Introduction
The World Health Organization (WHO) has declared antimicrobial resistance (AMR) as one of the top ten global public health threats facing humanity.[a],1 The main drivers of AMR include misuse and overuse of antimicrobials; lack of access to clean water, sanitation and hygiene; poor infection prevention and control practices in healthcare facilities and farms; poor access to quality and affordable medicines, vaccines, and diagnostics; lack of awareness and knowledge; and weak enforcement of laws.[1],[2] AMR contributes to morbidity, prolongs hospital stay, and increases mortality. The overuse and misuse of antimicrobial agents such as antibiotics—which is one of the biggest drivers of AMR—occur not only at the individual level but also among prescribers (doctors) and institutions (hospitals).
This report seeks to create an understanding of knowledge, attitudes, behaviours, and practices (KABP) related to antibiotics use and antimicrobial resistance at the population-level. KABP studies are used by social scientists to examine highly nuanced issues associated with a problem in a group or community. Their aim is to identify the most common gaps in people’s knowledge and practices, in order to guide policymaking. This report uses a survey, undertaken to assess the awareness levels of individuals visiting a science museum in Kolkata, a metropolitan city in the state of West Bengal. There is evidence that AMR is a significant problem in the city, which would have motivated the Science Museum to host a “superbug exhibition” to educate the public about AMR.
The rest of the report describes the methodology employed by the authors, outlines the key findings of the survey, and analyses the implications to policymaking.
Methodology
The survey was conducted among visitors at an exhibition on antimicrobial-resistant pathogens, organised in January and February 2021 at the Science City Museum in Kolkata in the state of West Bengal. A part of the survey was also conducted with participants in a mobile exhibition awareness campaign across the city.[b] Volunteers at the science museum administered the questionnaire to visitors, who were randomly chosen as they emerged from the last section of the exhibition. The questionnaire was composed in both English and the vernacular, Bengali, the participants were asked to choose which version they wished to use. The questionnaire was brief, comprising 10 questions, and the researchers made sure to write them in simple language in order to facilitate easy participation. (See Annex for a sample questionnaire in English.) Volunteers at the museum explained the survey questions and recorded the answers, whenever it was required.
The authors analysed the data after each response and demographic category was entered manually in a spreadsheet. The proportions were expressed as percentages.
Results
Demographics of Participants
Responses from 613 participants visiting the “Superbugs: The End of Antibiotics” exhibition at the Science City Museum and the mobile tableau were collated during the study period. Approximately two-thirds of the responders (67 percent) visited the Science City Museum and one-third (33 percent) responded after interaction with the museum volunteers at the mobile tableau.
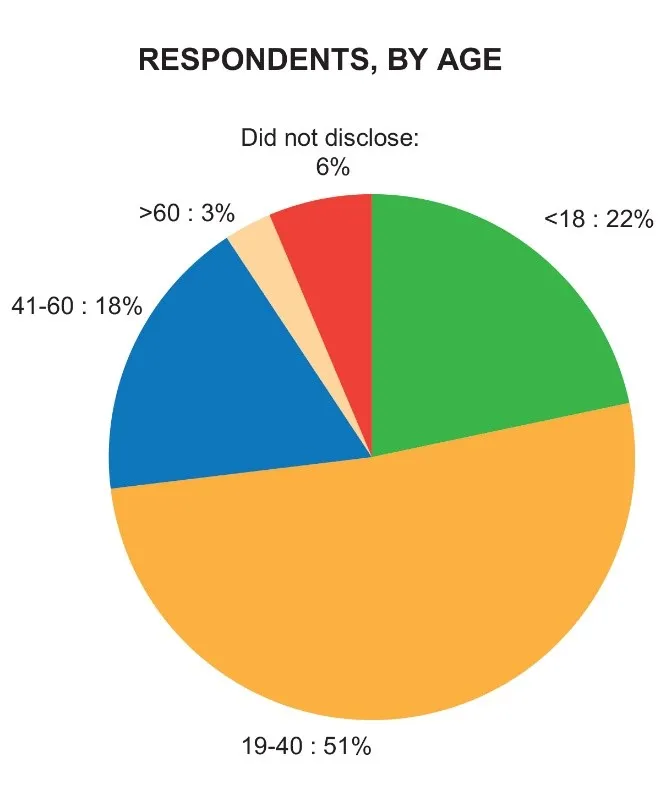
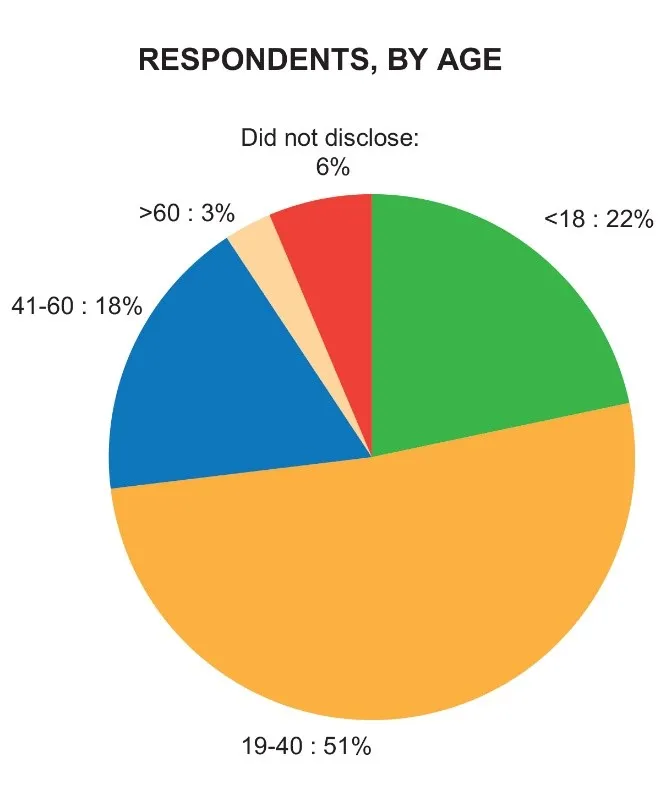
Respondents, by age
A little over 51 percent of the participants were between 19-40 years old; 22 percent were under 18 years; and nearly 18 percent were in the 41-60 age group. Some six percent of the participants did not disclose their age.
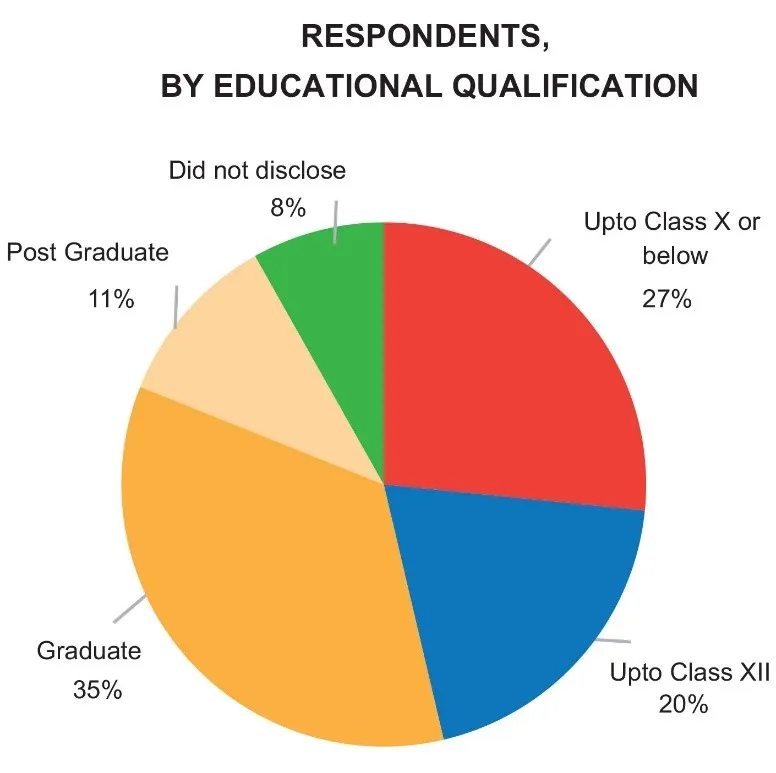
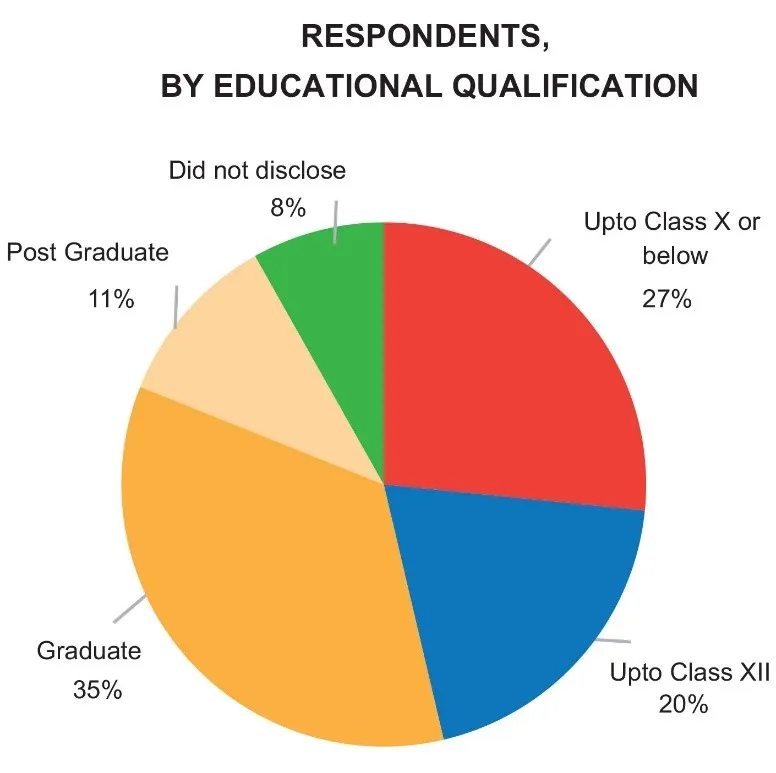
Respondents, by education
In terms of educational qualification, about 35 percent of the respondents were graduates, 11 percent were post-graduates, and 46 percent were high-school students.
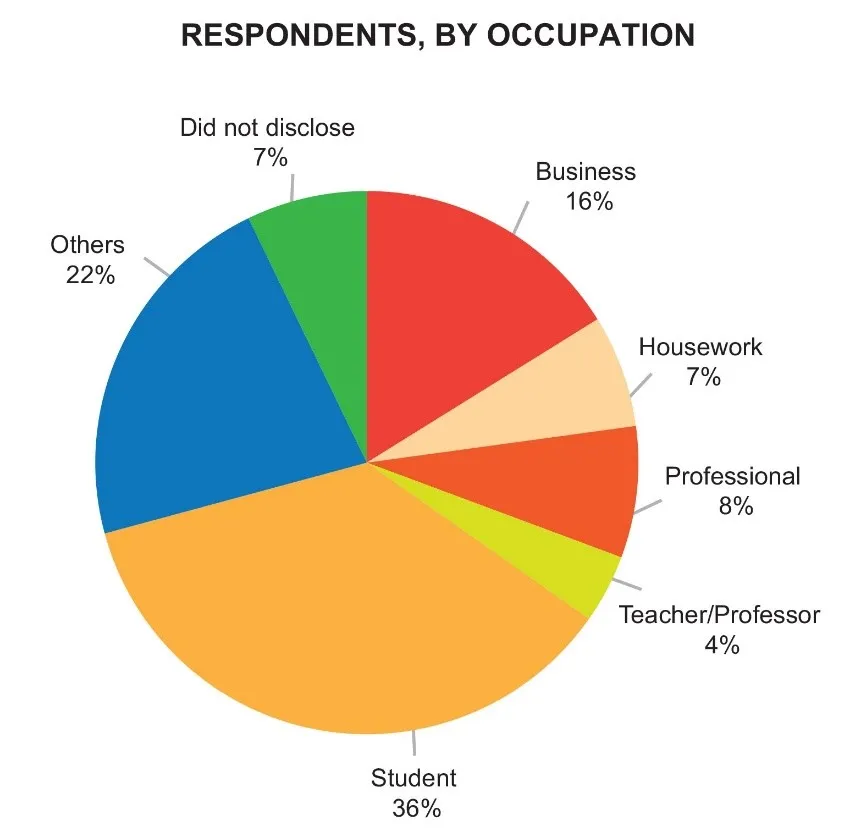
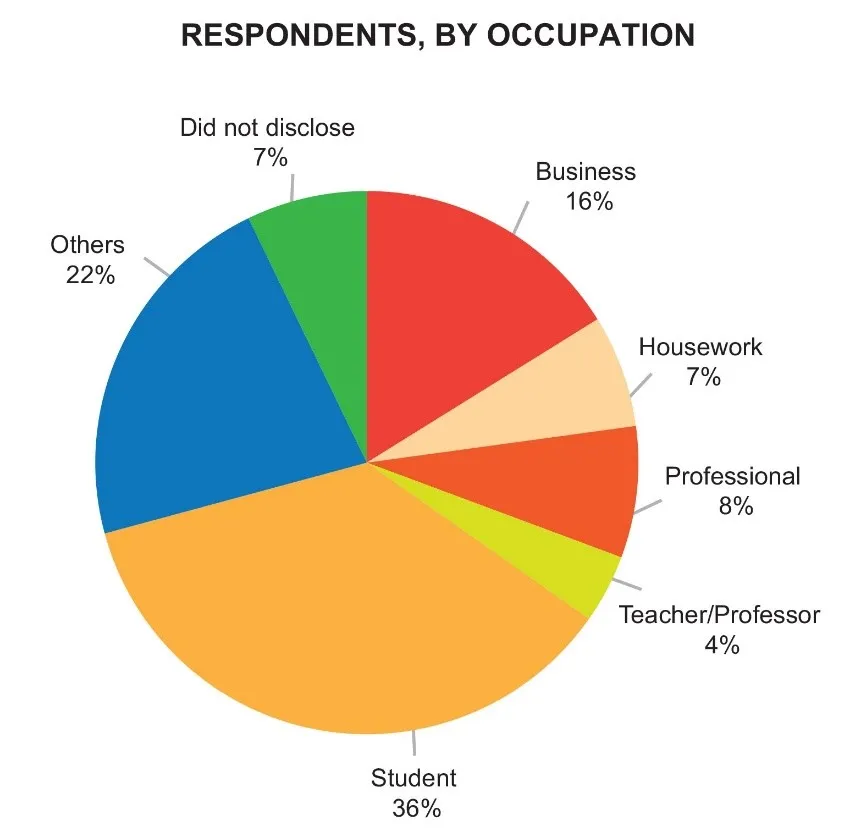
Respondents, by occupation
About 36 percent were students, 12 percent were professional educators (professors or teachers), 16 percent were in business, and 7 percent did housework.
Responses to questions
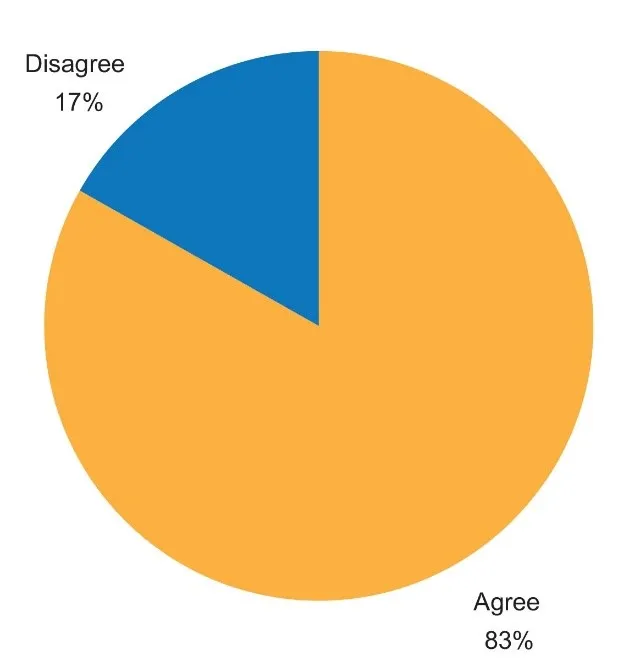
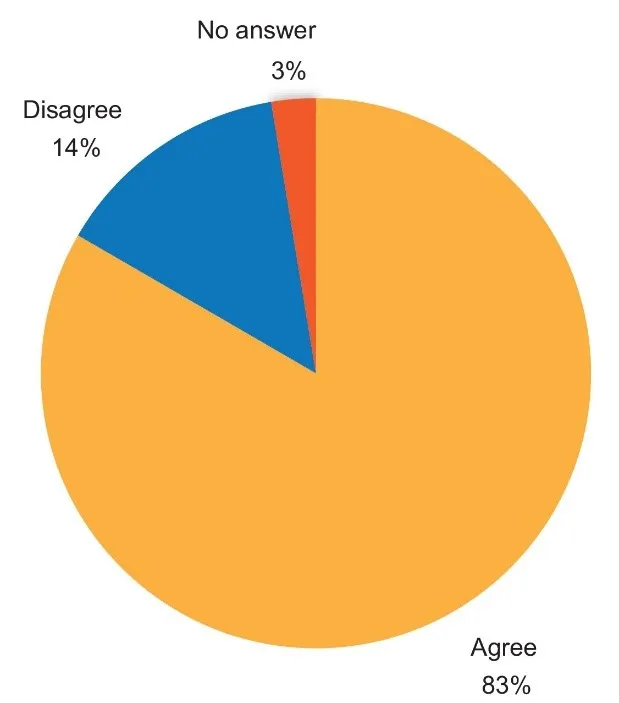
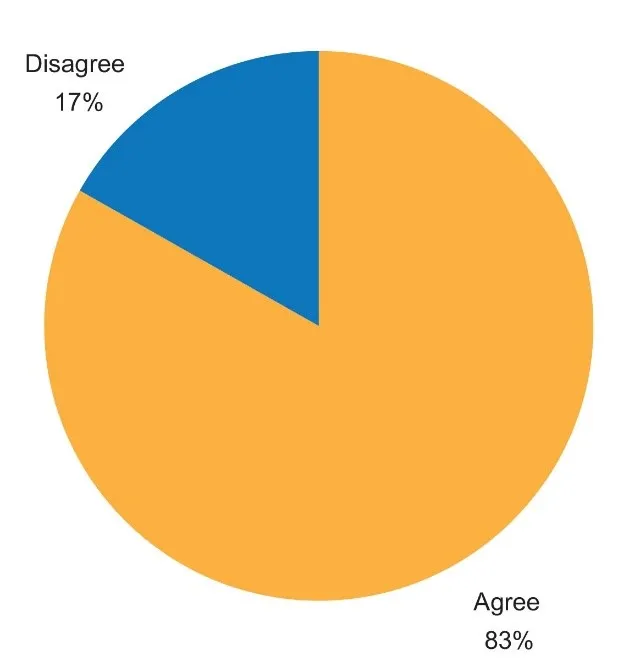
- “Antibiotics should not be purchased or used without the prescription of a registered medical doctor.”
103/613 (17 percent) disagreed.
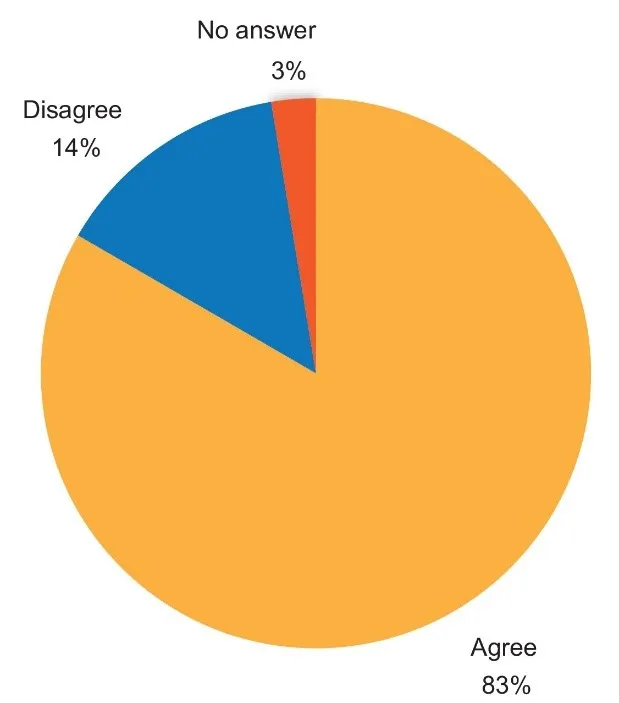
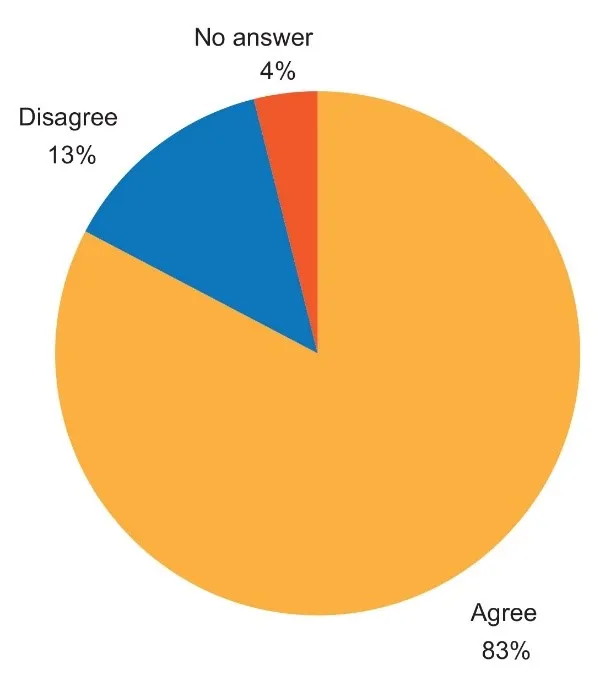
- “Antibiotics are used in animals as well as humans.”
86/613 (14 percent) disagreed and 3 percent of the participants did not provide an answer to the question.
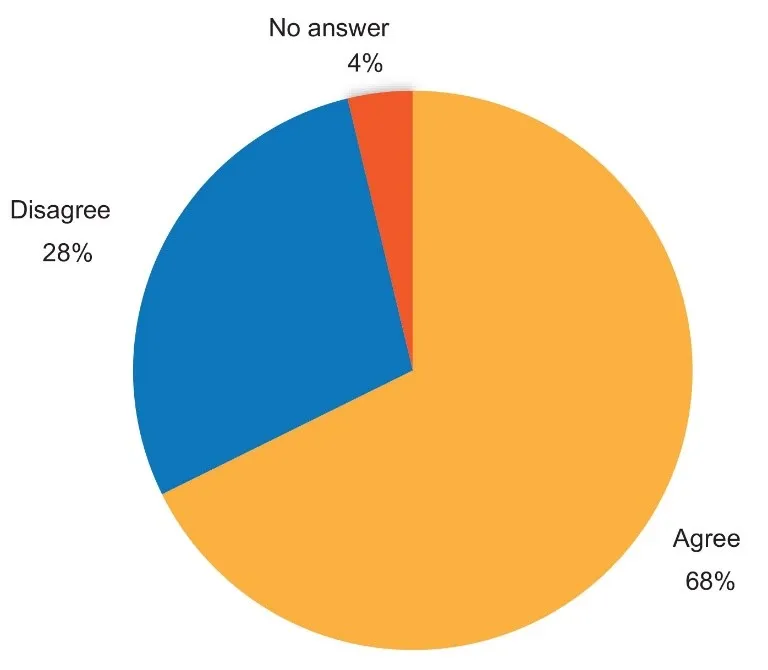
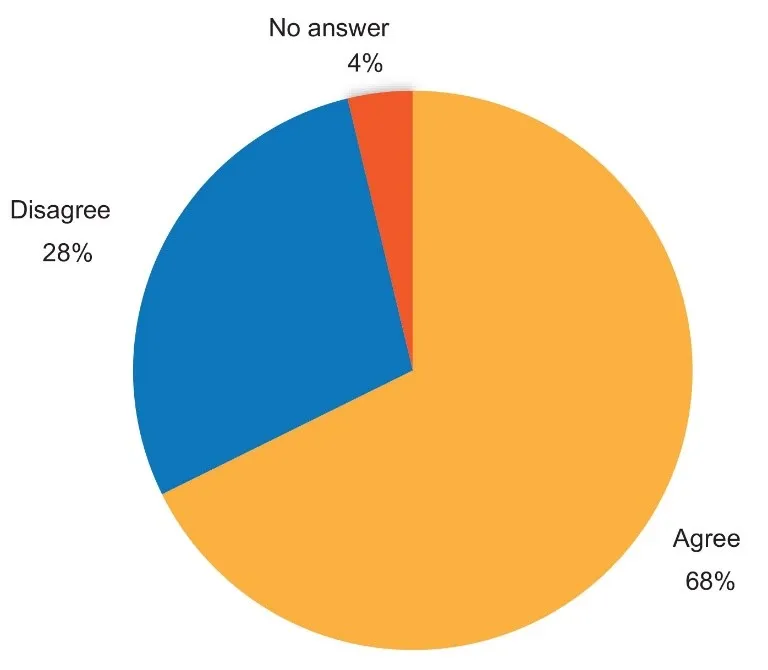
- “Antibiotics can be used to treat viral infections such as common cold, influenza, dengue, etc.”
175/613 disagreed (28 percent) and nearly 4 percent did not answer the question.
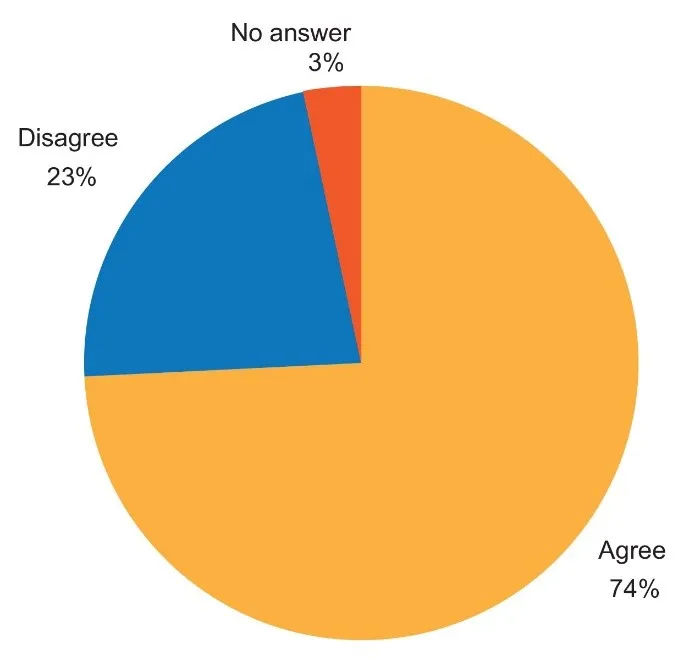
- “Antibiotic resistant bacteria can spread from person to person.”
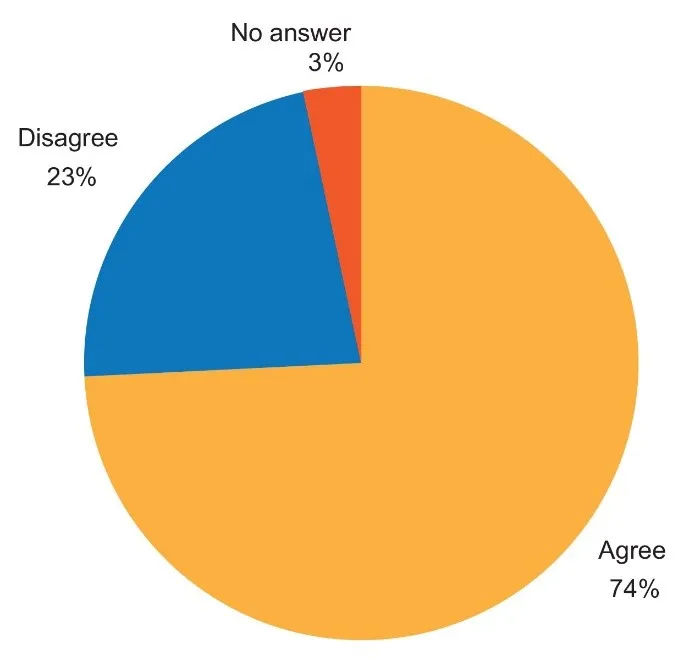
138/613 (23 percent disagreed and a little over 3 percent of the participants did not answer the question.
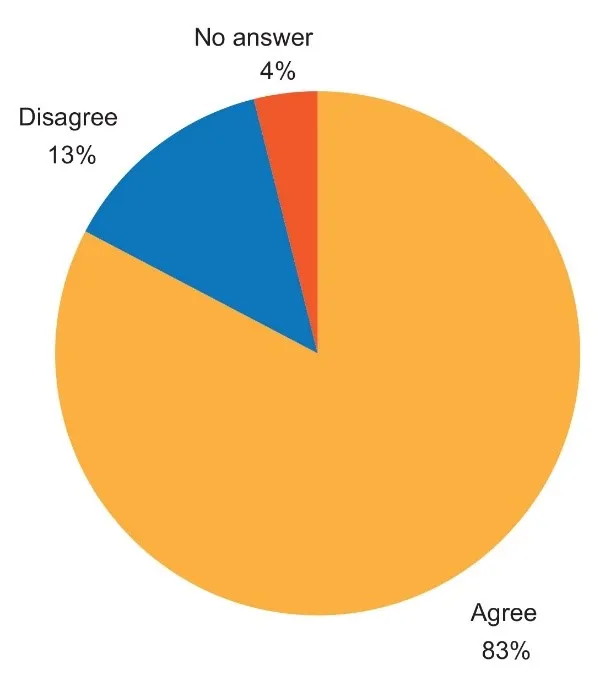
- “Antibiotic resistant bacteria can be transmitted to humans by contaminated water or food.”
82/613 (13 percent) disagreed, and almost 4 percent of the participants did not provide an answer to the question.
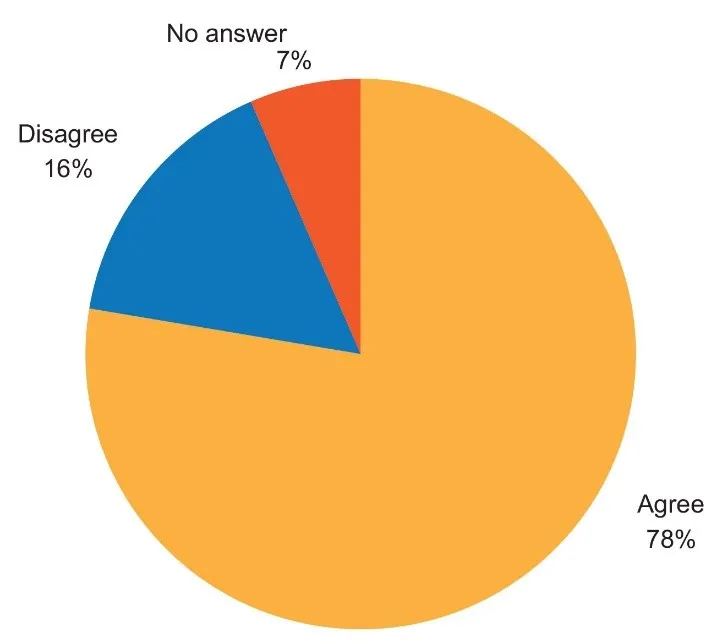
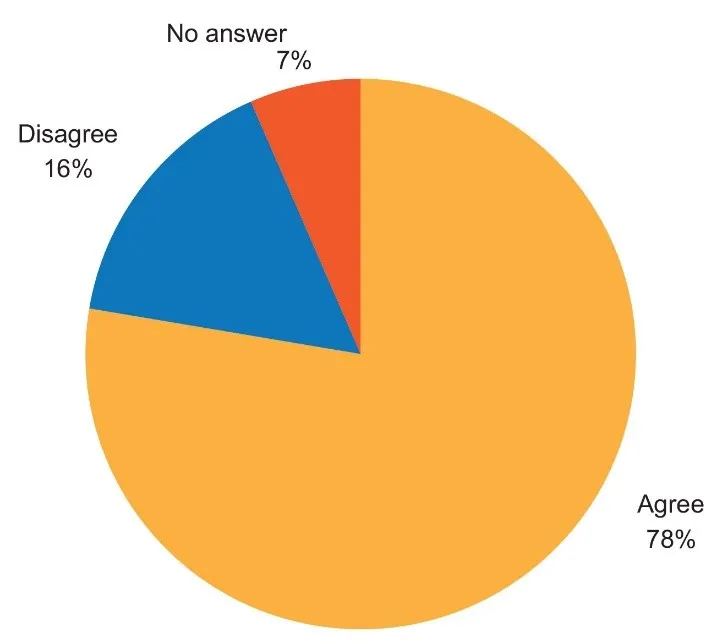
- “Antibiotic resistant bacteria may be found both in the hospital as well as in the community.”
97/613 (nearly 16 percent) disagreed and 6 percent did not answer the question.
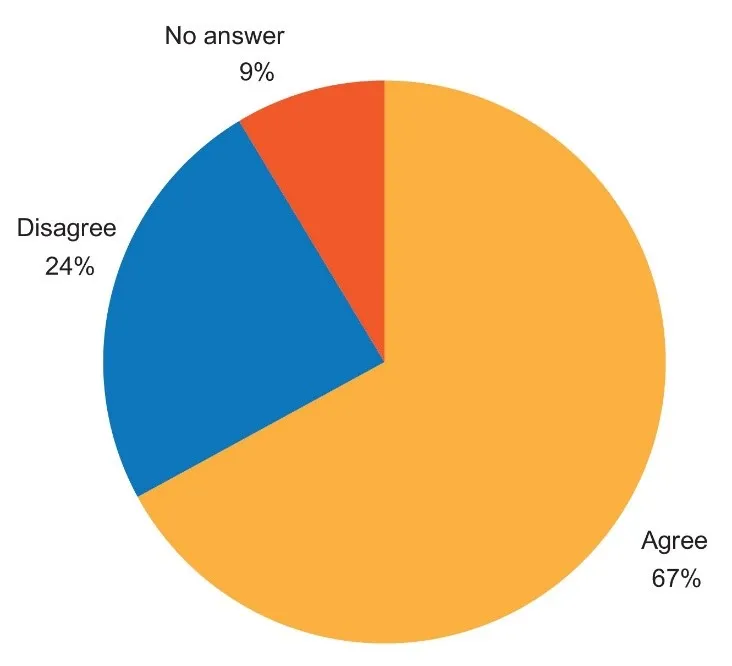
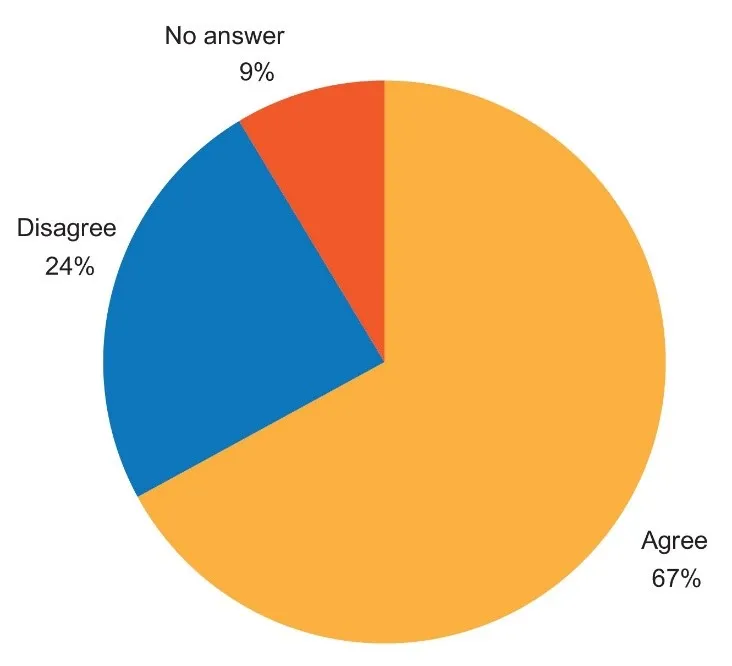
- “Antibiotic resistant infections are more difficult to treat and more expensive to treat than antibiotic sensitive infections.”
149/613 disagreed (24 percent) and nearly 9 percent of the participants did not answer the question.
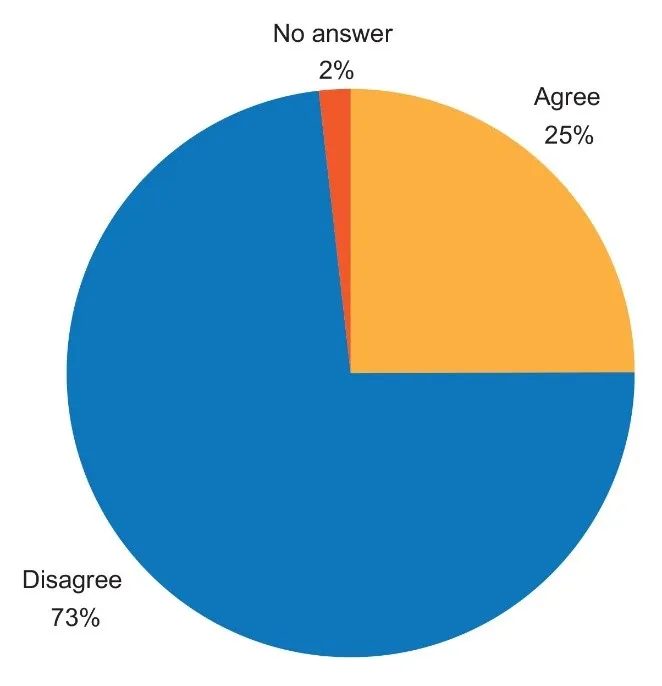
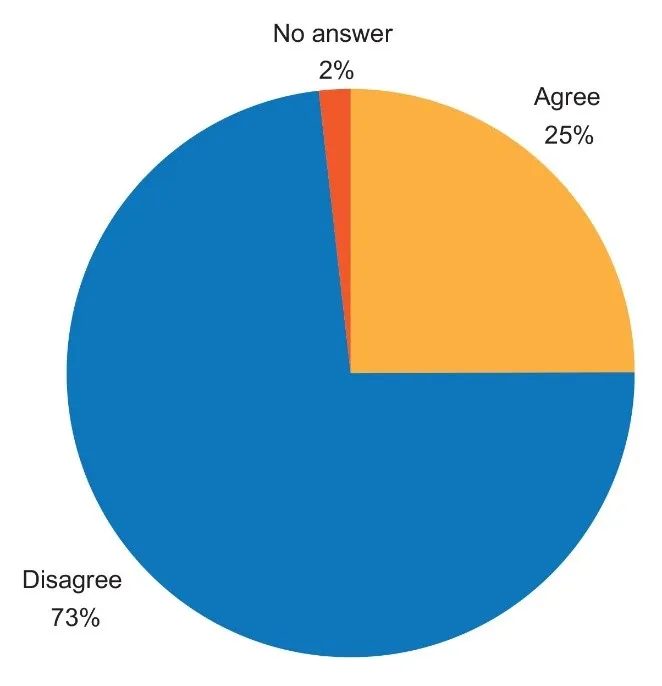
- “Sometimes to save time, you can easily check symptoms on the internet and purchase antibiotics from the pharmacist without asking a doctor.”
449/613 (73 percent) disagreed and almost 2 percent did not answer.
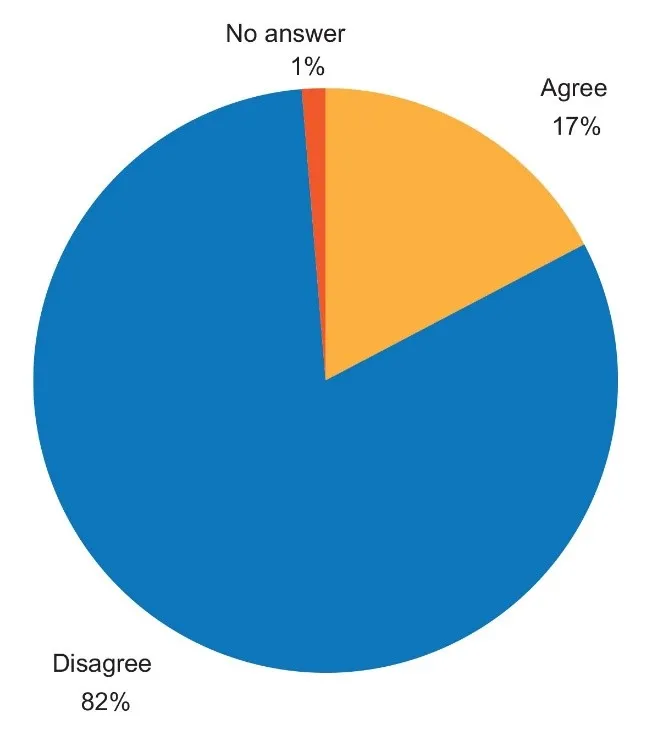
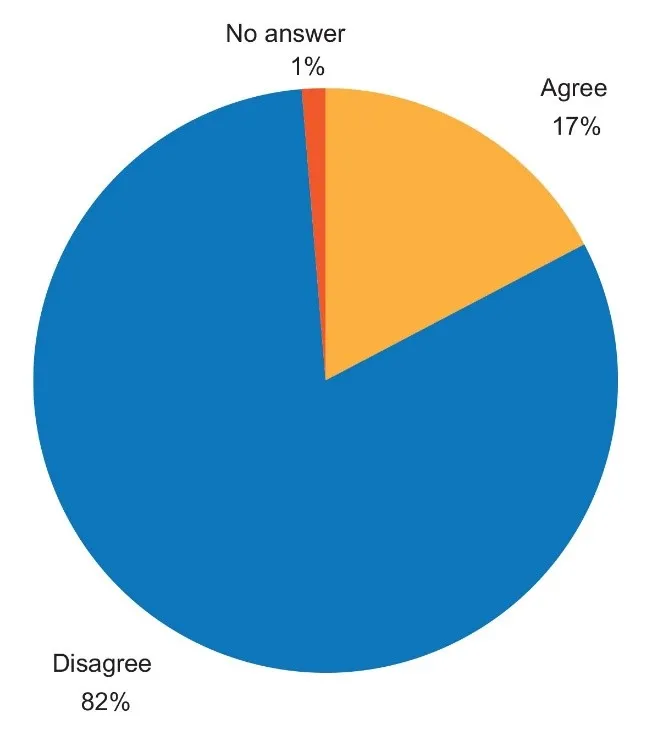
- “Is it okay to share your antibiotics with your needy friend or relative for similar looking symptoms?”
499/613 (82 percent) disagreed, and 1 percent of the respondents did not answer.
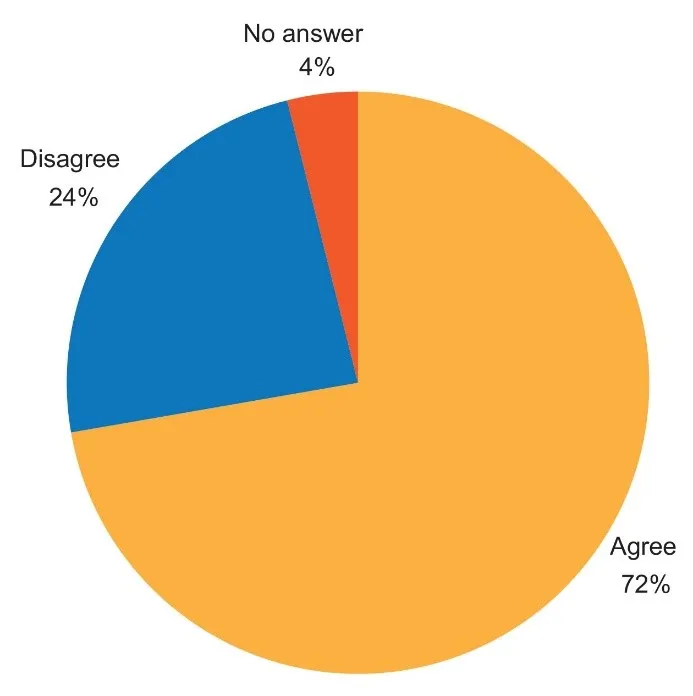
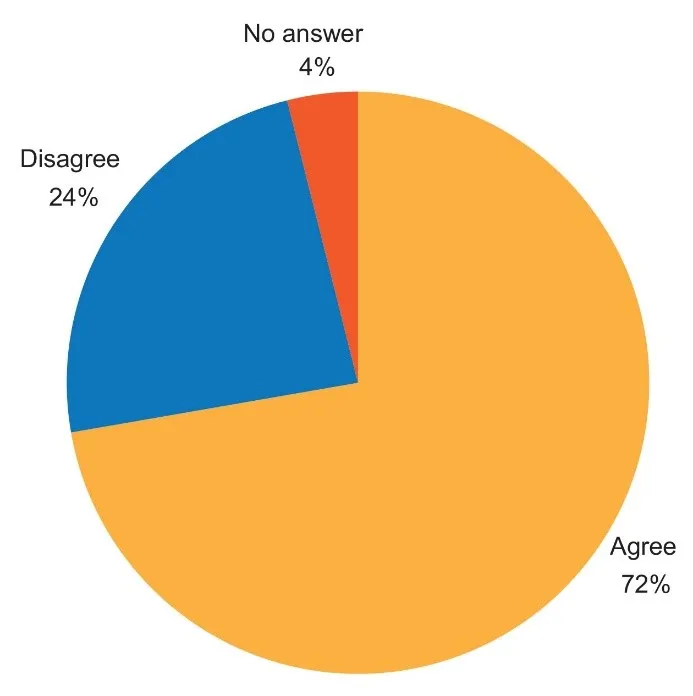
- “It’s our bodies that become resistant to the antibiotic.”
146/613 (24 percent) disagreed, and 4 percent of the participants did not answer the question.
Other findings
- More than seven of every 10 respondents (72 percent, or 443/613) were of the view that it was the human body that became resistant to antibiotics, and not the bacteria. Seventy-four percent of the 443 respondents who thought that it is our body rather than the bacteria that become resistant to antibiotics were adults; 47 percent were graduates or post-graduates; and 29 percent were professionals/teachers/business people.
- Fifty-nine out of 250 responses from 25 teachers and professors (23.6 percent) were wrong. One-third (31.4 percent, or 415/1,320) of the responses from children were wrong. Among the adults, 28.5 percent (1,269/4,790) responses were incorrect.
Discussion and Analysis
Experts estimate that some 10 million people will die every year by 2050 due to antimicrobial resistance or AMR.[3] In 2010, it was reported that India was the world’s largest consumer of antibiotics for human ailments, at 12.9 x 109 units (10.7 units per person). In a study published by Princeton University, it was reported that between the years 2000 and 2010, the consumption of antibiotics increased by 36 percent. The BRICS countries—Brazil, Russia, India, China, and South Africa—accounted for 76 percent of this increase. The per-capita use of carbapenem, for example—which is an antibiotic used to treat serious infections such as sepsis, urinary tract infections, ventilator-associated pneumonia, and post-surgical infections—had risen to over 10 million standard units by 2010.[4] Over-the-counter, non-prescription sales of carbapenems in India are among the highest in the world and contribute to growing carbapenem resistance among Gram-negative bacteria[c] like E. coli, Klebsiella, Pseudomonas aeruginosa and Acinetobacter spp.[5],[6]
Earlier studies have documented that the practice of self-medication is common in India, with patients resorting to such practice to treat ailments such as upper respiratory tract infection or diarrhoea.[7] This present survey found 67 percent of participants believing that antibiotics can be used to treat viral infections such as the common cold, influenza, or dengue. The researchers found poor understanding among the general population of the difference between viral and bacterial diseases, and how they are treated.
One-fourth of the participants in this study said they were comfortable buying antibiotics on their own, based on the symptoms they are showing, if doing so would save them time. This could be a reflection of the lack of access to affordable consultation services with medical doctors. At the same time, however, most of the participants (83 percent) agreed that antibiotics should not be available without prescription. Still, many of them (24 percent) are not aware of the consequences of increasing antimicrobial resistance levels, such as the more expensive treatment required for drug-resistant infections.
Globally, there are ongoing discussions around the concept of ‘One Health’ for antimicrobial containment. ‘One Health’ is a collaborative, multisectoral, and transdisciplinary approach—working at the local, regional, national, and global levels—aimed at achieving optimal health outcomes and recognising the interconnection between people, animals, plants, and their shared environments. Some studies from India have highlighted the presence of antibiotic residues in chicken and honey—while consuming these food products, consumers may be inadvertently getting exposed to antibiotics and facing the possibility of imbibing antibiotic-resistant bacteria.[8],[9] Other studies have found that antibiotics percolate in the food chain. The present survey also wanted to explore the respondents’ understanding of the AMR threat from antibiotic residues in animal products. A number of participants (13 percent) were unaware of this risk.
Indeed, previous studies reported from India have already discovered a lack of knowledge among the general public, as well as even prescribers (i.e., medical doctors), around antimicrobial prescription. A 2019 study from Kerala reported that a little over three percent of respondents (n=755 adults) self-medicated on antibiotic drugs; about 25 percent took self-medication for sore throat; and azithromycin was the most common antibiotic used (reported being used by 39 percent of the respondents). Among the respondents of the same Kerala study, 36 percent used their own doctor’s previous prescription to get antibiotics for another illness. The reason for antibiotic self-medication reported by four of every 10 respondents (41 percent) was convenience.[10]
Another study from West Bengal, conducted in 2019, revealed that although many doctors knew that antibiotics were not indicated for viral infections, over 87 percent of the respondents reported prescribing them in this situation. Moreover, nearly 31 percent of all the doctors who prescribed antibiotics in general relied on sales representatives from pharmaceutical companies as a key source of information on antibiotics.[11]
To be sure, these behaviours are not unique to India. A 2018 study from Japan found that many people obtained antimicrobials from healthcare institutions to treat the common cold; about 12 percent of the participants did not finish the prescribed dosage of their antibiotics; and 24 percent adjusted the doses by themselves without consulting a healthcare professional. The same study found that about 10 percent of the participants had requested antibiotics from their doctors—i.e., although they did not necessarily meet the clinical criteria for antibiotic therapy, they still asked for it. Nearly 30 percent of the respondents preferred to consult with doctors who prescribed antibiotics even for the common cold. The participants in the study said their common sources for information on antibiotics were television news and newspapers.[12]
Knowledge surveys from other developed countries have also revealed noteworthy findings about people’s perspectives on antibiotics. A 2018 study from the United Kingdom (UK) found that respondents residing in more affluent areas of the country possessed better understanding of AMR and the need for more prudent use of antibiotics.[13] The same UK study showed that exposure to an awareness campaign on antibiotics only partially raised their general knowledge on the use of these antimicrobials.[14] Meanwhile, a study from Norway found 57 percent of the 877 participants having high knowledge of antibiotics, in general; 71 percent of them were aware of the dangers of antibiotic resistance.[15] More than nine of every 10 participants in the study were aware that bacteria can become resistant against antibiotics and that unnecessary use of antibiotics can make them less effective.
In contrast, most of the participants in this present study (72 percent) were not aware that bacteria can become resistant against antibiotics because of misuse and abuse. This survey also found a significant number (29 percent) of individuals who had high level of education and were engaged in some professional occupation, having an incorrect perception about antibiotics and AMR—i.e., they believed that it is the human body that could become resistant to antibiotics, and not the bacteria.
Further studies to understand these knowledge gaps are required in India. Indeed, such studies that target a cross-section of the population and aimed at guiding focused and evidence-based awareness campaigns are not common in the country. This present study was undertaken among a specific target group: those with enough interest in science and AMR, that they visited a museum exhibit on the subject matter.
The findings of this study highlight a limited understanding of infectious diseases, the difference between viral and bacterial infections, and the proper use of antimicrobials even among those who have finished higher levels of education. These same people can be potential consumers of significant volumes of antibiotics.
Disseminating information and knowledge about the responsible use of antimicrobials (antibiotics, antiviral, anti-fungal, anti-parasitic agents) is an imperative, given the relatively few antimicrobial classes in the pipeline and increasing levels of resistance reported every year by experts such as those at the Indian Council of Medical Research (ICMR). It is also important to dissect the various social and economic factors that contribute to the overuse of antimicrobials. After all, AMR is not only a medical problem; it has a socio-economic context as well. The solution for containing AMR will therefore come from raising awareness of patients and prescribers about the importance of antimicrobials and how their misuse can cause harm.
There is good evidence that public campaigns promoting responsible antibiotic use may be associated with reductions in overall antibiotic use. The individual impact of various public campaigns in Europe between 1997 and 2007 has been estimated to be equivalent to a 6.5– 28.3-percent drop in the mean level of overall antibiotic use.2 Literature on the topic of antibiotic awareness campaigns done within India and globally support a multi-modal and coordinated strategy. For example, a nationwide voluntary antibiotic resistance awareness campaign in India in 2019 used multiple pedagogical and participatory techniques such as physical events, lectures, posters, booklet/pamphlet distribution, audio and video messages, competitions, mass rallies, and broadcast of messages in local languages using community radio stations across the country.[16]
Another study by Mathew et al. from India explored the appropriate communication strategies for improving public awareness on responsible antibiotic use.[17] Key strategies included emphasising the following: a) that antibiotic resistance is a global health issue; b) the misuse of antibiotics is the primary driver of AMR; c) the imperative of designing communication strategies for AMR; d) making the proper decisions about the target groups for messaging campaigns; e) nurturing leadership in communication and raising awareness; f) designing the messaging approach; g) engaging professional and industry groups; h) identifying stakeholders of the messaging strategy; i) promoting behaviour change; j) reinforcing or building a sound regulatory environment; k) creating material and emotional incentives; and l) building an enabling social structure for behaviour change.[18]
In 2019, WHO conducted a global survey of stakeholders in 55 countries on improving antibiotic awareness campaigns. It found 45 campaigns (75 percent) were conducted on a national level and most of them (47/60 or 78 percent) were organised by public health authorities and were publicly funded. There were no substantial differences between low- and middle-income countries, on one hand, and on the other, high-income countries, in the types of key messages that proved effective in raising AMR awareness. A ‘One Health’ approach was mentioned in 13/60 antibiotic awareness campaigns (22 percent). Most messages were universally applicable; however, there was no systematic effort to adapt these campaigns according to locally prevalent public misconceptions.[19]
It is to be noted that large amounts of antimicrobials are also used in animals which can have important consequences on AMR in humans. It has been reported that in animals whose meat is consumed as food, the total global utilisation of antimicrobials was about 131,000 tonnes in 2013; the volume is expected to reach about 200,000 tonnes by 2030.[20] Antibiotic use in food animals is not only for treatment and prevention of infections, but also for growth promotion (i.e., the administration of antimicrobials to animals to boost weight gain.)[21] The problem of AMR cannot be adequately addressed without focusing on a ‘One Health’ approach where human health and animal health issues are recognised as being closely linked, and thereby addressed using an integrated approach.
Conclusion
There is enough evidence of increasing levels of antimicrobial resistance in India. The usefulness of antibiotic awareness campaigns in reducing antimicrobial use is also well-documented. The immediate imperative is for the government to address the problem on war-footing and initiate country-wide campaigns for raising awareness and changing behaviours around antibiotics use. In India, antibiotic-resistant infections—despite their high morbidity, mortality, and healthcare costs—are still not notifiable to the public health authorities under any law.
Any effort to disseminate proper and adequate information on AMR will benefit from the widespread availability and use of social media. The primary challenge will be in creating the most effective messages that are suited to Indian settings, where there is considerable diversity in how healthcare is delivered. This is a crucial consideration, as some countries have reported—as discussed briefly earlier in this report—that exposure to an antibiotics campaign did not raise public respondents’ knowledge on AMR and only partially raised their general knowledge on antibiotics use.[22] Such studies imply the need for optimisation of public awareness campaigns in terms of form and content. They also underline the need to have targeted strategies, tailored to ground realities and local environments, tied together by a multi-sectorial approach.
The problem of AMR is multi-faceted. Public opinion and understanding is one of the many facets but a critical one as far as end-user knowledge and awareness is concerned.9 This report has attempted to shine the light on that aspect of the AMR solution that has largely remained unaddressed within the Indian context. The aim of the authors is to offer a pathway to a deeper understanding of public perception about antibiotics and AMR—all on a more comprehensive national scale.
At the same time, the community must be regarded as a critical pillar of any awareness strategy on combating AMR.[23] This survey assesses awareness levels about antibiotics use and antimicrobial resistance among urban, educated communities in a metropolitan city in India. The poor understanding and knowledge of the general population in AMR highlights the need to undertake integrated awareness campaigns based on evidence to ensure desirable results in terms of behaviour change amongst targeted population groups.
Annex
Invitation to the survey and questions:
ANTIBIOTIC AWARENESS SURVEY AMONG VISITORS OF THE SUPERBUGS EXHIBITION AT SCIENCE CITY MUSEUM IN KOLKATA, INDIA, JAN- FEB 2021
Dear Guest,
Welcome to the Superbugs Exhibition!
Your participation in this short survey will help us in understanding public awareness and develop policies to combat the problem of Antibiotic Resistant Bacterial Infections in India.
Thank you for your support.
ICMR and National Council of Science Museum, India
|
Your Age: A. 60 years
Education: A. Post graduate; D. Graduate; C. up to Class 12; D. up to Class 10 or less
Profession: A. Housework; B. Business; C. Student; D. Professional (doctor/ engineer/ lawyer, etc.);
E. Teacher/ Professor; F. Others
|
|
Q 1: Antibiotics should not be purchased or used without the prescription of a registered medical doctor.
Answer: A. Agree; B. Disagree
Q2: Antibiotics are used in animals as well as humans.
Answer: A. Agree; B. Disagree
Q3: Antibiotics can be used to treat viral infections such as common cold, influenza, dengue, etc.
Answer: A. Agree; B. Disagree
Q4: Antibiotic resistant bacteria can spread from person-to-person.
Answer: A. Agree; B. Disagree
Q5: Antibiotic resistant bacteria can be transmitted to humans by contaminated water or contaminated food.
Answer: A. Agree; B. Disagree
Q6: Antibiotic resistant bacteria may be found both in the hospital as well as in the community.
Answer: A. Agree; B. Disagree
Q7: Antibiotic resistant infections are more difficult to treat and more expensive to treat than antibiotic sensitive infections.
Answer: A. Agree; B. Disagree
Q8: Sometimes to save time, you can easily check symptoms on the Internet and purchase antibiotics medicines from the pharmacist without asking a doctor?
Answer: A. Agree; B. Disagree
Q9: It is okay to share your antibiotic medicines with a needy friend or relative for similar looking symptoms?
Answer: A. Agree; B. Disagree
Q10: It’s our bodies that become resistant to the antibiotic.
Answer: A. Agree; B. Disagree
|
Kamini Walia is Program officer AMR, Division of Epidemiology and Communicable Diseases, Indian Council of Medical Research.
Subhabrata Chaudhuri is former Director, Science City, Kolkata; Director, Nehru Science Centre, Mumbai.
Rina Sinha is National Professional Officer, Public Information and Advocacy, WHO Country Office for India.
Subhasankar Ghosh is Curator at Science City, Kolkata.
Abhirup Chowdhury and Souvik Manna are students of Molecular Medical Microbiology at the Department of Microbiology, Tata Medical Center, Kolkata.
Dr Sanjay Bhattacharya is Consultant in Microbiology at Tata Medical Center, Kolkata.
Endnotes
[a] Antimicrobial resistance (AMR) occurs when micro-organisms such as bacteria do not respond to antibiotic therapy because of certain structural, functional, genetic changes in the bacteria.
[b] The exhibition was supported by the Indian Council of Medical Research (ICMR), the Science Museum Group of the UK, and Welcome Trust, and organised by the National Council of Science Museums, Ministry of Culture, Government of India.
[c] Gram-negative bacteria include micro-organisms such as E. coli, Salmonella, Klebsiella, Pseudomonas, and Acinetobacter which cause infections in community as well in healthcare facilities.
[1] World Health Organization, “Antimicrobial resistance,” Fact Sheets, November 17, 2021.
[2] Welcome Trust, HM Government, “Review on Antimicrobial Resistance: Tacking Drug Resistance Infection globally”.
[3] World Health Organization, “Antimicrobial resistance.”
[4] T.P. Van Boeckel, S. Gandra, A. Ashok, Q. Caudron, B.T. Grenfell, S.A. Levin, et al. “Global antibiotic consumption 2000 to 2010: An analysis of national pharmaceutical sales data,” Lancet Infect Dis 14 (2014): 742–50.
[5] R. Laxminarayan and R.R. Chaudhury, “Antibiotic Resistance in India: Drivers and Opportunities for Action,” PLoS Med 13 (2016): e1001974.
[6] T.P. Van Boeckel, et al., “Global antibiotic consumption 2000 to 2010: An analysis of national pharmaceutical sales data.”
[7] A. Rajendran, K.G. Kulirankal, P.S. Rakesh, S. George, “Prevalence and Pattern of Antibiotic Self-Medication Practice in an Urban Population of Kerala, India: A Cross-sectional Study,” Indian J Community Med 44 (2019): S42-S45.
[8] R. Sahu and P. Saxena P, “Antibiotics in Chicken Meat,” Report No.: Contract No.: PML/PR-48/2014 (New Delhi, India: Centre for Science and Environment, 2014).
[9] B. Er Demirhan and B. Demirhan, “Detection of Antibiotic Residues in Blossom Honeys from Different Regions in Turkey by LC-MS/MS Method,” Antibiotics (Basel, Switzerland) 11 (2022): 357.
[10] A. Rajendran, et al., “Prevalence and Pattern of Antibiotic Self-Medication Practice in an Urban Population of Kerala, India: A Cross-sectional Study,” Indian J Community Med 44 (2019): S42-S45
[11] M. Nair, S. Tripathi, S. Mazumdar, et al., “Knowledge, attitudes, and practices related to antibiotic use in Paschim Bardhaman District: A survey of healthcare providers in West Bengal, India,” PLoS One 14 (2019): e0217818.
[12] K. Kamata, Gu. Y. Tokuda, N. Ohmagari, and K. Yanagihara, “Public knowledge and perception about antimicrobials and antimicrobial resistance in Japan: A national questionnaire survey in 2017,” PLoS One 13 (2018): e0207017.7.
[13] T. Mason, C. Trochez, R. Thomas, M. Babar, I. Hesso, and R. Kayyali, “Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance,” BMC Public Health 18 (2018): 711.
[14] T. Mason, et al., “Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance.”
[15] M. Waaseth, A. Adan, I.L. Røen, et al., “Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers – A cross-sectional study,” BMC Public Health 19 (2019): 66.
[16] Ashok J. Tamhankar, R. Singh, et al., “Characteristics of a Nationwide Voluntary Antibiotic Resistance Awareness Campaign in India; Future Paths and Pointers for Resource Limited Settings/Low and Middle Income Countries,” Int Environ Res Public Health 16 (2019): 5141.
[17] P. Mathew, S. Sivaraman, S. Chandy, “Communication strategies for improving public awareness on appropriate antibiotic use: Bridging a vital gap for action on antibiotic resistance,” J Family Med Prim Care 8 (2019): 1867-71.
[18] P. Mathew, et al., “Communication strategies for improving public awareness on appropriate antibiotic use: Bridging a vital gap for action on antibiotic resistance.”
[19] B. Huttner, M. Saam, L. Moja, et al., “How to improve antibiotic awareness campaigns: findings of a WHO global survey,” BMJ Glob Health 4 (2019): e001239.
[20] K. Walia, M. Sharma, S. Vijay, B.R. Shome, “Understanding policy dilemmas around antibiotic use in food animals & offering potential solutions,” Indian J Med Res 149 (2019): 107-118.
[21] P. Mathew, S. Sivaraman, S. Chandy, “Communication strategies for improving public awareness on appropriate antibiotic use: Bridging a vital gap for action on antibiotic resistance.”
[22] A. Rajendran, et al., “Prevalence and Pattern of Antibiotic Self-Medication Practice in an Urban Population of Kerala, India: A Cross-sectional Study,” Indian J Community Med 44 (2019): S42-S45
[23] World Health Organization, “Antimicrobial resistance.” See also, Welcome Trust, HM Government, “Review on Antimicrobial Resistance: Tacking Drug Resistance Infection globally.”
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

 PDF Download
PDF Download


 PREV
PREV








