | 4.1 | 4.2 |
| 7 | Ill-defined/ All other symptoms, signs and abnormal clinical and laboratory findings | 3.0 | 5.4 | 3.9 |
| 8 | Motor Vehicle Accidents | 5.2 | 1.6 | 3.8 |
| 9 | Genito-urinary diseases | 3.8 | 3.6 | 3.8 |
| 10 | Diarrhoeal diseases | 2.7 | 4.6 | 3.4 |
| All Other Remaining Causes | 15.6 | 20.5 | 17.4 | |
| Total | 100.0 | 100.0 | 100.0 | |
It is clear that in both developed and less developed states, a shift is happening towards NCD conditions in terms of the overall burden. However, since most of the “MDG conditions “also happen to be diseases and conditions of the poor, completely reorienting the health system to address NCDs will throw up questions of equity and ethics.
|
Table 2: Top three causes of mortality (2001-03 and 2010-13) Source: http://www.censusindia.gov.in/vital_statistics/causesofdeath.html |
||||||
| EAG + Assam | 2001-03 Rank | 2010-13 Rank | Other States | 2001-03 Rank | 2010-13 Rank | |
| Cardiovascular diseases | 1 (12.9 %) | 1 (15.6 %) | Cardiovascular diseases | 1(23.9%) | 1 (27.5%) | |
| Diarrheal diseases | 2 (11.0%) | 5 ( 7.8%) | Respiratory diseases | 2 (8.7%) | 3 (7.3%) | |
| Respiratory infections | 3 (8.8%) | 6 (5.4%) | Cancers | 3 (7.1%) | 4 (7.0%) | |
While cardiovascular diseases retain the top slot with an increased proportion of deaths, the ranks of diarrhoeal diseases and respiratory infections have gone down considerably in the EAG states and Assam (See Table 2). In the other states too, the proportion of deaths due to cardiovascular diseases is rapidly increasing.[xciii]
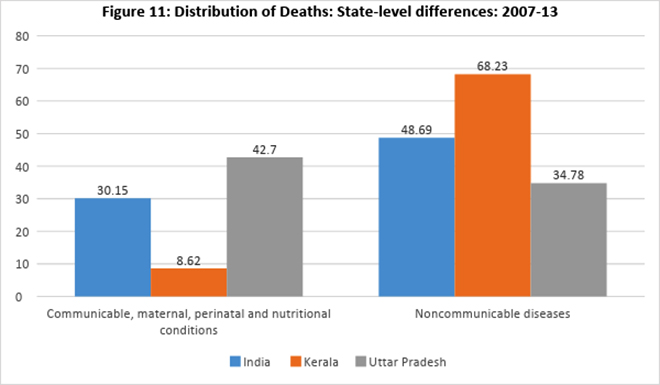
Given the stark inter-state variations in malnutrition and morbidity burdens, national level averages are of limited significance to informing policy. This is seen in the distribution of deaths by major cause groups (2007-2013). In the following example, major causes of deaths are explored across the national average, state average for UP and state average for Kerala. Both the states are far away from the national averages. According to the NITI Health Index which ranked the larger Indian states according to their health system performance, UP is ranked last and Kerala is ranked first.[xciv] The MDG conditions leads to just 8.62% deaths in Kerala whereas they cause 42.7% deaths in UP. NCD conditions cause 2/3rds of all deaths in Kerala, but only one-third in UP (Figure 12). The India average is right in between these two somewhat representative states of the ongoing epidemiological and nutritional transition, and hence, it has only a very limited significance in driving sub-national policy.
Figure 12: Distribution of deaths: State level differences (2007-13)
Most big states for which data are available had cardiovascular diseases as the leading cause of death. Tamil Nadu, Kerala and Karnataka all have relatively higher life expectancies and have Diabetes Mellitus as one of the top ten causes of death. Meanwhile, Andhra Pradesh, Assam, Bihar, Chhattisgarh, Delhi, Gujarat, Haryana, Jharkhand, Maharashtra, Odisha, Rajasthan, UP, Uttarakhand and West Bengal have Tuberculosis as among the top causes of death. Interestingly, nine percent of all deaths in Odisha are because of Malaria. Despite these wide variations, for children between 0-4 years of age, prematurity & low birth weight still remain the top causes of death across developed as well as less developed states, and urban and rural areas. [xcv]
Situation specific health and nutrition policy, with at least district level tracking of outcomes, which will allow for mid-course correction, will be the major development challenge of India in the coming decades.
Assessing the readiness of India’s healthcare system
An earlier version of the National Health Policy had articulated the dilemmas of India’s healthcare delivery system well. [xcvi] It found that all the disease conditions for which national programmes provide universal coverage account for less than 10 percent of all mortalities and only for about 15 percent of all morbidities. Similarly, the National Health Programmes that address infectious diseases at the sub-center and PHC levels represented only less than six percent of all morbidities and about 25 percent of all infectious diseases.[xcvii] In other words, even when the balance of the overall disease burden is shifting from communicable diseases to NCDs, over 75 percent of communicable disease conditions have not been part of any existing national programmes. Overall, communicable diseases and maternal and neonatal ailments contribute to 24.4 percent and 13.8 percent of the country’s disease burden, respectively. NCDs (39.1 percent) and injuries (11.8 percent) constitute the bulk of India’s disease burden, although National Health Programmes for NCDs are limited in coverage and scope. 80
Early signals from the current government had suggested that a focus on the MDG conditions and undernutrition will continue, and at a larger scale. India’s Economic Survey 2015-16 had made a compelling case for more government spending in the relatively low-cost maternal and early-life health and nutrition programmes as they offer high returns on investment. The survey observed that already halfway through its demographic dividend, India would need a healthy and educated population to take full advantage of its potential.[xcviii] Government of India’s drastic policy initiatives on prices of cardiac stents and cancer medicines is an indirect acknowledgement of the need to make significant re-alignments in health policy.[xcix]
Health and Wellness Centers (HWC), currently being rolled out as part of the Ayushman Bharat initiative is an important step of diversification of the health system’s focus towards non-communicable conditions. As many as 1.5 lakh HWCs will be set up across the country to bring the healthcare system closer to the people. These centres—to be set up by 2022—will provide comprehensive primary healthcare, including for non-communicable diseases and maternal and child health services. These centres will also provide free essential drugs and diagnostic services. They will offer mental health services, vaccinations against select communicable diseases, and screening for hypertension, diabetes and some cancers. A task force set up by the Union government in 2014 to provide a report on the rollout of comprehensive primary health care recommended implementing HWCs. However, the report also reminded that the credibility of a health and wellness centre would rest on the availability of essential medicines and diagnostics for a wide range of health care needs.[c]
The WHO has acknowledged the policy challenge resulting from the rising double burden of malnutrition and has rolled out a Strategic Action Plan to Reduce the Double Burden of Malnutrition in the South-East Asia Region 2016–2025. The plan encourages comprehensive implementation of policy actions that deal simultaneously with undernutrition and overnutrition. The draft action plan was developed through a series of four consultations held in New Delhi over 2015 and 2016. [ci] India has an array of programmes (presented in Box-1) from multiple ministries/sectors on improving maternal and child nutrition but lags behind on convergence and political commitment.[cii]
| Box-1: Multisectoral programmes on maternal & child nutrition in India |
| India is the first country to develop a monitoring framework for prevention and control of NCDs.[ciii] In March 2017, India became the first country to adapt the World Health Organization guideline for the nutritional care and support of TB patients.[civ] Similar guidelines already exist for AIDS patients.[cv] The challenge of nutrition figures prominently in the draft National Strategic Plan for TB Elimination (2017-2025) as well. [cvi] The Working Group on Addressing Consumption of Foods High in Fat, Salt and Sugar (HFSS) and Promotion of Healthy Snacks in Schools of India in 2015 tried to address the triple burden of malnutrition where undernutrition, micronutrient deficiencies and excess intake of calories by preparation of guidelines.[cvii] The Food Safety and Standards Authority of India (FSSAI) has already issued the draft guidelines on fortification for five food items. [cviii]The need for multi-sectoral action to prevent and reduce the undernutrition prevalence as well as anaemia has been acknowledged by the Government of India and a Multisectoral Nutrition Programme to Address Maternal and Child Undernutrition has been rolled out in 200 high-burden districts, as part of the National Nutrition Mission. [cix] National Nutrition Mission (POSHAN Abhiyaan) is a flagship programme of the Ministry of Women and Child Development (MWCD), Government of India, which ensures convergence with various programmes i.e., Anganwadi Services, Pradhan Mantri Matru Vandana Yojana (PMMVY), Scheme for Adolescent Girls (SAG) of MWCD Janani Suraksha Yojana (JSY), National Health Mission (NHM), Swachh-Bharat Mission, Public Distribution System (PDS), Department Food & Public Distribution, Mahatma Gandhi National Rural Employment Guarantee Scheme (MGNREGS) and Ministry of Drinking Water & Sanitation. The Poshan Abhiyaan is being rolled out in a phased manner across the country, beginning 2017-18 with 315 districts, followed by 235 districts in 2018-19 and remaining districts by 2019-20. The goals of Poshan Abhiyaan are to achieve improvement in nutritional status of children from 0-6 years, adolescent girls, pregnant women and lactating mothers. The programme will aim to reduce stunting, undernutrition, anemia and reduce low birth weight by 2%, 2%, 3%, and 2% yearly respectively and bring down stunting to 25% by 2022 from 38.4% (NFHS 4).[cx] |
The success of the Poshan Abhiyaan will lie in its effective implementation and how it reaches the vulnerable population it is looking to target like adolescent girls, pregnant and lactating women. This requires political will and convergence with the other key sectors specially the health sector. Counselling on nutrition is the key to bring about behavior change and every opportunity to be tapped from the time women attends the antenatal clinic through her delivery to home visits. This calls for integration of the key ministries handling of health and nutrition and repositioning nutrition programmes for accelerating improvement in maternal and child health and nutrition. [cxi]
For India to meet the SDG target on malnutrition requires ninety-percent coverage of women and children in the first one thousand days of life with evidence-based Essential Nutrition Interventions (ENIs) and maternal-child health services. This has to be complemented with nutrition sensitive interventions like improving access to diversified food, improved sanitation and women’s empowerment.[cxii]
In addition, with the aim of strengthening the ICDS systems and convergent actions for improved nutrition outcomes, India rolled out the ICDS Systems Strengthening & Nutrition Improvement Program (ISSNIP) with support from the World Bank in 2012. The objective was to supplement and provide value addition to the ICDS and facilitate states/districts to experiment and innovate more effective approaches to achieve early childhood education and nutrition outcomes. The ISSNIP is implemented in 162 districts having high prevalence of undernutrition across eight states.[cxiii] There are interesting multi-sectoral initiatives at the state level and Karnataka Multisectoral Nutrition (KMN) Pilot is one of them. [cxiv] The objective of the KMN is to increase utilization of nutrition-improving services by under-three children, adolescent girls and pregnant and nursing women from poor households in the target areas. Interestingly, neither the department of health and family welfare nor the department of women and child development, but the department of rural development and panchayati raj, and the zilla parishads implement the project. [cxv] Initiatives trying to address nutritional challenges by ministries other than the Ministry of Women and Child Development or MoHFW are not one-off. Intersectoral convergence of initiatives is important for scaling up essential maternal and child health interventions. Ensuring better coordination among ministries will ensure that nutrition services reach the most deprived communities. A detailed note on such initiatives is given in Annexure 3.
It is estimated that in 40 years’ time, 80 percent of the world’s elderly population will be in low and middle-income countries, 200 million of them being Indians.[cxvi] The reorientation of the primary care infrastructure of India to adapt to the changing epidemiological needs of the population is a policy imperative. As most NCDs have their contributing factors intertwined with dietary practices, physical inactivity, tobacco use, harmful use of alcohol, high blood pressure, raised blood glucose, overweight and obesity, the need for cross-sectoral collaboration is well acknowledged in policy documents. The national action plan and monitoring framework for prevention and control of NCDs maps possible ministries/sectors for such initiatives and diet and physical inactivity figure prominently, as shown in the Figure 13.
Figure 13: Examples of cross-sectoral government engagement to reduce risk factors, and potential health effects of multi-sectoral action

Irrespective of these initiatives and plans, which are at the nascent stage at best, India’s health system is geared more towards addressing maternal/child health conditions and partly communicable diseases, which still remain formidable challenges to the poorer states. Nevertheless, there have been some efforts to reconcile the task of addressing the twin challenges of disease and malnutrition. Acknowledging the role of the health sector to address malnutrition, during 2006, a Working Group on Integrating Nutrition with Health was formed under the chairpersonship of Secretary, Ministry of Women and Child Development. This was done as part of the preparation for the eleventh five-year plan.
The working group acknowledged that despite an increase in economic productivity and enhanced efforts in terms of nutrition interventions, significant improvements in nutritional status have not been forthcoming. In view of the huge burden of morbidity and mortality directly linked to malnutrition (undernutrition as well as overnutrition), the working group recommended treating malnutrition as the number one public health problem in the country, and putting a greater emphasis on nutrition action at all levels of the health sector.[cxvii] Other recommendations included bringing nutrition issues centrestage in terms of social policy, establishing a nutrition information system in the country, addressing infant and young child nutrition more effectively to ensure child survival, promoting growth and development on the one hand and preventing diet related chronic diseases on the other, addressing micronutrient deficiencies in a holistic manner adopting a five-pronged strategy with due focus on dietary diversification, nutrient supplementation, food fortification, horticultural interventions and public health measures, and finally, creating a climate of nutritional awareness in the country utilising all available channels of communication.[cxviii]
A multi-stakeholder consultation hosted by the Planning Commission in 2010 had discussed policy options to address India’s nutrition challenges. The group of experts who explored possible institutional arrangements at national/state/district/local levels led by senior bureaucrats recommended that at both the national as well as the state level, there needs to be a supra-ministerial set-up to help allocate nutrition to a single entity, rather than the fragmented way in which it is handled currently.[cxix]
In parallel to the high-level policy conversations on integrating health and nutrition, some public-private partnerships at the state level have been exploring these possibilities at the grass-root. A project involving development agencies and state governments titled Integrated Nutrition and Health Project (INHP) attempted in many Indian states an approach of localizing nutrition and health interventions through volunteer change agents. Nutrition and Health Days (NHD) were introduced in villages where the frontline workers of both health and nutrition programmes provided services including immunizations, antenatal care, take-home supplementary food, micronutrient supplements, and health talks[cxx]. The Dular Project used a similar approach in Bihar and Jharkhand where trained local resource-persons helped improve nutrition, childcare, and hygiene in the villages. NHDs have been replicated across the country and they now form part of NRHM under the name Village Health and Nutrition Day (VHND). [cxxi]
A maternal and child care entitlement card was jointly introduced by ICDS and NRHM in March 2010, signifying the strategic focus on reaching mothers and children under three years of age and a holistic approach to child health and development integrating nutrition and health. [cxxii] However, these efforts of integrating health, nutrition and other sectors remain fragmented and often limited within the narrow confines of a maternal and child health approach. A focus on mothers and children may be necessary as malnutrition is attributed to more than one-third of the under-five deaths in India.[cxxiii] Still, a broader level of integration transcending the RCH sector is necessary, given the nature of the epidemiological as well as nutritional transitions in the country whereby “MDG conditions” are declining fast as the source of the dominant burden.
A study exploring integration of nutrition and health by researchers Nirupam Bajpai and Ravindra H. Dholakia observed that the ICDS requires strengthening and restructuring with a strong convergence with NRHM and the Total Sanitation Campaign (TCS). They added that ICDS should focus on pregnant and breastfeeding mothers and children under three, and there is a need for ministries associated with health, drinking water supplies, sanitation, school education, agriculture, and food and public distribution to integrate a concrete nutrition focus to their programming. [cxxiv] As a step forward the Government of India during the 12th five year plan proposed strengthening and restructuring of ICDS Scheme to improve the services under ICDS. [cxxv] ICDS restructuring aims to reduce child undernutrition, enhance early development outcomes, improve care of girls and women, and reduce anemia prevalence. All this will be in convergence with Health and NRHM.[cxxvi] While the formal collaboration between the frontline workers of MoHFW and MWCD – ASHA (NRHM) and the AWW (ICDS) – is largely limited to the Village Health and Nutrition Days (VHND), there is a need to deepen the linkages in order to improve the integration of the health and nutrition sectors. The study[7] also recommended an Accredited Nutrition Activist (ANA) per every 1000 people in the country, who would serve as a joint appointment between ICDS and NRHM, as an intermediary between the AWW and ASHA, focusing on the outreach needs of the AWC. [cxxvii]
A recent analysis of the ICDS[cxxviii] has found increase in the utilisation of services but gaps exist in in terms of implementation, population size, diversity, and community awareness. The study calls for scaling up the programme with effective implementation at the sub national level and to reach the neglected and marginalized group.
All the above emphasise on multisectoral convergence to tackle the burden of malnutrition. This has been highlighted in a review[cxxix] on India’s national policy and strategic plan, to strengthen the policy environment. It suggests joint implementation of the various schemes under different ministries for improving nutritional needs of children, adolescent girls, and pregnant women. The need to correctly position the nutrition programme within the National Health Mission and universalising Essential Nutrition Intervention (ENI), by the Ministry of Health and Family Welfare has been emphasised in a working paper. [cxxx]
The way forward: Restructuring at the centre, with sub-national solutions
India has come a long way from the 1970s when, as popularly enunciated, “over 70 per cent families continued to be poor; even though their expenditure on food was 70 per cent of their total household expenditure, 70 per cent of children were still under-nourished”.[cxxxi] However, the old problems remain and the health system remains only partly equipped to deal with the emerging problems. A realignment of the health system is required, which currently has a limited focus on reproductive / child health and communicable diseases through vertical interventions. While the existing focus on “MDG conditions” need to be consolidated and expanded to underserved populations, more focus on preventive and promotive health needs within a comprehensive framework and customized interventions at sub-district levels is needed.
The increased policy attention to the MDGs since 2000 has meant greater progress on maternal and child health related indicators, but the new challenges need a fresh approach, building on the gains of the MDG era. The SDGs built on the success of MDG are a universal call to action to end poverty, protect the planet and ensure that all people enjoy peace and prosperity. India has played an important role in shaping the SDGs and effectively committed to achieving them. [cxxxii] The imperative is a well-integrated nutrition and health sector. It calls for the promotion of universal access to all direct nutrition actions and relevant health actions impacting nutrition through health programmes.
With the high and increasing level of mutual interaction between malnutrition and disease at both ends of the spectrum, the nutrition and health sectors cannot afford to work in silos, if India is to achieve its health and nutrition goals. There are already policy conversations and action on the ground, but much more can be done. Nutrition is certainly a policy issue going beyond women and children alone, as the country moves away from the selective emphasis of the MDGs to the more comprehensive SDGs. The increasing burden of communicable diseases as well as overnutrition are leading to complex policy challenges: for example, diabetes and hypertension prevalence are higher among men than women, although more women are overweight/obese.[cxxxiii]
Interestingly, efforts by Government of India to address the dual burden of malnutrition saw some seemingly ad-hoc division of responsibilities. For example, the Twelfth Plan document suggested that while overnutrition will be screened by the health system, ICDS and health will be responsible for screening for undernutrition.[cxxxiv] While NRHM already has some nutrition related interventions iron supplementation, researchers have suggested that given that maternal and child undernutrition is a common cause of infant and child mortality, more efforts in the form of multi-programme coordination on nutrition is needed to break the link between undernutrition, disease, and child mortality, and overcome the fragmented nature of existing policy efforts.[cxxxv]
Within the framework of maternal and child nutrition, convergence will result in improved coverage, a low lying fruit, given that the health system is able to reach out to a wide majority of population currently through ANC coverage, institutional deliveries and immunisation efforts to strengthen governance and accountability. Experts observe that with the recent policy of introducing the second dose of measles in the second year of a child’s life, the health sector is expected to reach not only all children 0–1 years old, but all children in the 0–2 year’s age group. [cxxxvi] Therefore, leveraging the existing health and family welfare infrastructure to streamline the delivery of nutrition services may be something to consider, given that more than one-third of Indian children are still underweight and almost two-third are anaemic. This was done in Bangladesh in the last decade, utilising the window of opportunity to intervene within the first 1,000 days of life, where antenatal care (ANC) and management of sick under-five children were identified by the National Nutrition Services (NNS) as critical health service delivery contacts.[cxxxvii]
However, optimal coordination between the nutrition and health programming remains absent in India. While MWCD has a broader mandate of addressing the glaring gender disparities and child protection across sectors, maternal and child nutrition has become the predominant policy concern. Many of the central level MOUs of nutrition related interventions with external agencies are with MWCD, irrespective of the implementing agencies at the state level. A quick analysis of WCD budget over the years shows that most of the budget that the ministry spends is for nutrition – with the large ICDS programme absorbing 83 percent (2016-17), and 76 percent (2017-18) of overall outlay -and hardly anything being spent on the core mandate.[cxxxviii] The reduction of the proportion in 2017-18 was because of the allocation of INR 27 billions to the Maternity Benefit Programme. If that amount is excluded, the proportion allocated to ICDS had in fact increased to over 86 percent in 2017-18. [cxxxix] In 2018-19, out of a total outlay of INR 247 billions, INR 232 billions were spent on ICDS alone.
This leads to a more important question: why is it that gender is only given an incidental importance? The transition of the Department of Women and Child is a case in point- it was first hosted in the Ministry of Social Welfare and later in the Ministry of HRD during the United Nations Decade for Women (1975-85), then became an independent ministry in 2006, but still piggybacking on the policy focus on mother and child nutrition. [cxl] The instrumental role the framework gives to women is noteworthy, where the primary aim is development of the child. Ministry documents related to ICDS, a scheme constituted right after the National Policy for Children of 1974 read: “Women between 15 and 45 years have also been brought within the ICDS ambit, since the mother plays the key role in the overall development of the child. Therefore, any scheme that aims at the welfare of the child may logically include the welfare of the mother, particularly when pregnant or nursing.” [cxli]
Perhaps it is time to transcend the unitary focus on mother and child nutrition, and SDGs give us an opportunity to reallocate responsibilities and arrive at a more optimal solution. India currently has 1,55,708 functioning sub-centers. [cxlii] There are 1,98,356 female ANMs and 55,657 male ANMs in position. In addition, 8,70,089 ASHAs work in the villages[cxliii], and they are often the first point of contact for a majority of the Indian population. At the same time, India has 13,56,569 operational AWCs across the country reaching out to 949.39 lakh beneficiaries both children and mothers. [cxliv]
A formal integration of this infrastructure can mean enhanced access to both health as well as nutrition services to the currently underserved populations. There is history of collaboration with MWCD and MoHFW at multiple layers of governance on the issue of nutrition.[cxlv] Now, there is an opportunity to take it to the next level, and start a national conversation on the feasibility of a new Ministry of Health and Nutrition, like Sri Lanka has done. Such a conversation, unlike earlier, can be informed by robust evidence at the sub-state levels. The ongoing National Family Health Survey -5 (NFHS) holds great promise for customised solutions at the sub-state level. NFHS in India is one of the only two so far from the global DHS team – other being Kenya – that have collected data at the lowest administrative level.[cxlvi]
Earlier policy documents and studies on ICDS state that the health services provided by ICDS offered a link between the village and the Sub Centre.[cxlvii] This description matches exactly with the work responsibility of ASHA, a cadre which has helped expand the health care coverage across the country.[cxlviii] It is time to consider consolidating the gains, and amplify the reach of existing health and nutrition delivery systems with increased investments at the frontline to offer enhanced services that help deal with the maternal and child health and nutritional conditions, communicable as well as the non-communicable diseases through a comprehensive primary health care approach as articulated in the National Health Policy 2017. Anganwadi Centers can work in collaboration with the planned network Health and Wellness Centers – upgraded Sub Centers and Primary Health Centers—across the country with the introduction of a health worker focusing on nutrition in every village who works in tandem with other ground level health and nutrition functionaries.
The authors would like to acknowledge two anonymous referees for their valuable inputs on an early draft of this paper and Vasundhara Singh for her help with references.
ANNEXURE
Annexure 1: Percentage point difference between underweight and overweight women and % of women with very high blood sugar level
Annexure 2: Percentage point difference between underweight and overweight men and % of men with very high blood sugar level
Annexure 3: Multisectoral initiatives to address nutritional challenge
UNICEF India in collaboration with National Ministry of Rural Development and Panchayati Raj has started the Swabhimaan multi-sector demonstration programme in 2016 across Bihar, Chhattisgarh and Odisha as part of National Rural Livelihood Mission. The aim of the programme is to test an integrated multi-sectoral strategy to improve girls and women’s nutrition before conception, during pregnancy and after birth in India.[cxlix]
The SABLA scheme under MWCD, launched in 2010 using the platform of ICDS Scheme through Anganwadi Centers (AWCs) is specially designed for providing life skills, supplementary nutrition and basic health check-up facilities for the out of school adolescent girls, in .[cl] The Beti Bachao Beti Padhao scheme (BBBPS) under the same ministry has a target to improve the nutrition status of girls – by reducing the prevalence of undernourishment and anemia among girls under 5 years of age (from NFHS 3 levels). [cli] A recent initiative from MoHFW with a potentially big impact on undernutrition is the National Deworming Day, initiated in 2015 to address the risk from Soil Transmitted Helminths (STH). It is the world’s largest deworming programme and currently covers 340 million children across 36 states/ UTs.[clii]
Given the fact that the probability of dying during the most productive years (ages 30-70) from one of the four main NCDs is a staggering 26% in India, the government launched the National Programme for the Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). Analysts have observed it as a necessary – but not sufficient – programme to reduce NCDs’ national burden.[cliii] Noting the quantum of the challenge, MoHFW has augmented NPCDCS in 100 districts to include universal screening of diabetes and hypertension as well. According to the DGHS, the aim is to expand the reach and coverage of the programme by integrating early detection and management of hypertension and diabetes into the service package at the most peripheral levels. So far, more than 65 million people have been screened, and a cancer-screening programme is to be launched soon. [cliv]
As part of this initiative, a set of guidelines for population level screening and MoHFW published early detection for major NCDs- diabetes, hypertension and three common Cancers- in 2017. This set of guidelines, according to secretary, MoHFW, is the first of a series, which will enable offering services linked to early detection and management for non-communicable diseases at the sub- center level. [clv] This is in line with the vision shared in the NHP 2017, whereby existing facilities will be converted into ‘Health and Wellness Centers’, providing comprehensive primary health care services at the most peripheral levels.[clvi] As of February 2019, 8030 HWCs are operational across the country.[clvii]
The Ministry of Health and Family Welfare Mothers launched Mother’s Absolute Affection[clviii] (MAA) programme in 2016 for promoting breastfeeding. It is aimed to create an enabling environment to ensure that others, husbands and families receive adequate information and support for promotion of breastfeeding. The goal of the MAA Programme is to enhance optimal breastfeeding practices, which includes early initiation of breastfeeding within one hour of birth, exclusive breastfeeding for the first six months, and continued breastfeeding for at least two years, along with feeding of safe and appropriate nutritious food on completion of six months. Improved breastfeeding is a proven intervention to combat malnutrition in the 1000 days critical window of opportunity.
Endnotes
[1] Type of malnutrition characterised by overweight or obesity.
[2] Low height-for-age.
[3] Low weight for height.
[4] Children given something other than breastmilk during the first three days of life.
[5] Children aged 6-23 months are considered to be fed a minimum acceptable diet if they receive breastmilk, other milk or milk products, are fed the minimum dietary diversity and are fed the minimum meal frequency
[6] Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Odisha, Rajasthan, Uttarakhand and Uttar Pradesh.
[7] According to the study, The ANA’s outreach work would focus on a finite list of critical nutrition interventions for: young women, pregnant women, breastfeeding mothers, infants, children under two, children under five, and heads of household.
[i]NCD Risk Factor Collaboration. “Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19· 2 million participants“. The Lancet 387, no. 10026 (2016): 1377-1396.
[ii] World Health Organization. Healthier, fairer, safer: the global health journey, 2007–2017. World Health Organization, 2017.
[iii] Achadi, Endang, Arti Ahuja, Mohamed Ag Bendech, Zulfiqar Ahmed Bhutta, Luz Maria De-Regil, Jessica Fanzo, Patrizia Fracassi et al. Global Nutrition Report: From Promise to Impact: Ending Malnutrition by 2030. International Food Policy Research Institute, 2016.
[iv] Vidya Krishnan, “Fight stunting, says World Bank Chief”. The Hindu, June 30, 2016, National Section.
[v] Von Grebmer, Klaus, Jill Bernstein, David Nabarro, Nilam Prasai, Shazia Amin, Yisehac Yohannes, Andrea Sonntag, Fraser Patterson, Olive Towey, and Jennifer Thompson. 2016 Global hunger index: Getting to zero hunger. Intl Food Policy Res Inst, 2016.
[vi] World Health Organization 2016. “Strategic Action Plan to Reduce the Double Burden of Malnutrition in the South-East Asia Region 2016-2025”.
[vii] National Institution for Transforming India, Government of India (NITI) Aayog. “An overview of sustainable development goals” (2016).
[viii] Sue Desmond-Hellman, “A cost we can’t afford: The human and economic costs of malnutrition and how India can end this scourge”, Times Of India, October 20, 2016, TOI Edit Page.
[ix] Jena, Pratap K., and Baliyeri P. Jeena. “Overnutrition among schoolchildren in India: a review and meta-analysis.” The Lancet Global Health 6 (2018): S25.
[x] Forouzanfar, Mohammad H., Ashkan Afshin, Lily T. Alexander, H. Ross Anderson, Zulfiqar A. Bhutta, Stan Biryukov, Michael Brauer et al. “Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015.” The Lancet 388, no. 10053 (2016): 1659-1724.
[xi] Reddy, K. Srinath. “Global Burden of Disease Study 2015 provides GPS for global health 2030.” The Lancet 388, no. 10053 (2016): 1448-1449
[xii] Global Nutrition Report, 2018.
[xiii] National Family Health Survey 4, 2015-16.
[xiv] National Family Health Survey 4, 2015-16 Factsheet.
[xv] ibid
[xvi] World Bank. “Prevalence of stunting, height for age (% of children under 5)” (2016).
[xvii] ibid
[xviii] Ravi, Shamika, and Ramandeep Singh. “Nutrition in India: Targeting the First 1,000 Days of a Child’s Life.” Available at SSRN 3041157 (2016).
[xix] ibid
[xx] ibid
[xxi] IFPRI. “How Are India’s Districts Doing on Maternal, Infant and Young Child Nutrition? Insights from the National Family Health Survey-4” (2017).
[xxii] Prasad, Vandana, and Dipa Sinha. “Potentials, experiences and outcomes of a comprehensive community based programme to address malnutrition in tribal India“. International Journal of Child Health and Nutrition 4, no. 3 (2015): 151-162.
[xxiii] Victora, Cesar G., Linda Adair, Caroline Fall, Pedro C. Hallal, Reynaldo Martorell, Linda Richter, Harshpal Singh Sachdev, and Maternal and Child Undernutrition Study Group. “Maternal and child undernutrition: consequences for adult health and human capital.” The lancet 371, no. 9609 (2008): 340-357.
[xxiv] World Health Organisation Staff, World Health Organization, and UNICEF. Global strategy for infant and young child feeding. World Health Organization (2003).
[xxv] Rollins, Nigel C., Nita Bhandari, Nemat Hajeebhoy, Susan Horton, Chessa K. Lutter, Jose C. Martines, Ellen G. Piwoz, Linda M. Richter, Cesar G. Victora, and The Lancet Breastfeeding Series Group. “Why invest, and what it will take to improve breastfeeding practices?.” The Lancet 387, no. 10017 (2016): 491-504.
[xxvi] Victora, Cesar G., Bernardo Lessa Horta, Christian Loret De Mola, Luciana Quevedo, Ricardo Tavares Pinheiro, Denise P. Gigante, Helen Gonçalves, and Fernando C. Barros. “Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil.” The Lancet Global Health 3, no. 4 (2015): e199-e205.
[xxvii] Rollins, Nigel C., Nita Bhandari, Nemat Hajeebhoy, Susan Horton, Chessa K. Lutter, Jose C. Martines, Ellen G. Piwoz, Linda M. Richter, Cesar G. Victora, and The Lancet Breastfeeding Series Group. “Why invest, and what it will take to improve breastfeeding practices?.” The Lancet 387, no. 10017 (2016): 491-504.
[xxviii] WHO 2017. Global Nutrition Targets 2025: Policy brief series.
[xxix] Bhutta, Zulfiqar A., Tahmeed Ahmed, Robert E. Black, Simon Cousens, Kathryn Dewey, Elsa Giugliani, Batool A. Haider et al. “What works? Interventions for maternal and child undernutrition and survival.” The Lancet 371, no. 9610 (2008): 417-440.
[xxx] Walia, B. N., S. K. Gambhir, S. R. Sroa, and S. Chaudhary. “Decline in breast feeding practices in urban population of Chandigarh during a decade.” Indian Pediatrics 24, no. 10 (1987): 879.
[xxxi] World Breastfeeding Trends Initiative (WBTi) . Arrested Development. 5th Report of Assessment of India’s Policy and Programmes on Infant and Young Child Feeding (2018).
[xxxii] Przyrembel, Hildegard. “Timing of introduction of complementary food: short-and long-term health consequences.” Annals of Nutrition and Metabolism 60, no. Suppl. 2 (2012): 8-20.
[xxxiii] Collective, Global Breastfeeding, and UNICEF. “Nurturing the health and wealth of nations: the investment case for breastfeeding.” World Health Organization (2017).
[xxxiv] ibid
[xxxv] Sengupta, Angan, Federica Angeli, Thelakkat S. Syamala, Pieter C. Dagnelie, and C. P. van Schayck. “Overweight and obesity prevalence among Indian women by place of residence and socio-economic status: Contrasting patterns from ‘underweight states’ and ‘overweight states’ of India.” Social Science & Medicine 138 (2015): 161-169.
[xxxvi] National Family Health Survey 3 2005-2006.
[xxxvii] Who, Expert Consultation. “Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies.” Lancet (London, England) 363, no. 9403 (2004): 157.
[xxxviii] Misra, Anoop, and Nikhil V. Dhurandhar. “Current formula for calculating body mass index is applicable to Asian populations.” (2019): 3.
[xxxix] ibid
[xl] Misra, Anoop, P. Chowbey, B. M. Makkar, N. K. Vikram, J. S. Wasir, D. Chadha, and Shashank R. Joshi. “Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management.” JAPI57, no. 2 (2009): 163-70.
[xli] Dang, Archana, and J. V. Meenakshi. The nutrition transition and the intra-household double burden of malnutrition in India. No. 725. ADBI Working Paper Series, 2017.
[xlii] Aziz, Nuzhat, Sailaja Devi Kallur, and Praveen Kumar Nirmalan. “Implications of the revised consensus body mass indices for Asian Indians on clinical obstetric practice.” Journal of clinical and diagnostic research: JCDR 8, no. 5 (2014): OC01.
[xliii] Shannawaz, Mohd, and P. Arokiasamy. “Overweight/Obesity: An Emerging Epidemic in India.” Journal of Clinical & Diagnostic Research 12, no. 11 (2018).
[xliv] Sengupta, Angan, Federica Angeli, Thelakkat Sankaranarayanan Syamala, C. P. Van Schayck, and Pieter Dagnelie. “State-wise dynamics of the double burden of malnutrition among 15–49 year-old women in India: how much does the scenario change considering Asian population-specific BMI cut-off values?.” Ecology of food and nutrition 53, no. 6 (2014): 618-638.
[xlv] World Health Organization. “The Double Burden of Malnutrition” Policy Brief (2017).
[xlvi] Bhore, Joseph Chairman. “Report of the Health Survey and Development Committee. Vol. I: Survey.” (1946).
[xlvii] Drèze, Jean, and Amartya Sen. “An uncertain glory: India and its contradictions.” Economics Books (2015).
[xlviii] Prema Ramachandran. Triple Burden Of Malnutrition In India: Challenges And Opportunities India Infrastructure Report (2013).
[xlix] P.M. Kulkarni, “Demographic Transition in India”, Office of Registrar General of India (2014).
[l] Garrett, James L., and Marie T. Ruel. “Stunted child–overweight mother pairs: Prevalence and association with economic development and urbanization.” Food and nutrition bulletin 26, no. 2 (2005): 209-221.
[li] Dang, Archana, and J. V. Meenakshi. The nutrition transition and the intra-household double burden of malnutrition in India. No. 725. ADBI Working Paper Series (2017).
[lii] World Health Organization. “Global report on diabetes: World Health Organization; 2016.” (2017).https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf?sequence=1
[liii]. Plan, Eleventh Five Year. “Document, Government of India. 2006. Report of the Working Group on Integrating Nutrition with Health, Ministry of Women and Child Development.” November. New Delhi. India (2007).
[liv] Indo-Asian News Survey, “India’s TB deaths double in a year from 2.2 lakh to 4.8 lakh; here’s why”, India Today, October 27, 2016.
[lv] Kounteya Sinha, “Malaria kills 20 times more than what govt says”, Times of India, January 11, 2013.
[lvi] Dhirar, Nonita, Sankalp Dudeja, Jyoti Khandekar, and Damodar Bachani. “Childhood Morbidity and Mortality in India—Analysis of National Family Health Survey 4 (NFHS-4) Findings.” Indian pediatrics 55, no. 4 (2018): 335-338.
[lvii] Arnold, Fred, Sulabha Parasuraman, P. Arokiasamy, and Monica Kothari. “Nutrition in India. National Family Health Survey (NFHS-3) India 2005-06.” (2009).
[lviii] Gragnolati, Michele, Caryn Bredenkamp, Meera Shekar, Monica Das Gupta, and Yi-Kyoung Lee. India’s undernourished children: a call for reform and action. The World Bank, 2006.
[lix] ICMR, PHFI. “IHME (2017): “India: Health of the Nation’s States the India State-level Disease Burden Initiative,” Indian Council of Medical Research.” Public Health Foundation of India, Institute for Health Metrics and Evaluation, New Delhi.
[lx] World Health Organization. Strategic Action Plan to reduce the double burden of malnutrition in the South-East Asia Region 2016–2025 (2017).
[lxi] Dandona, Lalit, Rakhi Dandona, G. Anil Kumar, D. K. Shukla, Vinod K. Paul, Kalpana Balakrishnan, Dorairaj Prabhakaran et al. “Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study.” The Lancet 390, no. 10111 (2017): 2437-2460.
[lxii] World Health Organization. “World Malaria Report 2016 (World Health Organization, Geneva).” (2016).
[lxiii] World Malaria Report 2018. Geneva: World Health Organization (2018).
[lxiv] National Health Portal India. “World Malaria Day 2018”.
[lxv] “National Strategic Plan Malaria Elimination in India 2017-2022”, Ministry of Health and Family Welfare, Government of India
[lxvi] “In its quest to eliminate malaria, India focuses on Odisha and the tribal states”, World Health Organization, 2018.
[lxvii] World Health Organization. Guidelines for the treatment of malaria. World Health Organization, 2015.
[lxviii] Mahapatra, Ashish, Sabyasachi Mohapatra, Niloy Mitter, Sushree Swagata Dash, Rudra Prasanna Mishra, and Durga Madhab Satapathy. “Malaria and malnutrition co-existence among under-five children of tribal dense regions of Odisha: a community based study.” International Journal Of Community Medicine And Public Health 5, no. 7 (2018): 3024-3028.
[lxix] Jones, Kelsey DJ, and James A. Berkley. “Severe acute malnutrition and infection.” Paediatrics and international child health 34, no. sup1 (2014): S1-S29.
[lxx] Sama- Resource group for women and health, “From the margins to the centre- A study on the health inequities among the tribal communities in selected districts of Chhattisgarh, Jharkhand and Odisha”, National Human Rights Commission (2018)
[lxxi] Monteiro, Wuelton Marcelo, Márcia Araújo Alexandre, André Siqueira, Gisely Melo, Gustavo Adolfo Sierra Romero, Efrem d’Ávila, Silvana Gomes Benzecry, Heitor Pons Leite, and Marcus Vinícius Guimarães Lacerda. “Could Plasmodium vivax malaria trigger malnutrition? Revisiting the Bradford Hill criteria to assess a causal relationship between two neglected problems.” Revista da Sociedade Brasileira de Medicina Tropical 49, no. 3 (2016): 274-278
[lxxii] Das, D., R. F. Grais, E. A. Okiro, K. Stepniewska, R. Mansoor, S. Van Der Kam, D. J. Terlouw, J. Tarning, K. I. Barnes, and P. J. Guerin. “Complex interactions between malaria and malnutrition: a systematic literature review.” BMC medicine 16, no. 1 (2018): 186.
[lxxiii] Vandana Prasad. Report of the Consultation on Current Advances in Malaria Management and Implications for Malnutrition, Public Health Resource Network (2019).
[lxxiv] Katona, Peter, and Judit Katona-Apte. “The interaction between nutrition and infection.” Clinical Infectious Diseases46, no. 10 (2008): 1582-1588.
[lxxv] Charu Bahri, “More Than One Million TB Patients Lack Adequate Nutrition”, India Spend (2017) .
[lxxvi] Padmapriyadarsini, C., M. Shobana, M. Lakshmi, T. Beena, and Soumya Swaminathan. “Undernutrition & tuberculosis in India: Situation analysis & the way forward.” The Indian journal of medical research 144, no. 1 (2016): 11.
[lxxvii] Sinha, Pranay, Juliana Davis, Lauren Saag, Christine Wanke, Padmini Salgame, Jackson Mesick, C. Robert Horsburgh Jr, and Natasha S. Hochberg. “Undernutrition and tuberculosis: public health implications.” The Journal of infectious diseases219, no. 9 (2018): 1356-1363.,
[lxxviii] Yen, Yung-Feng, Pei-Hung Chuang, Muh-Yong Yen, Shu-Yi Lin, Peing Chuang, Mei-Jen Yuan, Bo-Lung Ho, Pesus Chou, and Chung-Yeh Deng. “Association of body mass index with tuberculosis mortality: a population-based follow-up study.” Medicine 95, no. 1 (2016).
[lxxix] World Health Organization. Healthier, fairer, safer: the global health journey, 2007–2017. World Health Organization, 2017.
[lxxx] Bhargava, Anurag, Madhuri Chatterjee, Yogesh Jain, Biswaroop Chatterjee, Anju Kataria, Madhavi Bhargava, Raman Kataria et al. “Nutritional status of adult patients with pulmonary tuberculosis in rural central India and its association with mortality.” PloS one 8, no. 10 (2013): e77979.
[lxxxi] World Health Organization. Ten years in public health, 2007–2017: report by Dr Margaret Chan, Director-General, World Health Organization. World Health Organization, 2017.
[lxxxii] Anjana, Ranjit Mohan, Rajendra Pradeepa, Mohan Deepa, Manjula Datta, Vasudevan Sudha, Ranjit Unnikrishnan, Lalith M. Nath et al. “The Indian Council of Medical Research—India Diabetes (ICMR-INDIAB) Study: Methodological Details.” Journal of diabetes science and technology 5, no. 4 (2011): 906-914.
[lxxxiii]. Mendis, Shanthi, Pekka Puska, Bo Norrving, and World Health Organization. Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization, 2011.
[lxxxiv] Anjana, Ranjit M., Rajendra Pradeepa, Ashok K. Das, Mohan Deepa, Anil Bhansali, Shashank R. Joshi, Prashant P. Joshi et al. “Physical activity and inactivity patterns in India–results from the ICMR-INDIAB study (Phase-1)[ICMR-INDIAB-5].” International Journal of Behavioral Nutrition and Physical Activity 11, no. 1 (2014): 26.
[lxxxv] ibid
[lxxxvi] Anjana R M, Mohan V. Diabetes and physical activity. Indian J Med Res (2016);143:530-1.
[lxxxvii] ibid
[lxxxviii] Planning Commission. “Report of the Working Group on Disease Burden for 12th Five Year Plan.” New Delhi: Planning Commission of India, Government of India (2011).
[lxxxix] Report of the Working Group on Disease Burden: Non-Communicable Diseases for 12th Five Year Plan (2011).
[xc] Causes of Death Statistics, Office of the Registrar General & Census Commissioner, Ministry of Home Affairs, Government of India.
[xci] “Life expectancy at birth, total (years)”, World Bank (2017).
[xcii] Defined as deaths before the average expectation of life at birth for (2010-14), 68 years.
[xciii] ICMR, PHFI. “Health of the Nation’s States—The India State-Level Disease Burden Initiative. New Dehli: Indian Council of Medical Research.” Public Health Foundation of India, Institute for Health Metrics and Evaluation (2017).
[xciv] Ministry of Health and Family Welfare, World Bank and Niti Aayog. Healthy States, Progressive States- Report on the Ranks of States and Union Territories. (2018).
[xcv] Sample Registration System, Office of the Registrar General & Census Commissioner, India (2011) http://www.censusindia.gov.in/2011-Common/Sample_Registration_System.html
[xcvi] Ministry of Health & Family Welfare. “National Health Policy 2015 Draft” (2014).
[xcvii] ibid
[xcviii] Government of India (2015) Economic Survey 2015-16, Mother and Child.
[xcix] Oommen C Kurian, The Story Of Extortive Prices For Cancer Drugs And Whether The Government Has Done Enough, Bloomberg Quint, April 08 2019.
[c] Oommen C. Kurian. Bankrolling a health care shake-up. Manorama Yearbook. December 2018.
[ci] ibid
[cii] Sheila C. Vir, “Re-examining and re-positioning India’s nutrition programme for accelerating improvements in maternal and child nutrition”, Observer Research Foundation (2017).
[ciii] World Health Organization. “India the first country to develop a monitoring framework for prevention and control of NCDs”.
[civ] Central Tuberculosis Division, Ministry of Health and Family Welfare, Government of India.
[cv] Government of India, Nutrition Guidelines for HIV-Exposed and Infected Children (0-14 Years Of Age), National AIDS Control Organisation (2013).
[cvi] ibid
[cvii] Ministry of Women and Child Development, Government of India. “Report of Working Group on Addressing Consumption of Foods High in Fat, Salt and Sugar (HFSS) and Promotion of Healthy Snacks in Schools of India” (2015).
[cviii] “FSSAI sets up panel to finalise laws on food fortification”, Times of India, February 12, 2017.
[cix] Ministry of Women and Child Development, “Multi-Sectoral Nutrition Programme”, Press Information Bureau, Government of India (2014) and Ministry of Women and Child Development, “National Nutrition Mission (NNM)”, Press Information Bureau, Government of India (2014).
[cx] POSHAN Abhiyan- Scheme for Holistic Nourishment, National Portal of India.
[cxi] ibid
[cxii] ibid
[cxiii] The World Bank. “India: ICDS Systems Strengthening & Nutrition Improvement Program (ISSNIP)”, World Bank.
[cxiv] The World Bank. “India-Karnataka Multisectoral Nutrition Pilot Project” (2014).
[cxv] Veena S Rao, “How to put India ‘on course’ to fight malnutrition, An ongoing mission in Karnataka shows the way to overcome challenges”, Governance Now (2017).
[cxvi] ibid
[cxvii] Plan, Ninth-Five Year. “Report on the Working Group on Integrating Nutrition with Health.” (2007).
[cxviii] ibid
[cxix] Planning Commission, Government of India. “Addressing India’s Nutrition Challenges” (2010).
[cxx] Bajpai, Nirupam, and Ravindra H. Dholakia. “Improving the integration of health and nutrition sectors in India.” (2011).
[cxxi] ibid
[cxxii] Planning Commission. “Twelfth Five Year Plan (2012-2017). Economic Sectors. Vol. II.” (2012).
[cxxiii] National Institute of Public Cooperation and Child Development New Delhi. “Evaluation of Usage of Mother and Child Protection Card by ICDS and Health Functionaries”, (2014).
[cxxiv] Bajpai, Nirupam, Jeffrey D. Sachs, and Ravindra H. Dholakia. “Improving access, service delivery and efficiency of the public health system in rural India“. (2009).
[cxxv] Ministry of Women and Child Development, “Restructuring of ICDS Scheme”, Press Information Bureau, Government of India (2013)
[cxxvi] “Planning Commission. “Report of the Inter Ministerial Group on ICDS Restructuring“. (2011).
[cxxviii] . Chakrabarti, Suman, Kalyani Raghunathan, Harold Alderman, Purnima Menon, and Phuong Nguyen. “India’s Integrated Child Development Services programme; equity and extent of coverage in 2006 and 2016.” Bulletin of the World Health Organization 97, no. 4 (2019): 270.
[cxxix] Vir, Sheila, K. C. Sreenath, Vijayluxmi Bose, Kavita Chauhan, Shivani Mathur, and Subhadra Menon. “National policies and strategic plans to tackle undernutrition in India: A review” (2014).
[cxxx] ibid
[cxxxi] ibid
[cxxxii] ibid
[cxxxiii] ibid
[cxxxiv] ibid
[cxxxv] Ibid
[cxxxvi] ibid
[cxxxvii] Billah, Sk Masum, Kuntal Kumar Saha, Abdullah Nurus Salam Khan, Ashfaqul Haq Chowdhury, Sarah P. Garnett, Shams El Arifeen, and Purnima Menon. “Quality of nutrition services in primary health care facilities: Implications for integrating nutrition into the health system in Bangladesh“. PloS one 12, no. 5 (2017): e0178121.
[cxxxviii] Ministry of Women and Child Development . Annexure – XXIX Annual Report (2017-18). https://wcd.nic.in/sites/default/files/AR-2017-18-Annexures.pdf
[cxxxix] Ministry of Women and Child Development, Government of India . Annual Report (2016-2017) and Ministry of Women and Child Development, “Budget 2017-18”, Press Information Bureau, Government of India (2017).
[cxl] “Department of Women and Child Development”, Ministry of Women and Child Development, Government of India.
[cxli] “Integrated Child Development Services Scheme”, Ministry of Human Resource Development, Government of India (1975).
[cxlii] Government of India, Ministry of Health and Family Welfare, Rural Health Infrastructure (2016).
[cxliii] Government of India, Ministry of Health and Family Welfare, Rural Health Statistics (2017).
[cxliv] “Child Development, Annual Report 2017-2018”, Ministry of Women and Child Development, Government of India (2018).
[cxlv] Government of India, Joint letter by Secretaries of WCD and MoHFW on convergence (2010).
[cxlvi] ibid
[cxlvii] Sinha, Amarjeet. Rallying Round the Child. Centre for Sustainable Development, Lal Bahadur Shastri National Academy of Administration, 1995.
[cxlviii] “Operational Guidelines for ASHA under NRHM”, National Health Mission, Haryana.
[cxlix] United Nations, Documentation on Sustainable Integrated Agriculture & Livestock for Nutrition Institutional Contract for Capacity building agency, UNICEF, 2017.
[cl] Ministry of Women and Child Development, “New Initiatives for Development of Women and Children”, Press Information Bureau, Government of India (2015).
[cli] Beti Bachao Beti Padhao Revised Guidelines (2015).
[clii] “National Deworming Day”, Press Information Bureau, Government of India (2017).
[cliii] Bloom, David E., Elizabeth T. Cafiero-Fonseca, Vanessa Candeias, Eli Adashi, L. Bloom, Lauren Gurfein, Eva Jané-Llopis, Alyssa Lubet, Elizabeth Mitgang, and Akshar Saxena. “Economics of non-communicable diseases in India: the costs and returns on investment of interventions to promote healthy living and prevent, treat, and manage NCDs“. In World Economic forum, Harvard school of Public health. 2014.
[cliv] Ministry of Health and Family Welfare, “Operational Guidelines for Prevention Screening and Control of Common Non-Communicable Diseases: Hypertension, Diabetes, and Common Cancers”, National Institute of Cancer Prevention and Research (2016).
[clv] ibid
[clvi] Government of India, Ministry of Health and Family Welfare, National Health Policy (2017), Page 9.
[clvii] Press Information Bureau, Ministry of Health and Family Welfare, Government of India, 8th February 2019.
[clviii] “Programme for Promotion of Breastfeeding, Operational Guidelines-2016”, Ministry of Health and Family Welfare, National Health Mission.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Oommen C. Kurian is Senior Fellow and Head of Health Initiative at ORF. He studies Indias health sector reforms within the broad context of the ...
Read More +
Dr. Shoba Suri is a Senior Fellow with ORFs Health Initiative. Shoba is a nutritionist with experience in community and clinical research. She has worked on nutrition, ...
Read More +