Introduction
The World Health Organization (WHO) defines non-communicable diseases (NCDs), or chronic diseases, as illnesses of long duration and the product of a combination of genetic, physiological, environmental, and behavioural factors.[1] The major types of NCDs are cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes. This paper focuses on the NCDs burden of India’s older adult women, which is a result of multiple factors, including what experts refer to as “social determinants of health”. These are “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”[2] They can include income and social protection, education, unemployment and job insecurity, housing, basic amenities, and the environment.
Women’s health has been historically under-prioritised and under-funded, especially beyond reproductive and maternal health. Later in their life, women bear an uneven and disproportionate share of the elderly illiterate, financially uninsured, and progressively diseased population. This phenomenon can be partly explained by the impact of social biases and gendered roles. For example, older adult women bear a disproportionate amount of unpaid care work (245 minutes a day for elderly women; 112 minutes for elderly men); they are often segregated in poorly paid labour-intensive work; and they have poor access to digital tools and technology. They also face the risk of gender-based violence. Nutritional deficiencies and morbidities like anaemia (5.9 percent women compared to 3.1 percent men) and obesity (10.2 percent of women compared to 3.4 percent of men) further exacerbate with age.
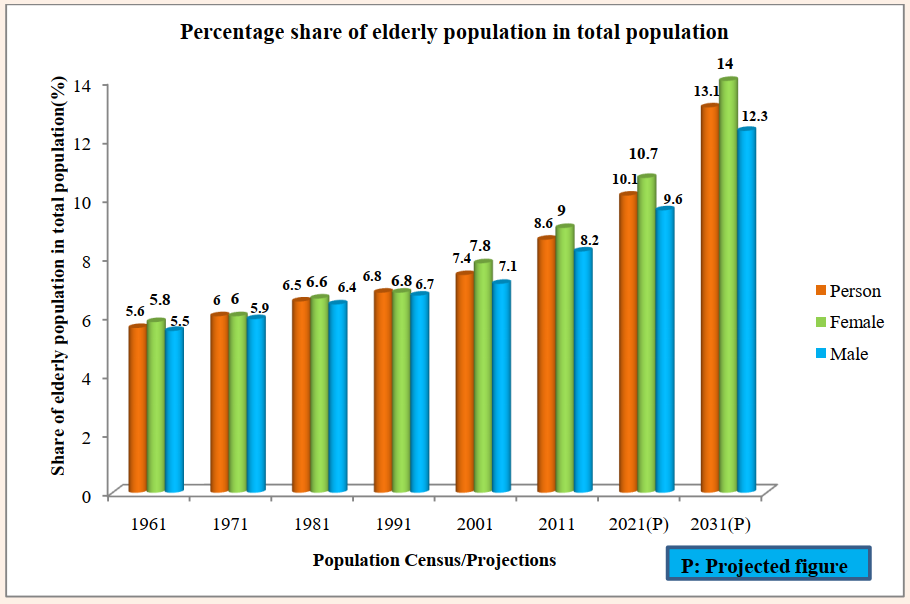
The population of India’s elderly[a] was at 138 million in 2021, of which 71 million were females.[3] Further, the share of the country’s overall population comprising the elderly has been steadily rising since 1961: the elderly males, from 5.5 percent (1961) to 9.6 percent (2021); and elderly females, from 5.8 percent (1961) to 10.7 percent (2021) (see Figure 1).
Figure 1: India’s Elderly Population as % of Total
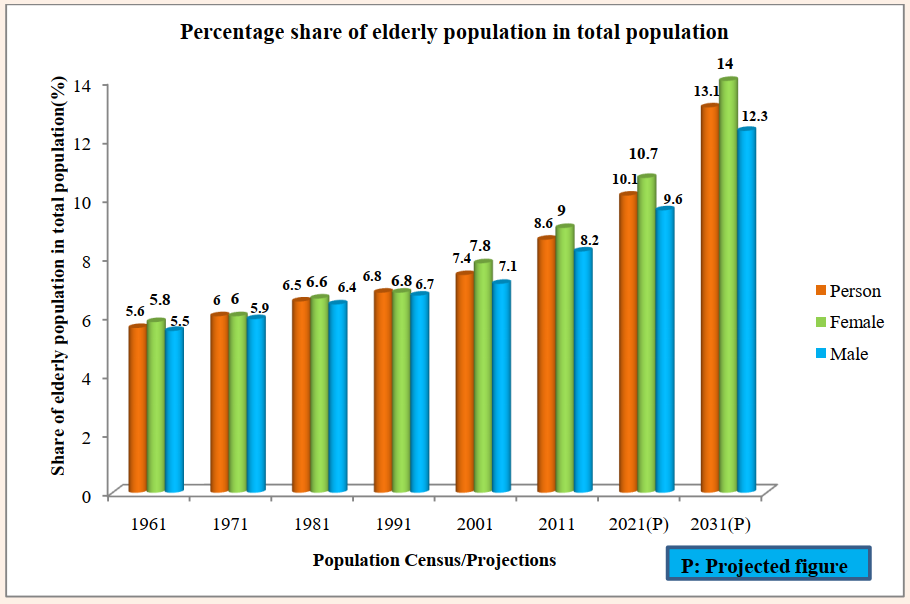
Source: Elderly in India 2021, Ministry of Statistics & Programme Implementation[4]
As the proportion of the elderly has been increasing in recent years, little attention is being paid to their specific health challenges. While the National Sample Surveys (NSS) and Census regularly take stock of their numbers, there is a lack of understanding of the unique challenges that they face, because of their age, with regard to the prevalence of NCDs. Filling this gap in the literature should help India make appropriate elderly-related policies towards the fulfilment of targets encoded in SDGs 3 and 5. In particular, addressing the challenges facing older adults are related to the following goals:
- 4 (To reduce by one-third pre-mature mortality from NCDs through prevention and treatment and promote mental health and well-being);
- 8 (To achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all); and
- 4 (To recognise and value unpaid care and domestic work through the provision of public services, infrastructure, and social protection policies, and the promotion of shared responsibility within the household and the family as nationally appropriate by 2030).
Furthermore, in line with the United Nations Decade of Healthy Ageing (2021–2030), this paper recommends the implementation of person-centred integrated care and long-term health services that will be more responsive to older people.
Review of Literature
Global Literature
Research from both developed and developing countries have captured the gender gap in self-rated health among the elderly. For instance, Le, Quashie and Prachuabmoh (2018) found, in their study of older adults in Vietnam, that the proportion of elderly women rating their health poorly was higher than that of elderly men.[5] A similar study of older adults in Singapore showed the gender differences in self-reported health and prevalence of chronic diseases and functional disability, which had reduced significantly when demographic, socio-economic, health risk behaviours, and social support factors were controlled for.[6] Meanwhile, a cross-city analysis in Latin America and the Caribbean suggests that women displayed worse health outcomes, of which self-rated health was a part, than men in all seven cities covered by the study.[7] In Taiwan, the gender gap in self-perceived health is considerable despite controlling for various health factors.[8] Evidence from Mexico also suggests that older women rate their health poorer than their male counterparts.[9]
The prevalence of multi-morbidity is higher among women compared to men, not only for chronic ailments but also for other diseases. The reasons are many, and they encompass biological, sociocultural, and economic causes. Existing studies also focus on the prevalence of NCDs, in particular, among women across different age groups.
In Nepal, females were found to be more often affected by cancer than males.[10] While breast cancer is more prevalent among younger women, cervical cancer is more common in middle-aged women, and lung cancer among the elderly women.[11] The prevalence of diabetes and impaired fasting glucose in the country was observed to increase with age for both men and women.[12],[13] Meanwhile, a study based on the elderly in Uganda observed that the reporting behaviour of NCDs was generally higher in the 60-69 years and 70-79 years age groups, and within these age groups, the likelihood was higher among older women.[14] In China, diabetes, hypertension, and dyslipidaemia were more prevalent among men, and osteoporosis was more common among women.[15] While the prevalence of diabetes, osteoporosis, and hypertension increased with age among both men and women, this was the case with obesity and dyslipidaemia only among women.
A study of employees in a large company in Iran suggests that the prevalence of diabetes, cardiovascular diseases, osteoporosis, and cancer increased with age among both men and women.[16] Similar results were found in a study in Qatar, where prevalence increased with age, and this rise was highest in the 30 to 49 age group.[17] Another study, this time of Canadian adults, found that women’s poorer health (measured in part by the presence of chronic illnesses like arthritis and high blood pressure) is partially attributable to their reduced access to social and material conditions that enable good health, and to the everyday stressors associated with women’s social roles.[18]
Women are more likely to have lower incomes, be single parents, carry a “double day” (working full- or part-time and carrying out household duties for their family), and work in lower-status occupations. A cross-country analysis of the elderly in the United States , the United Kingdom, Italy, Germany, and Spain, found that time allocated to paid work, household work, and active leisure activities was associated with favourable health among both women and men; the gender gap, however, was higher in Germany, Italy, and Spain.[19]
The link between NCDs and health risk behaviours, and the gendered prevalence of the latter, is well-documented. A study conducted among the poor elderly in rural Brazil found that among both men and women, consumption of alcohol with smoking, and physical inactivity with smoking, were the most prevalent cluster of risk factors.[20] They also concluded that men were more physically inactive than women. Another study of the elderly in Brazil revealed that the most frequent health risk cluster among women and men was physical inactivity and excess weight.[21] A community-based study in Ethiopia noted that the co-occurrence of multiple behavioural risk factors like harmful drinking, physical inactivity, and poor fruit and vegetable intake was more prevalent among women than men.[22]
It is observed that while pension coverage for those aged over 50 years was 51 percent, it was 79 percent among those aged above 65 in South Africa.[23] Research further notes that pension status was associated with a higher frequency of outpatient visits and treatment of hypertensive status; however, it was not associated with self-reported health. A study of Vietnamese households suggests that individuals who had reported NCDs as well as health insurance were twice as likely to utilise outpatient care compared to their counterparts without insurance. However, no significant association was found between having health insurance and the status of household members with reported NCDs.[24]
The Indian Context
Similar trends are occurring in India. The prevalence of NCDs among women is 62 per 1,000, as compared to 36 per 1,000 men.[25] Hypertension, depression, gastrointestinal illness, and diabetes are the most common NCD morbidities in the country. A 2012 study examining the health status of elderly women in rural India showed that hypertension is the most common NCD (78 percent of respondents were reported to have the disease), followed by osteoarthritis (73 percent), diabetes (66 percent), and bronchial asthma (77 percent).[26]
Data from the first Longitudinal Ageing Study in India (LASI), released in 2017, reveal sex differences in the prevalence, and socio-demographic and risk factors for NCDs among older adults in India.[27] Studies have established the gender gap in self-rated health outcomes among the elderly.[28],[29],[30],[31] The same LASI report shows that poor self-rated health is twice as common among adults aged 60 years and above as compared to those between 45 and 59.[32] Elderly women are also more likely to report poor self-rated health.
A study of elderly Indian women categorised into three age groups—60-69, 70-79, and above 80—found that the prevalence of diabetes and cancer increases with age.[33] In a study of the health of women in eastern Indian states, mild anaemia was found to be most prevalent among the adolescents ever-married and least among the younger never-married; moderate anaemia was highest among the younger never-married and adolescent ever-married; severe anaemia was most prevalent among the older never-married; and least so among younger ever-married women.[34]
Overweight/obesity is another health concern and is associated with a number of NCDs,[35] as it increases the risk of morbidity, disability, and death. Although measures such as waist circumference and waist-to-hip ratio are significantly associated with a higher prevalence of multi-morbidities among both the elderly men and women, a higher proportion of older women were found to be at high-risk waist-hip ratio (78.5 percent of women vs 75.4 percent of men) and waist circumference (37.1 percent of women vs 8.9 percent of men).[36] Increased cardiovascular occurrences, such as coronary heart disease, hypertension, stroke, type 2 diabetes, and several cancers, including breast cancer in postmenopausal women, endometrial cancer, and colon and kidney cancer, are major risk factors for mortality.[37] Women had, on average, more NCD risk factors than males did, due to risk factors like obesity and inactivity, which have been shown to be more common in women than in men.[38],[39]
The LASI data reveals a higher prevalence of tobacco use among the northeastern and eastern regions. The prevalence of obesity was found to be higher among urban men and women of all age groups as compared to their rural counterparts; the prevalence of both obesity and behavioural risk factors was found to increase with age in both areas.[40] A study by the World Health Organization (WHO) found that the percentage of adult women with inadequate physical activity is higher than in adult men; this is reversed in the case of smoking and alcohol consumption, in which the gender gap is also far more significant.[41] People in the highest wealth group, those aged above 70 years, women, and tobacco users had a higher likelihood of reporting NCD multimorbidity.[42]
Kundu et al. (2022) also found that, regardless of region, the spending incurred by the elderly on private health facilities was nearly five times the expenditure incurred on public ones.[43] Analyses of the LASI numbers reveal that the elderly with health insurance were more likely to have a higher uptake of public healthcare services and increased with age for outpatient consultations. For inpatient consultations, the preference for public health facilities declined with age, for both men and women. However, females use less inpatient and more outpatient services compared to men; this is because women are observed to report fewer health concerns compared to men.[44]
Furthermore, NSSO data from 1995-96 and 2014 suggests that first, while the proportion of men engaged in paid work and unpaid work/not working is equal, among older women, 90 percent of them fell into the latter category and second, poor self-rated health was associated with involvement in unpaid work, and not working.[45] The study notes that perceived bad health and immobility among the elderly increased from paid workers to unpaid workers and the non-working population.[46] The prevalence of household work and lesser paid or unpaid work among women thus exacerbates the burden of NCDs in their old age.
An equally vital role is played by the presence, or absence, of social protection measures. Across countries in the Global South, there is insufficient access to pension and insurance among the older populations.[47],[48],[49] Even as women, in particular, live longer than men, the former is less likely to have access to retirement, pension, or salaried employment.[50]
The above review of literature underlined the different social factors that affect the prevalence of NCDs among elderly women in India: income, social protection, and behavioural patterns. However, much of existing literature focus on self-rated health among the older adults, rather than the incidence and burden of specific NCDs, as found in official government statistics.
Evidence from Emerging Data
Gender becomes a key social determinant in an individual’s health quality of life in old age. Research shows that despite women having higher life expectancy, they are also more prone to experiencing poor health in their older age and are living more years with morbidities, compared to men.[51] Cancers, diabetes, cardiovascular diseases, chronic respiratory illnesses, and other non-communicable diseases are on the rise in low-income countries because of the increased prevalence of key modifiable behavioural risks, such as unhealthy diets and tobacco use, and reductions in infectious diseases.[52] At the same time, population ageing and growth are amplifying the speed of the shift from communicable, maternal, neonatal, and nutritional diseases to non-communicable diseases. More than three-quarters of all NCD fatalities worldwide (31.4 million) occur in low- and middle-income countries, where they affect people disproportionately.[53]
1. Cardiovascular Diseases
The age-associated increase in the prevalence of chronic diseases is very evident for cardiovascular and lung diseases. The LASI report (Wave I) notes increasing prevalence of cardiovascular diseases (CVDs) along the age groups: 22 percent in 45 to 59 years; 34.6 percent in the 60-74 group; and 37 percent among those above 75. [54] Diagnosed prevalence of cardiovascular diseases is also higher among the elderly women and men in urban regions, and among elderly women, overall. Of the elderly women, according to a 2014 United Nations Population Fund report, the prevalence of NCDs was considerably lower in the 60-69 cohort (60.7 percent) than the older group of 70 and above (74.1 percent).[55]
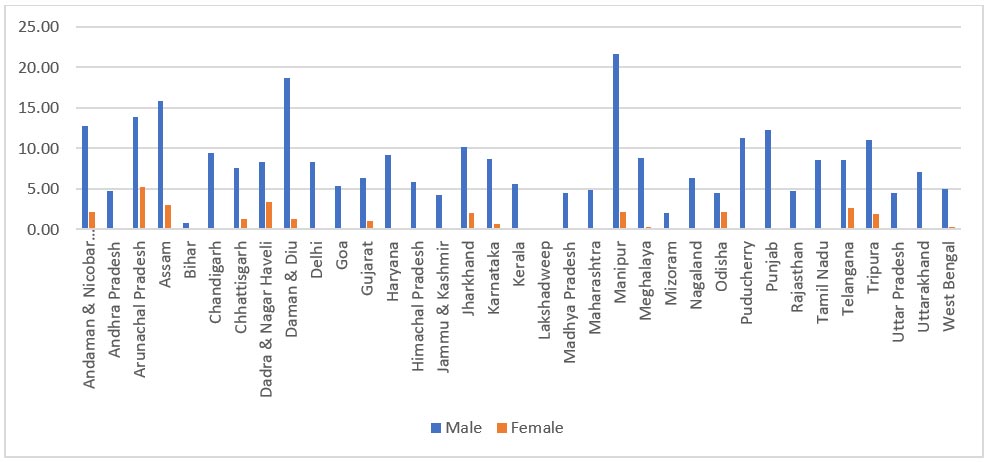
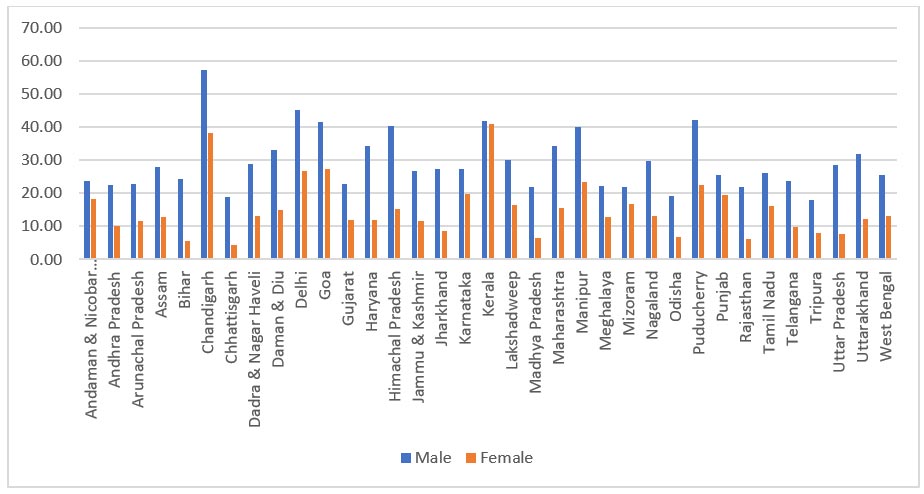
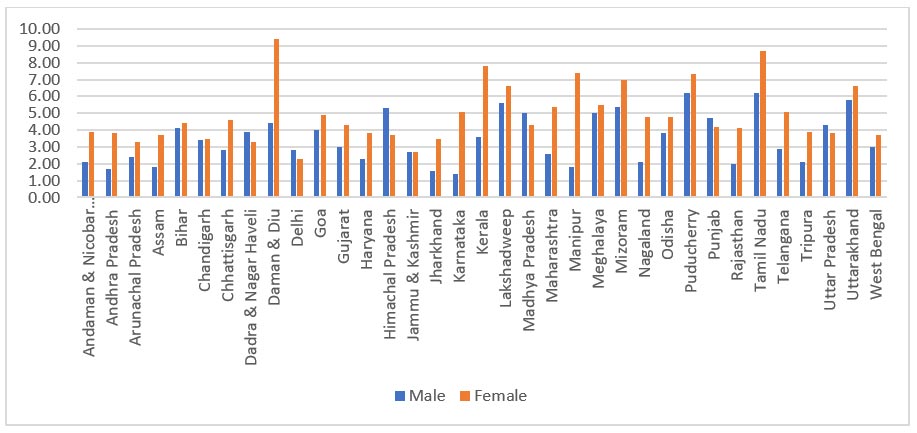
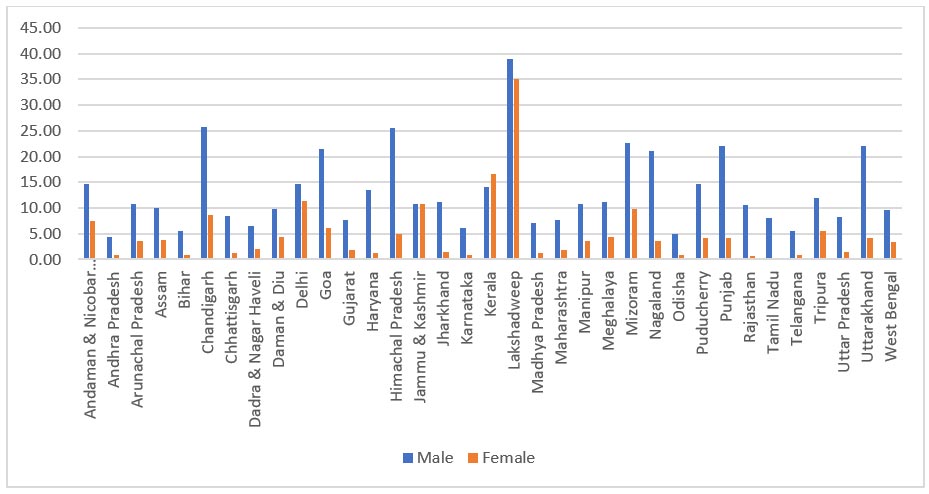
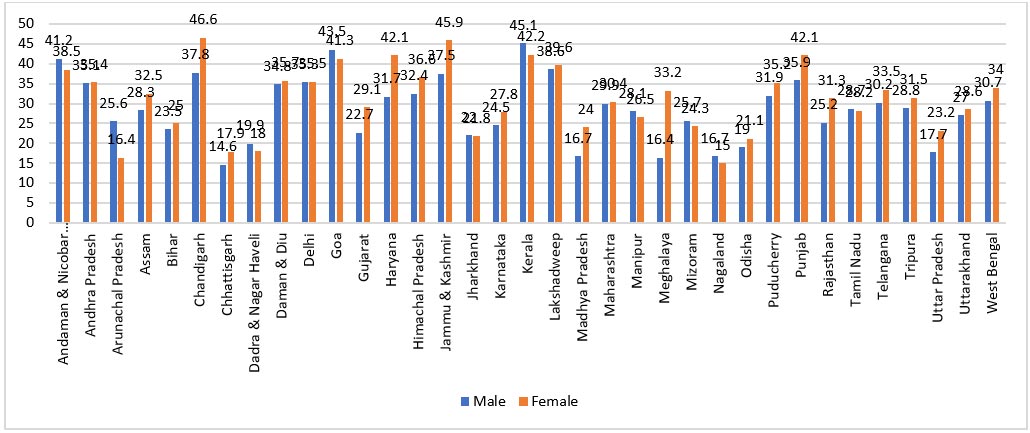
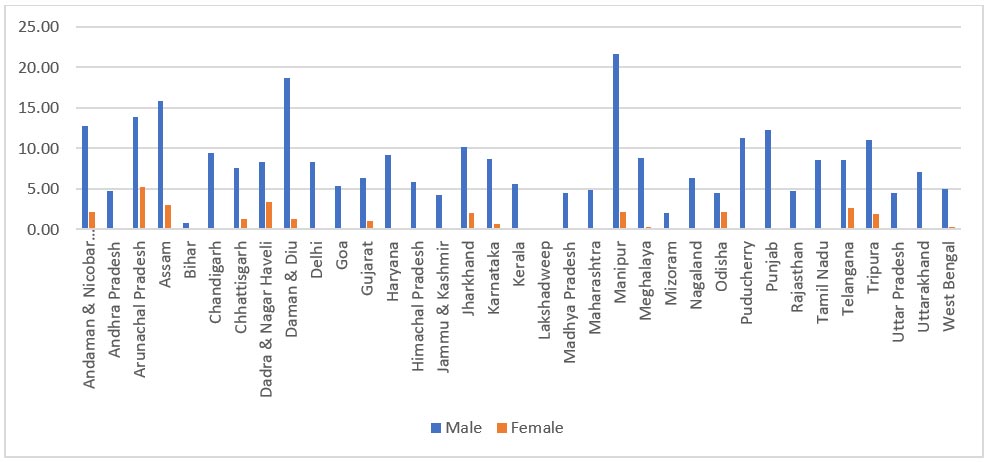
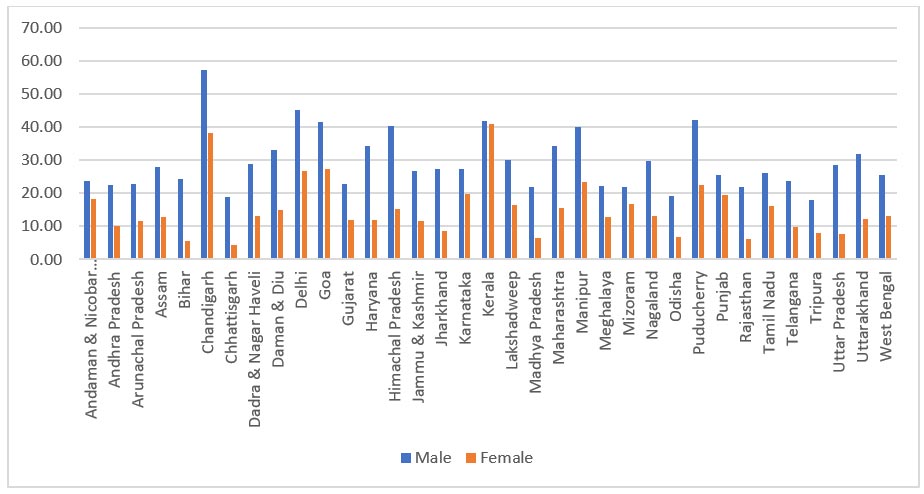
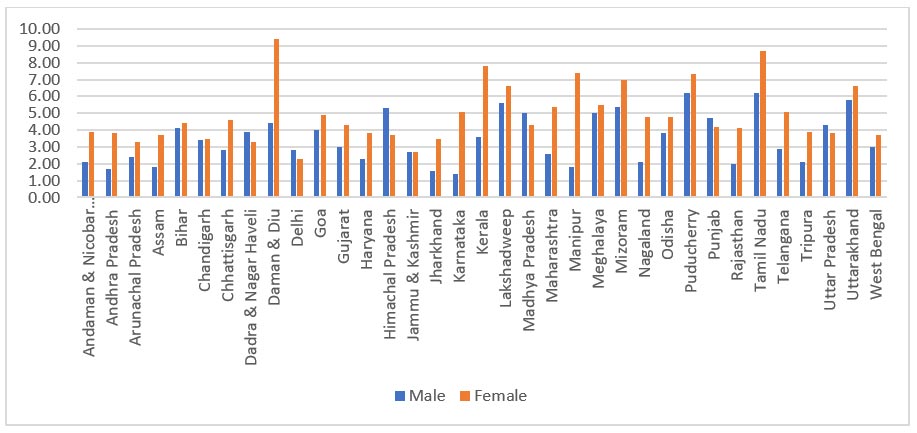
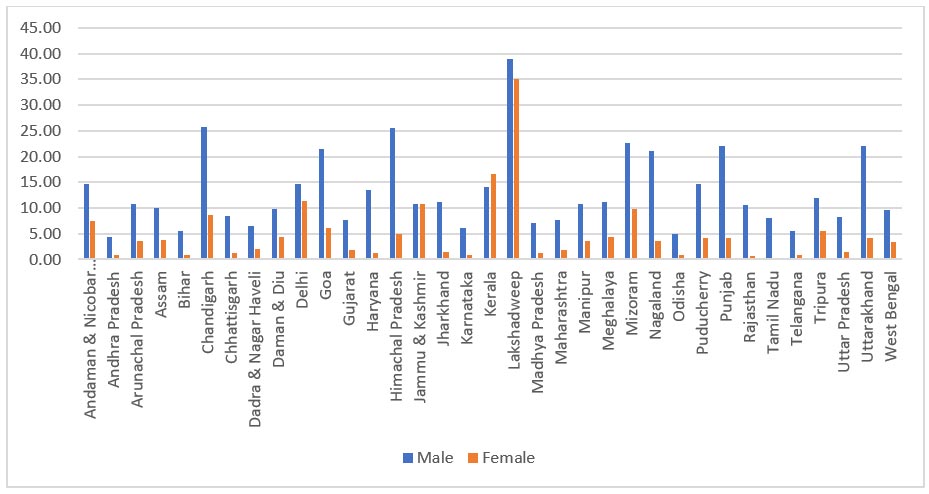
Figure 2 illustrates a consistent pattern of high self-reported rates of cardiovascular disease among elderly women, with a few exceptions in the northeastern states and union territories.
Figure 2: Self-reported Prevalence of CVDs, 60+ years
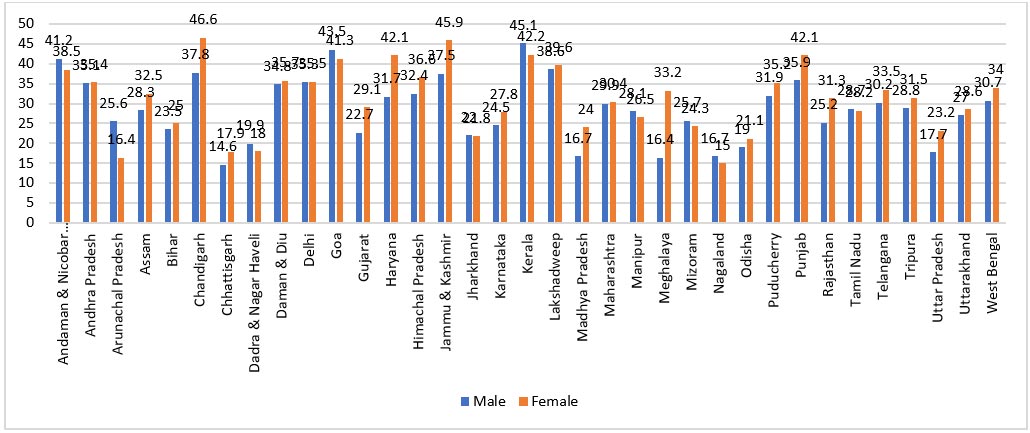
Source: LASI 2017-18 [56]
In India, a third of elderly people have hypertension, 5.2 percent suffer from chronic heart disease, and 2.7 percent have ever experienced a stroke.[57] Nearly 24.8 percent of all deaths in India, according to the Global Burden of Disease (2019),[58] are caused by CVDs. Data from Medical Certification of Cause of Death (2020)[59] also shows a significant rise in the percentage of deaths attributable to diseases of the circulatory system, which include diseases of pulmonary circulation, ischaemic heart diseases, cerebrovascular diseases, and hypertensive diseases. This increases notably for women 60 years and older.
Men’s CVD rates were higher in states like Kerala (45.1 percent of men compared to 42.2 percent of women), Goa (43.5 percent of men; 41.3 percent of women), and Andaman and Nicobar (41.2 percent of men; 38.5 percent of women) than in Chhattisgarh (17.9 percent of women; 14.6 percent of men) and Meghalaya (33.2 percent of women; 16.2 percent of men). The gender distribution was near-equal in states like Andhra Pradesh, Delhi, Jharkhand, and Tamil Nadu. The prevalence of CVD in women (33.2 percent) in Meghalaya was double that of men (16.4 percent).
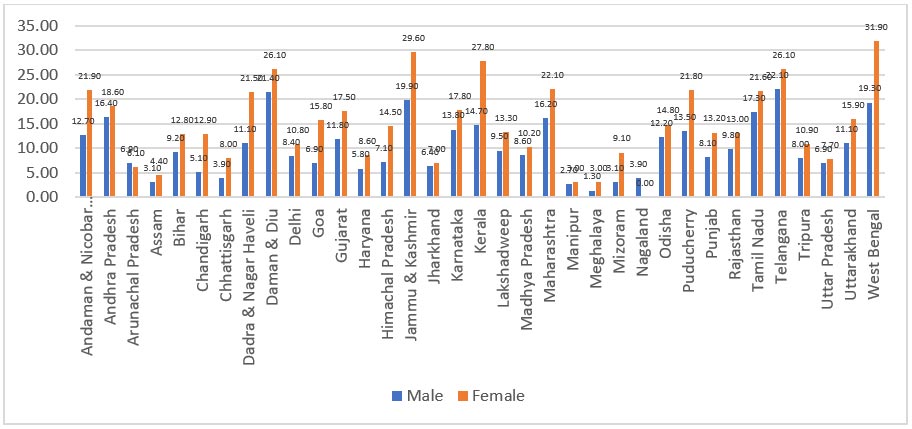
2. Anaemia
Anaemia is a prevalent medical condition among women of reproductive age.[b] Elderly women (aged 60 years or above) are more susceptible to the severe long-term impacts of anaemia compared to the younger demographic; these conditions can significantly lower their quality of life.[60] A study[61] among elderly women (60-92 years) in Delhi found almost 80 percent of them having anaemia. Studies also indicate a high prevalence of anaemia in both elderly men and women living in old-age homes in the national capital region,[62] and those in high-altitude regions.[63]
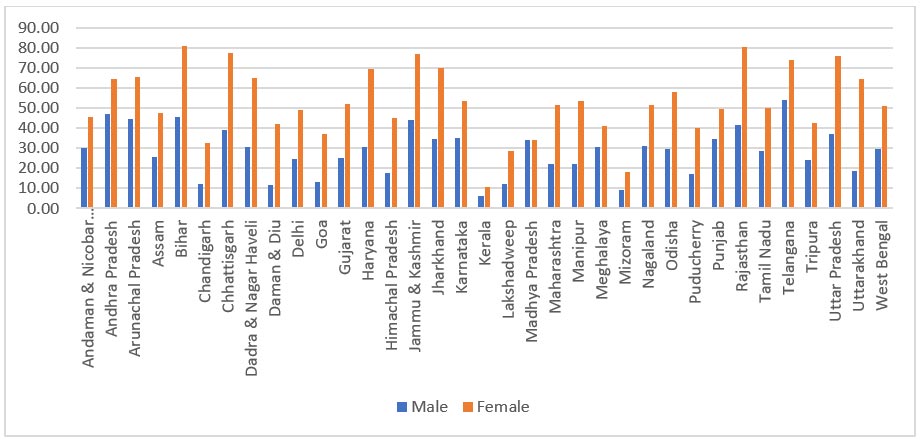
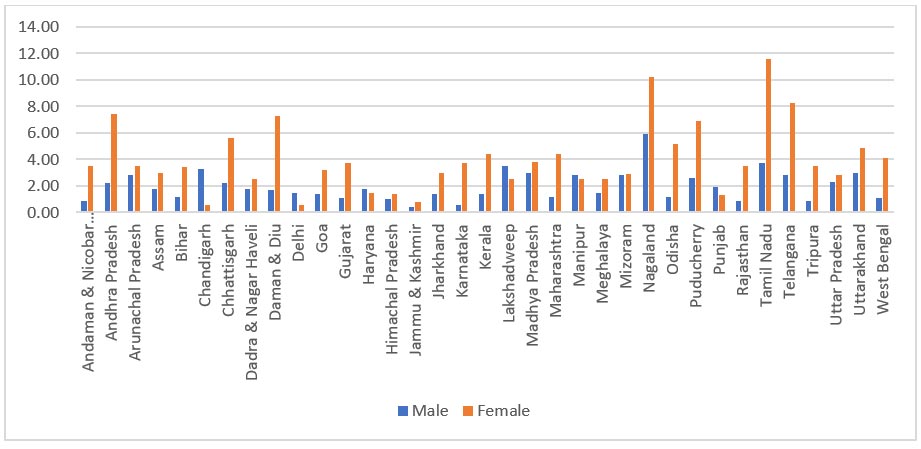
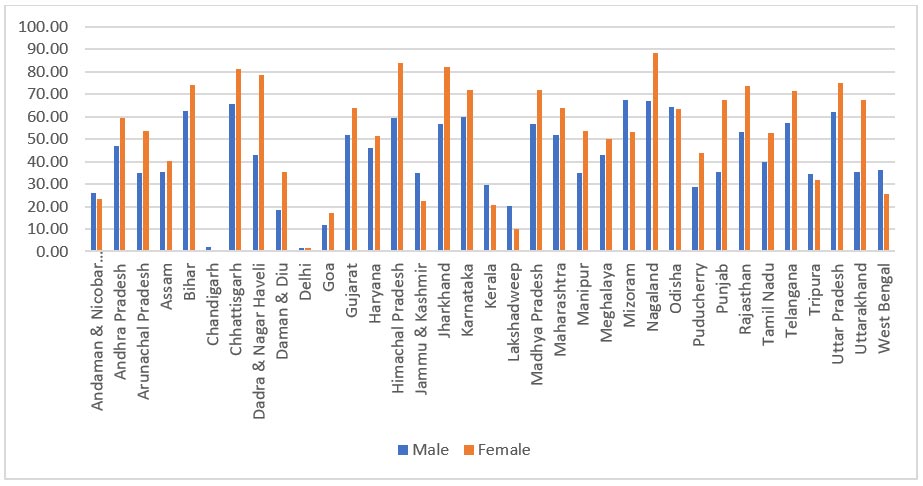
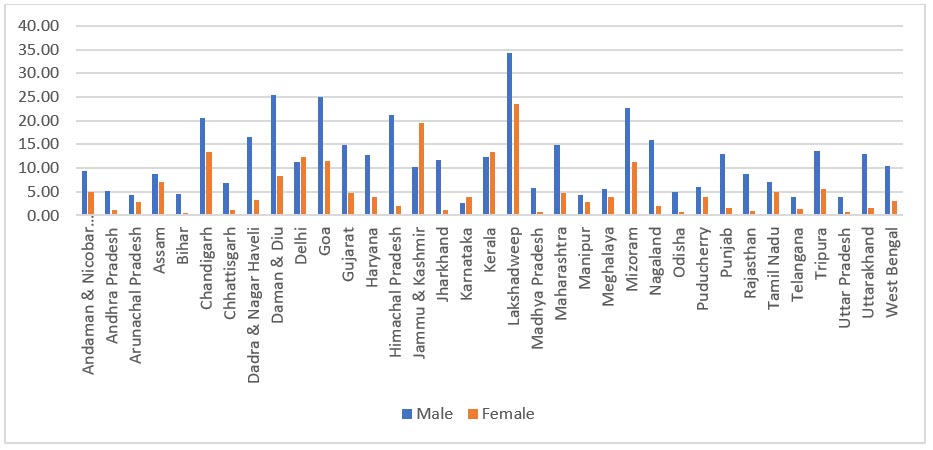
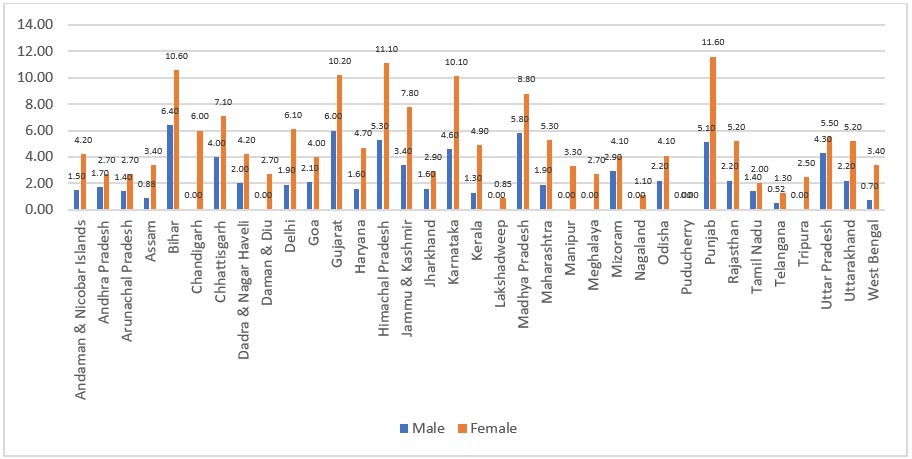
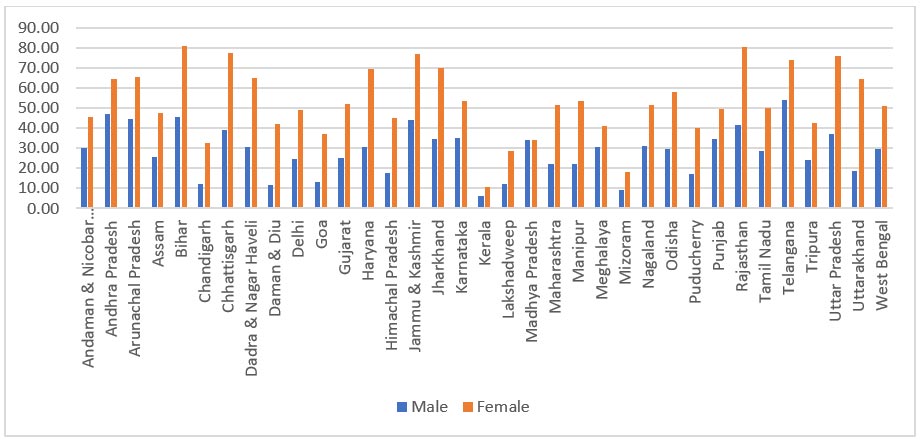
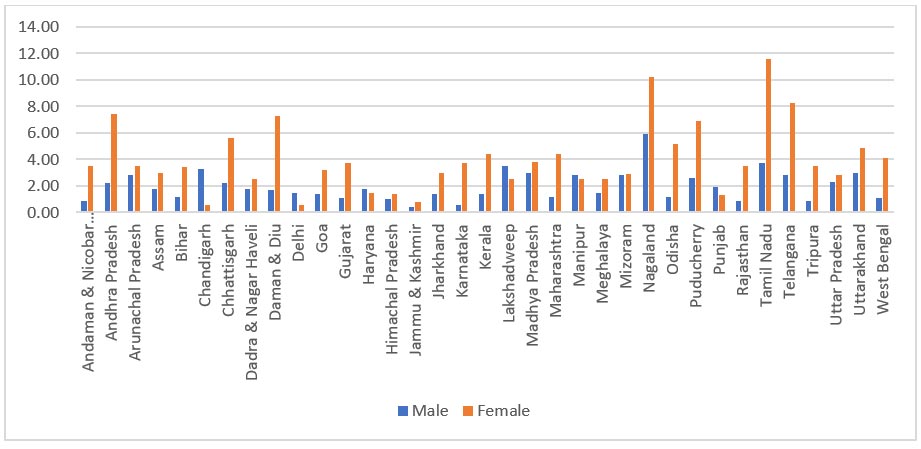
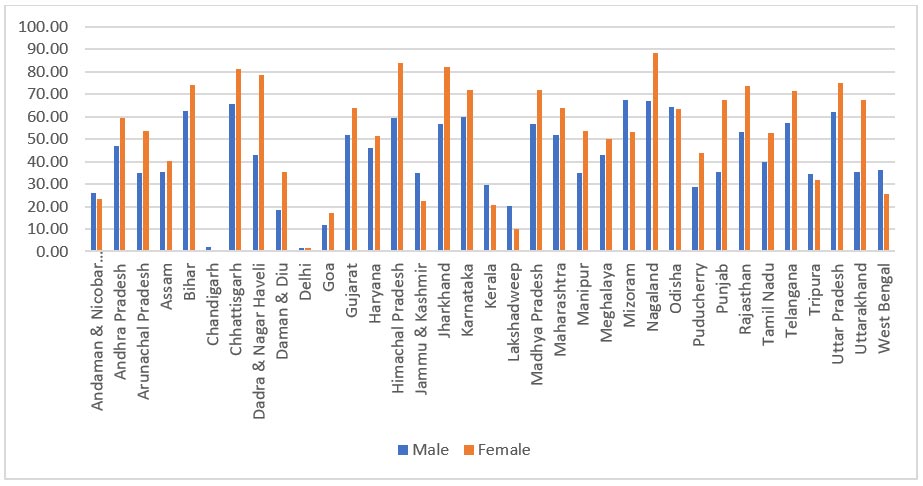
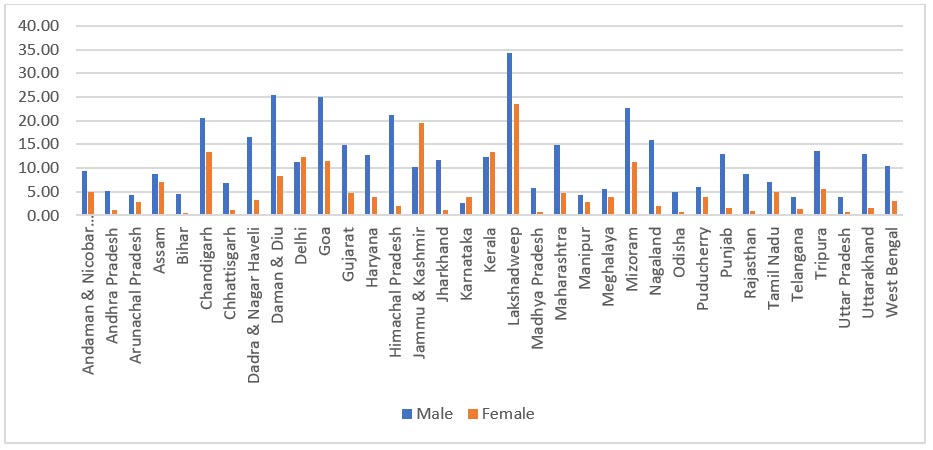
Figure 3: Self-reported Prevalence of Anaemia, 60+ years
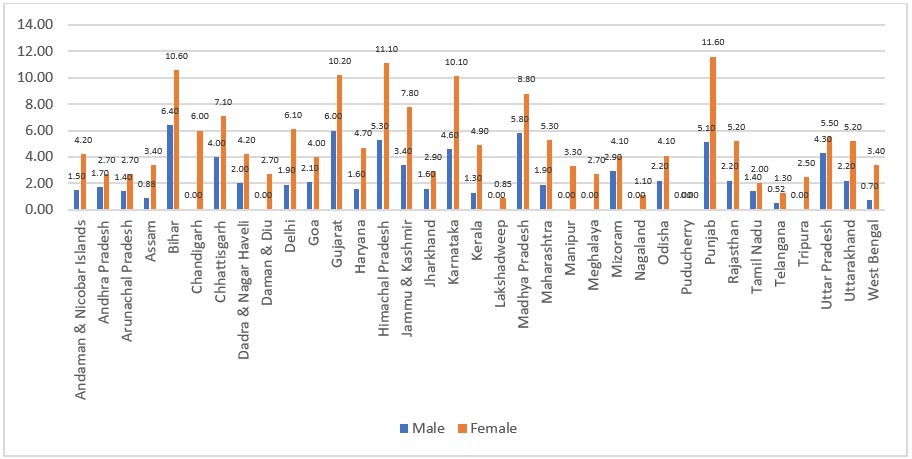
Source: LASI 2017-18
As the figure indicates, a larger proportion of elderly women than men reported being diagnosed with anaemia. The proportion of anaemic elderly women is almost double that of elderly men aged 60 and older in Bihar, Delhi, Goa, Himachal Pradesh, Jammu & Kashmir, Karnataka, and Punjab. In Chandigarh, Daman & Diu, Lakshadweep, and the northeastern states of Manipur, Meghalaya, Nagaland, and Tripura, anaemia were prevalent in elderly women. Overall, 5.9 percent of women compared to 3.1 percent of men among the elderly in India are anaemic.
The prevention of low birth weight, perinatal and maternal mortality, as well as susceptibility to disease later in life, depends on the treatment of anaemia in women of reproductive age. The NFHS-5 results show worrying trends with an increase in anaemia among women and children: 57 percent of women in reproductive age (15–49 years) and 60 percent of adolescent girls (15–19 years old).[64] This brings to focus the urgent need to tackle anaemia early on in women’s lives.
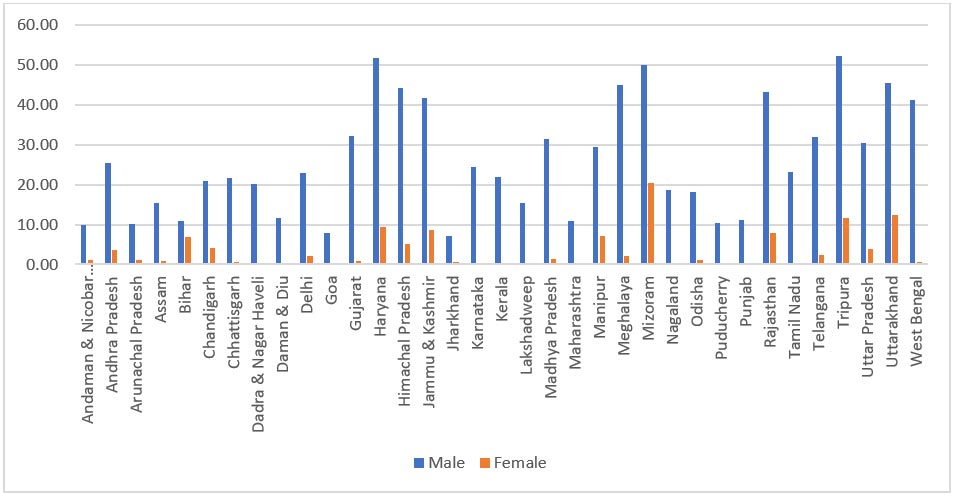
3. Hypertension
In a study of 80-year-olds and above in the urban districts of India’s southern states, there was an 83.5 percent prevalence of hypertension—81.6 percent among men and 84.7 percent among women, of which 64.5 percent was self-reported for both elderly men and women.[65]
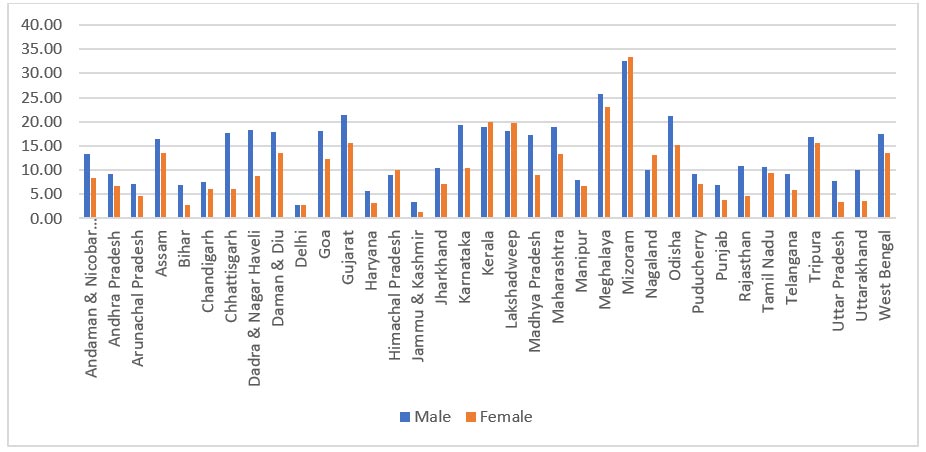
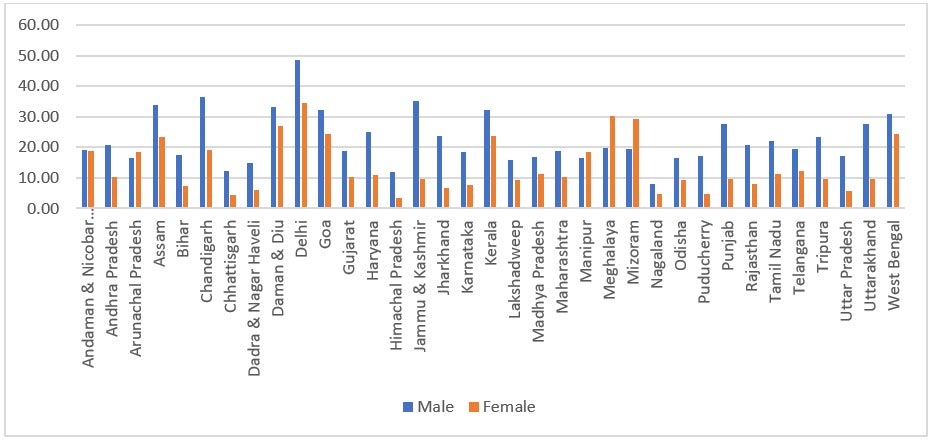
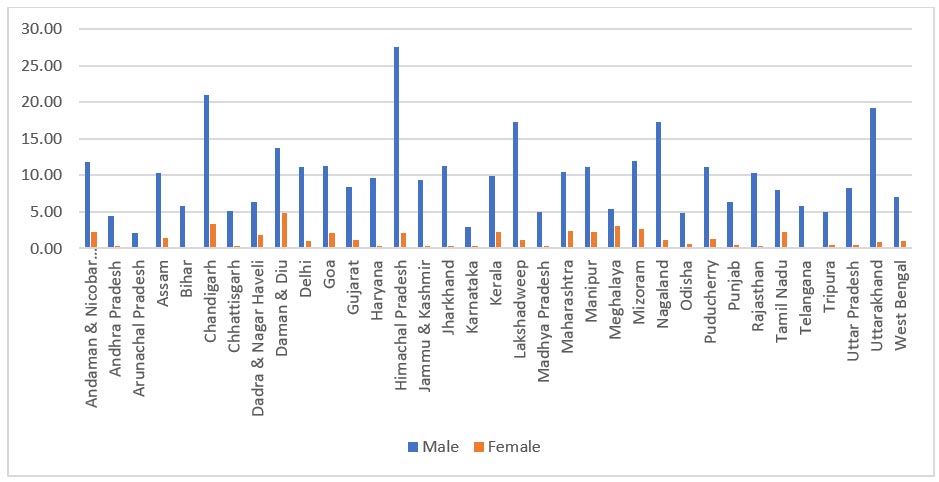
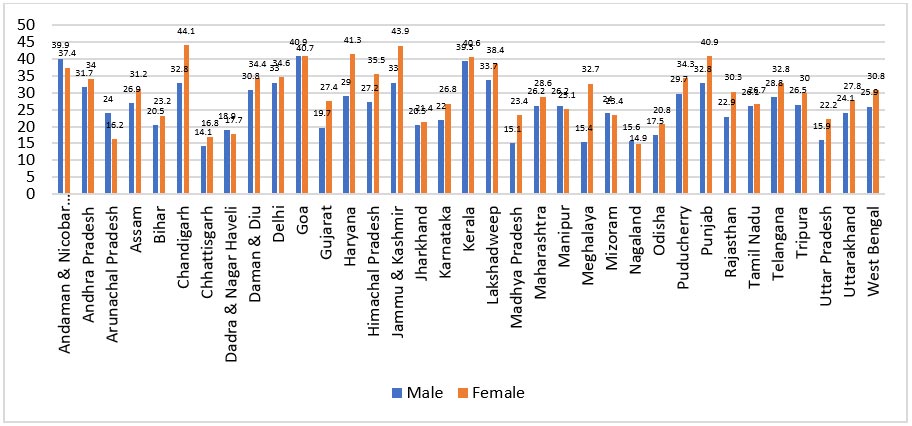
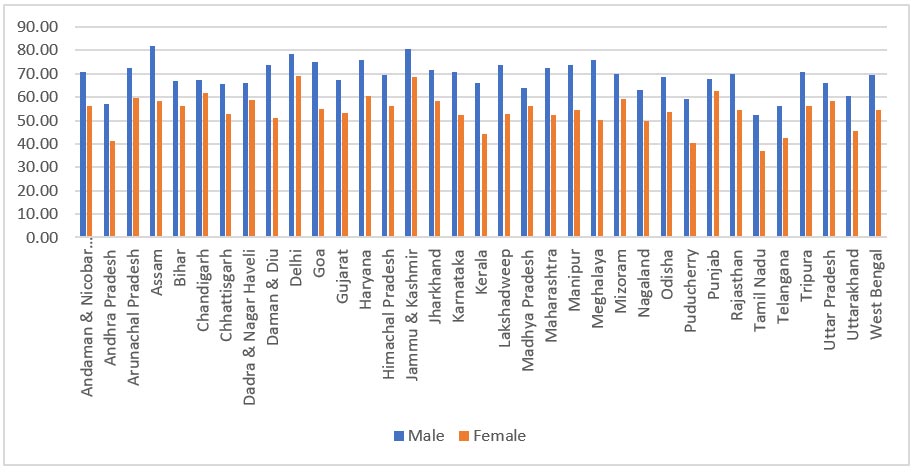
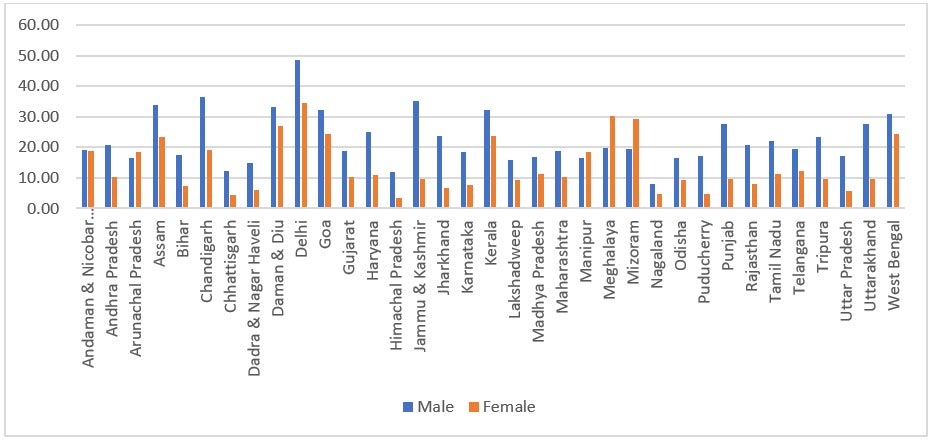
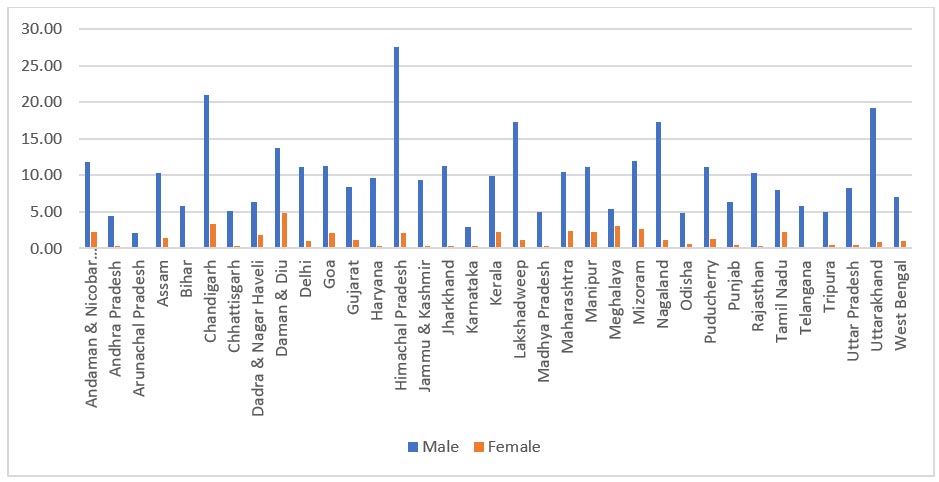
Figure 4: Self-reported Prevalence of Hypertension, 60+ years
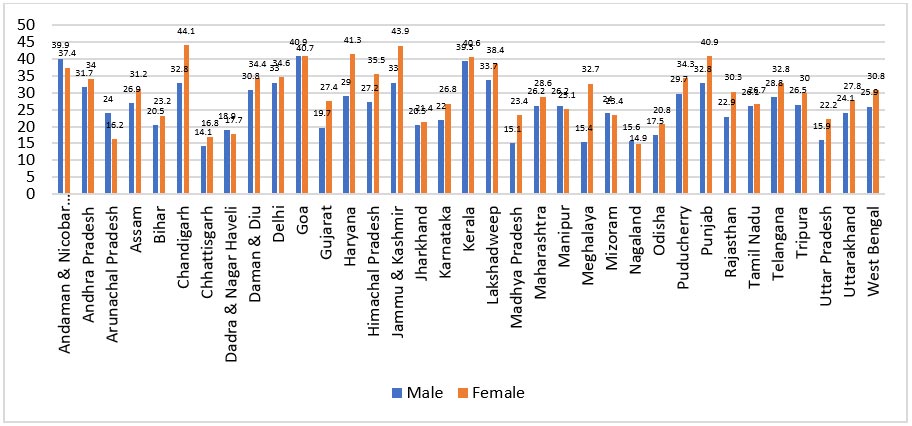
Source: LASI 2017-18
One in every three senior citizens in India has been diagnosed with hypertension.[66] Among older citizens, the prevalence was higher in women at 27.8 percent than in men (22.9 percent). Chandigarh had the highest percentage of women 60 years and older with the condition (44.1 percent) followed by Jammu & Kashmir, Haryana, Punjab, Kerala, and Goa. The lowest prevalence was found in Nagaland, at 14.9 percent.
A health ministry report, quoted in a 2021 issue of Down to Earth, noted an income factor in the prevalence of hypertension: in the highest quintile, 42 percent of senior people had been diagnosed with hypertension; the proportion was 25 percent of those in the poorest quintile.[67] In Mizoram and Bihar, where only around 50 percent of people received treatment, the hypertension rate was lower. Only one-fourth of the elderly population in Arunachal Pradesh who had been diagnosed with hypertension was receiving treatment. In Goa, Andhra Pradesh, Puducherry, and Kerala, more than 90 percent of the elderly were receiving treatment for hypertension. In Arunachal Pradesh, less than 10 percent were receiving the treatment.
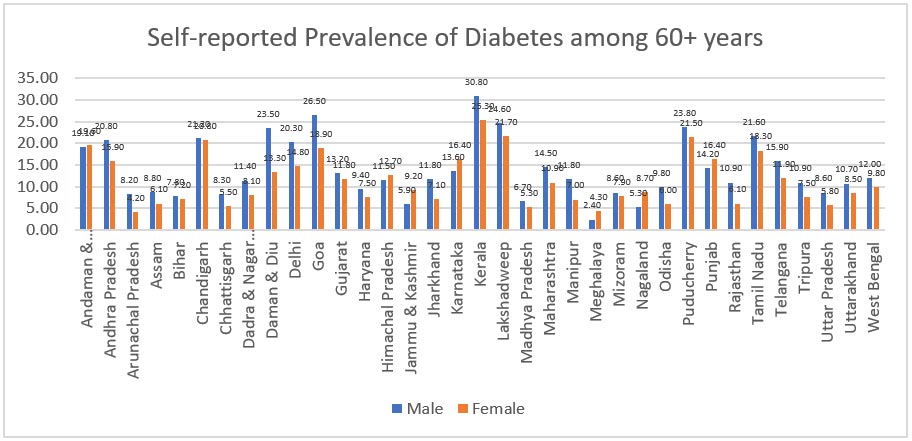
4. Diabetes
India is sometimes referred to as the “diabetes capital” of the world for the high prevalence rates of the disease, particularly in the metropolitan areas. The LASI estimates that the prevalence is higher among the older adults at 14.2 percent, than in people between the ages of 45 and 59 (9.2 percent).
While the prevalence of diabetes among elderly persons is not distinctly gendered, global research points that diabetes results in women being at a four times higher risk of heart disease (two times higher than in men) and more prone to worse outcomes in case of a heart attack.[68] Moreover, the relative risk of CVD mortality emerging from diabetes thus is 4.9 in women compared to 2.1 in men. While CVD usually presents approximately 10 years later in women than in men, the presence of diabetes almost fully offsets this gap. This also holds true for myocardial infarctions wherein they occur much earlier in women with diabetes.[69]
Further, a known high-risk factor for diabetes, overweight/obesity/higher BMI, despite decreasing from middle-age to old-age, is a more prevalent condition among elderly women than in men.[70] While it can be attributed to sex-related differences in risk factors and lifestyles, it puts women at an increasingly higher risk of developing diabetes and impaired fasting glucose levels.[71] Another risk factor—psychosocial stress and depression—was also notably higher among elderly women than men (26.2 percent of men vs 31.4 percent of women).[72] Therefore, while diabetes does not, prima facie, appear gendered, it causes far more adverse outcomes among elderly women.
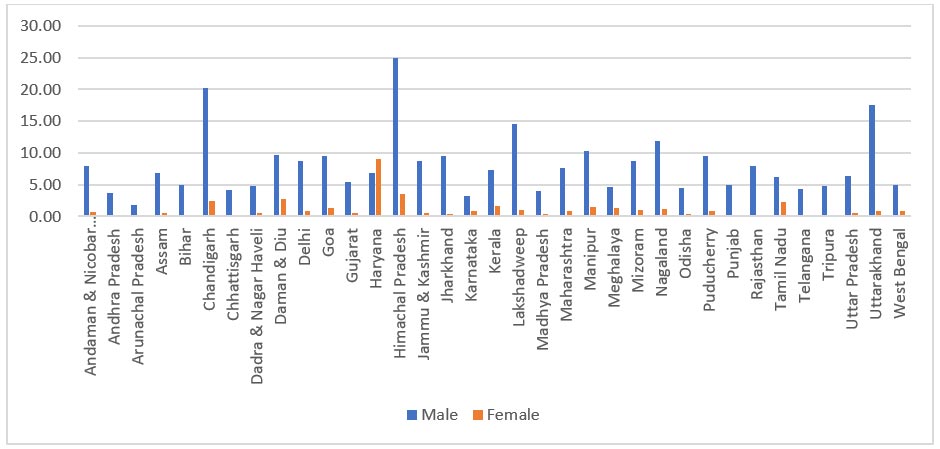
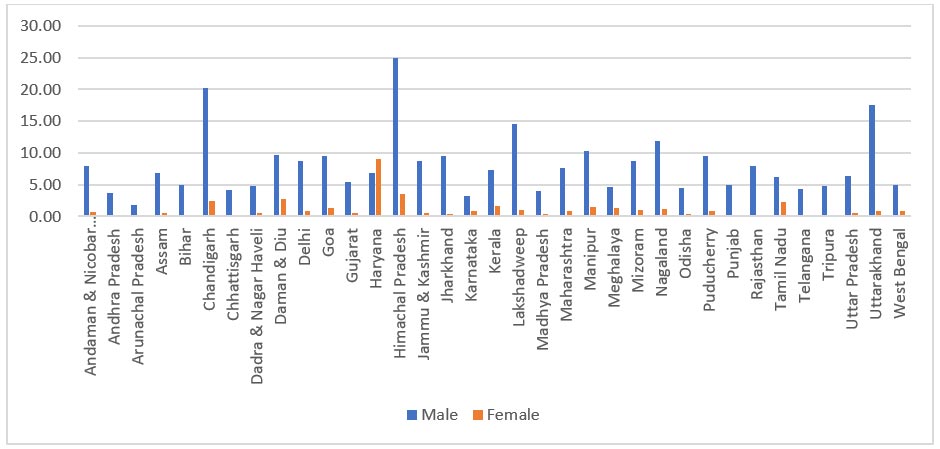
As per LASI, 10.8 percent of older women have self-reported prevalence of diabetes mellitus compared to 12.4 percent of men. Sub-nationally, self-reported prevalence among women is higher in the states of Kerala, Chandigarh, and Tamil Nadu and the union territories of Andaman & Nicobar and Lakshadweep Islands.
Figure 5: Self-reported Prevalence of Diabetes, 60+ years
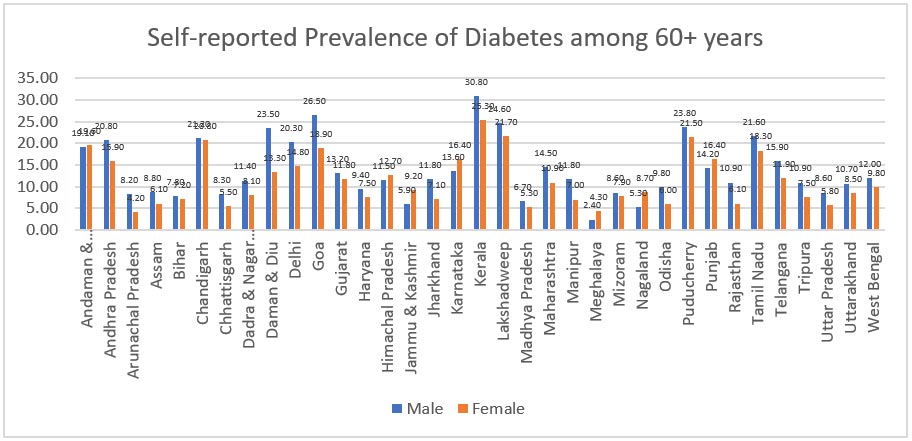
Source: LASI 2017-18
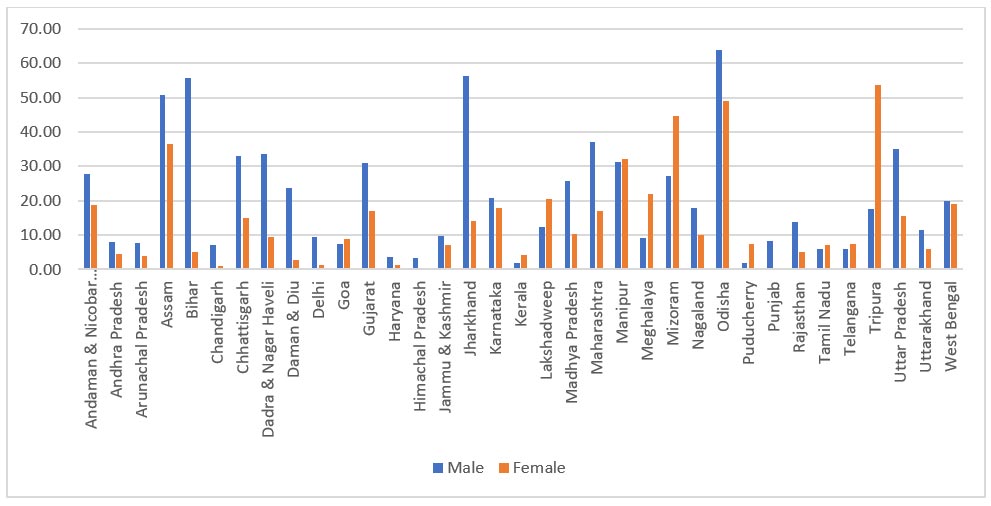
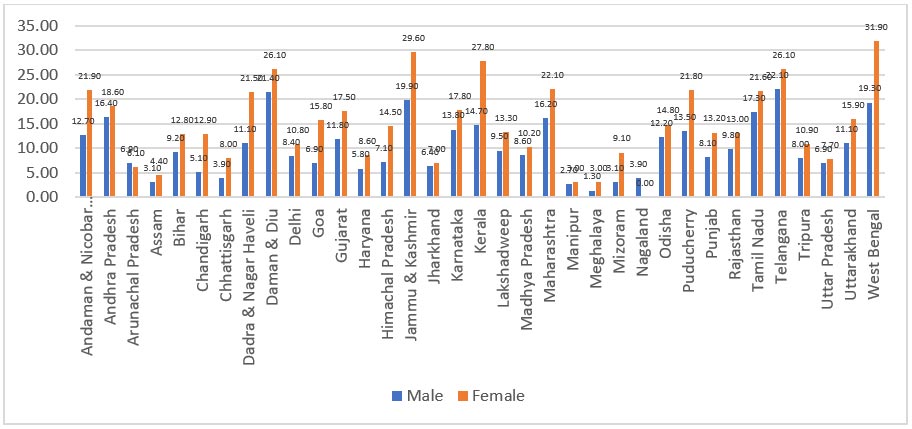
5. Bone and Joint Diseases
With a prevalence of 22-39 percent, osteoarthritis (OA) is among the most prevalent joint diseases and the second most prevalent rheumatologic condition in India.[73] While 70 percent of people over 65 display radiological signs of OA, a significant 45 percent of women experience symptoms. This is a major contributor to impairment in mobility, subsequently also increasing the risk of obesity due to sedentary lifestyles.[74] These conditions are likely to be caused by vitamin D deficiency, swelling in joints, bone degeneration, and tumours.
LASI reports gender-disaggregated data for osteoporosis (0.9 percent for men; 1 percent for women), arthritis (9.9 percent for women; 7.1 percent for men), and bone and joint diseases (16.9 percent for women; 12.3 percent for men). Moreover, the prevalence of chronic pains was higher among women (nearly 33 percent) compared to men (almost 25 percent).
Social, demographic, environmental, lifestyle and health-related variables influence the occurrence of disorders of the bones and joints. For instance, older adults are more likely to die or suffer major injuries as a result of physical, sensory, and cognitive changes brought on by ageing.[75]. Older women also reported a higher incidence of injuries and falls compared to their male counterparts. At the same time, as shown in NSS data, hospitalisation due to injuries is higher among elderly males compared to females.[76] The disparity in health treatment-seeking behaviour between men and women needs to be explored.
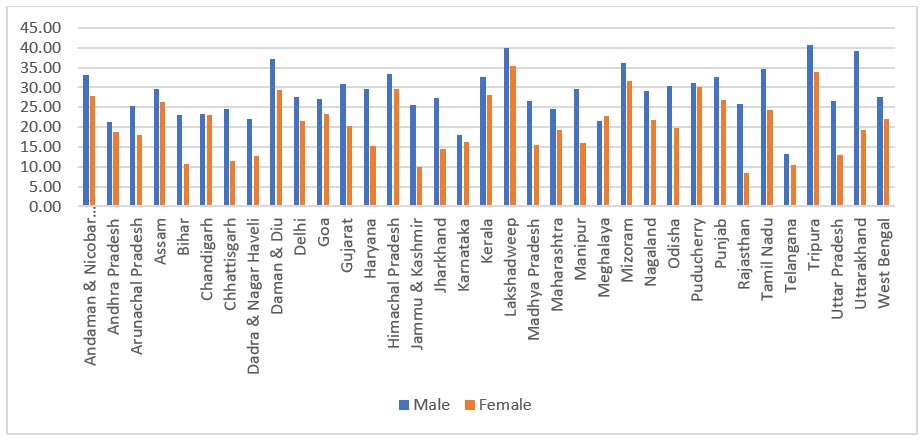
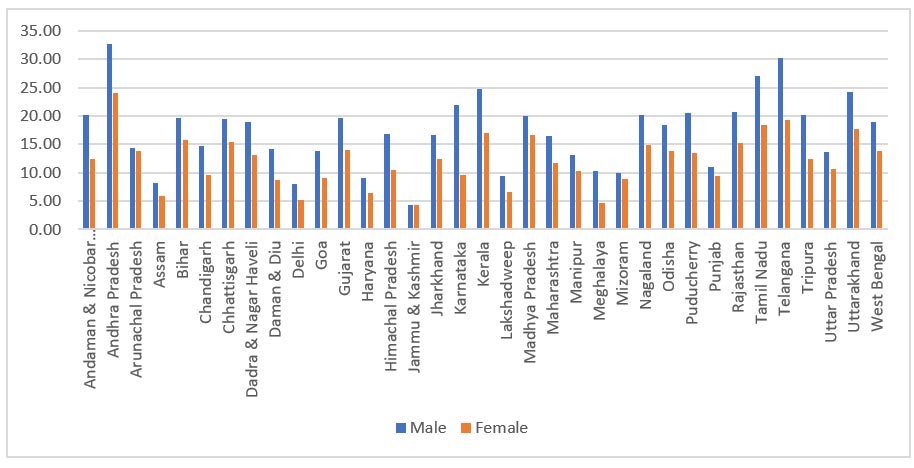
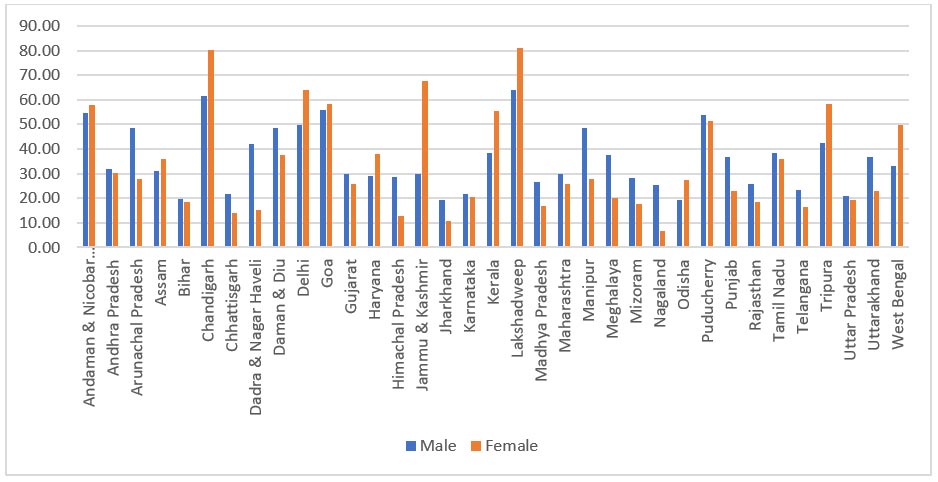
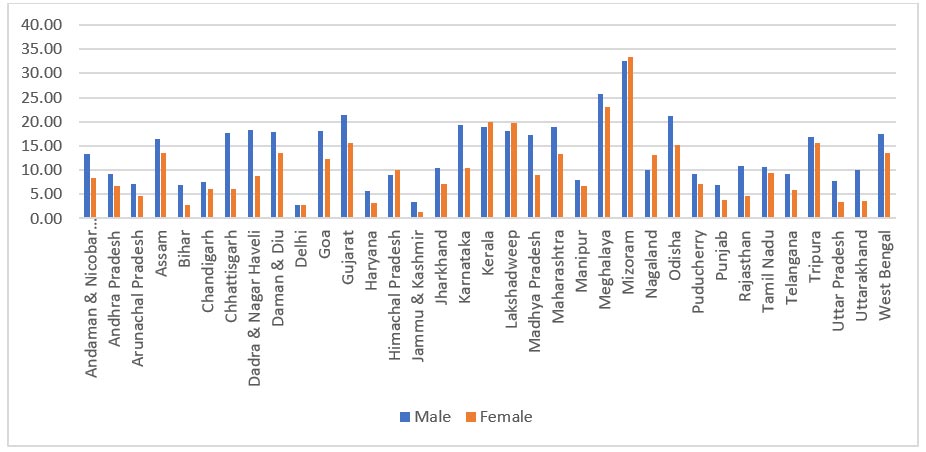
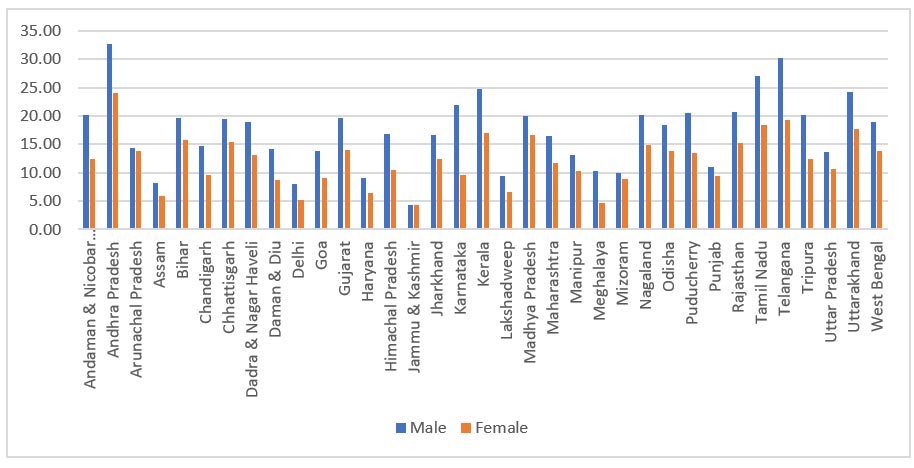
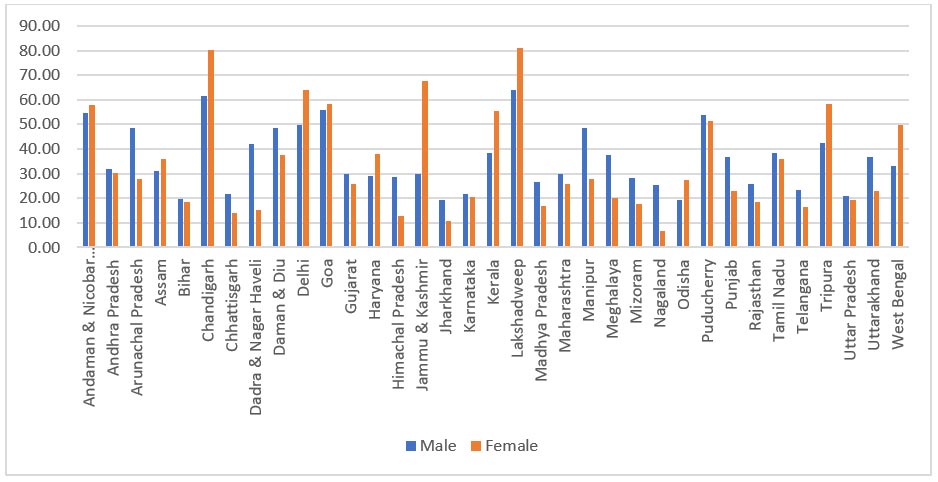
Figure 6: Self-reported Prevalence of Bone & Joint Diseases, 60+ years
Source: LASI 2017-18
Bone or joint diseases appear to be more prevalent in elderly women than in elderly men. The highest prevalence was seen in West Bengal at 31.9 percent of older women, followed by Jammu & Kashmir, Kerala, Daman & Diu, and Telangana. The lowest was in Manipur and Meghalaya at 3 percent of older women. The biggest gaps in the prevalence rates of bone and joint diseases between elderly males and their female counterparts were recorded in Kerala (27.8 percent in elderly women; 14.7 percent in elderly men), and West Bengal (31.9 percent in elderly women; 19.3 percent for elderly men).
The Role of Social Determinants
Social determinants shape the distribution of the four main behavioural risk factors of NCDs—i.e., unhealthy diet, physical inactivity, tobacco use, and excess alcohol consumption—and three physical conditions that are risks for NCDs—raised blood pressure, obesity, and diabetes. Other social determinants of health include job environment, family and social support, and educational attainment.
This section uses sub-national data from LASI 2017-18 to examine the role of socio-demographic variables in influencing one’s health.
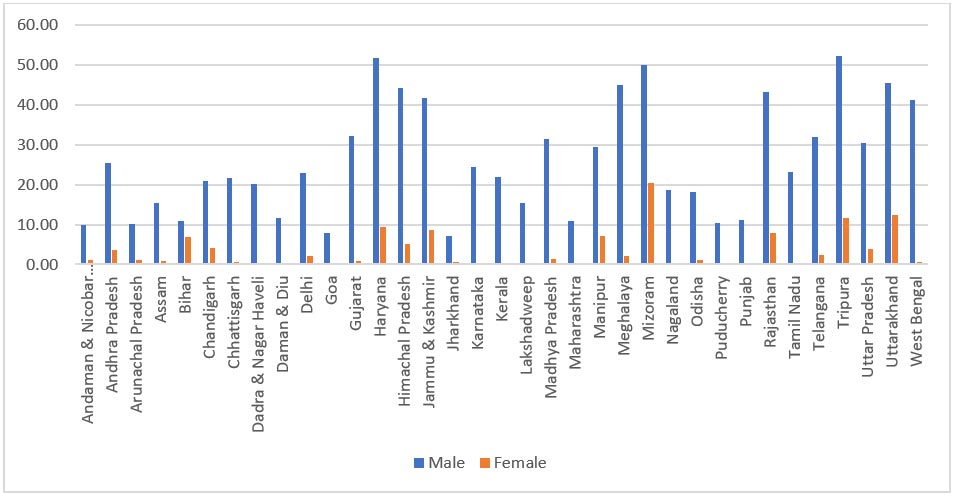
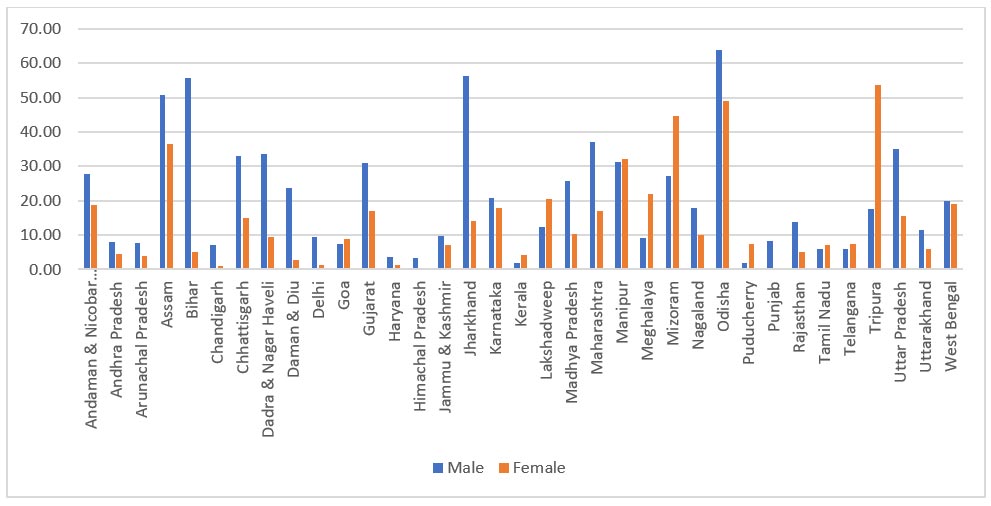
Smoking, Tobacco Use, and Heavy Drinking
Most non-communicable diseases are caused by four specific lifestyle-related risk factors: tobacco use, physical inactivity, poor diet, and alcohol abuse. These result in four crucial metabolic and physiological changes: elevated blood pressure, overweight/obesity, elevated blood glucose, and elevated cholesterol,[77] all of which enable pathways for more adverse outcomes from NCDs. A 2016 study of the urban population in Indonesia found that women’s progression towards old age resulted in a greater risk of high blood pressure, obesity, and elevated cholesterol levels, while men were more likely to be current smokers and have a propensity to have high blood pressure at a younger age.[78] A 2019 study from Thailand shows that among women, the risk of high blood pressure and high triglyceride levels are linked to a higher likelihood of heavy alcohol consumption.[79]
In 2017, the Lancet Global Health reported that in low-income and lower-middle-income countries, women were more likely to chew, and men smoke.[80] While there has been a decrease in the prevalence of smokeless tobacco[c] among women in India from 2009 to 2016, tobacco control efforts need to be sustained.[81]
A study on older adults from select Indian states found older age, women, higher socioeconomic status, tobacco and alcohol users more likely to have multimorbidity compared to those with no NCD.[82],[83] In the most visible forms, gender gap in risk factors like smoking, tobacco consumption, and heavy drinking continue to remain significantly skewed towards men, even in old age. The data further shows that gender gap in tobacco consumption trend in the north-eastern region remains minimal, almost equal, in contrast to the rest of the country.
Figure 7: Prevalence of Smoking, 60+ years
Source: LASI 2017-18
Among older adults, 25.8 percent of men smoke, compared to 2.4 percent of women. Smoking was high in the hilly and northeastern states like Mizoram, Tripura, Jammu & Kashmir, Uttarakhand, and neighbouring states of Haryana and Rajasthan. Similarly, only 0.5 percent of elderly women in India report engaging in heavy drinking, against 6.2 percent of men. Sub-nationally, no state had a higher percentage of elderly women involved in heavy drinking compared to men, but it was notably higher in the northeastern region including in the states of Arunachal Pradesh and Manipur, and the south-eastern region of Jharkhand, Telangana, and Odisha (Figure 9). Tobacco consumption was at 27.9 percent of elderly men and 13.9 percent of elderly women.
Figure 8: Prevalence of Tobacco Consumption, 60+ years
Source: LASI 2017-18
Figure 9: Prevalence of Heavy Drinking, 60+ years
Source: LASI 2017-18
Education level
Studies among the older adults in varied countries including Sweden, India, China, and Canada have found that men are more likely to report better self-rated health compared to women.[84],[85],[86],[87] Meanwhile, a 2017 analysis of European countries suggested that gender differences in health status among the elderly can also be attributed to varying levels of educational attainment, among other factors.[88] In India, LASI further revealed that, among elderly women, higher levels of education are associated with lower prevalence rates of NCDs owing to greater awareness about preventive measures.
A 2011 study in Germany said that the relative risk of diabetes among women decreased with education.[89] This continues to hold true in India as well, as studies have found a correlation between lower educational levels and lack of awareness of dietary risks or requirements, and then translating to a higher prevalence of diabetes.[90] In Japan, a 2019 study of middle-aged men and women observed that, in women, the prevalence of diabetes, heart disease, stroke, hypertension, and cancer decreases with higher educational levels.[91]
In low- and middle-income countries, there is evidence that socioeconomic circumstances have an impact on behavioural risk factors for NCDs. In India, poor overall literacy may correlate to lower health literacy. At the same time, among older adults, those in the higher-income brackets had a higher risk of hypertension and twice the risk of heart problems.[92]
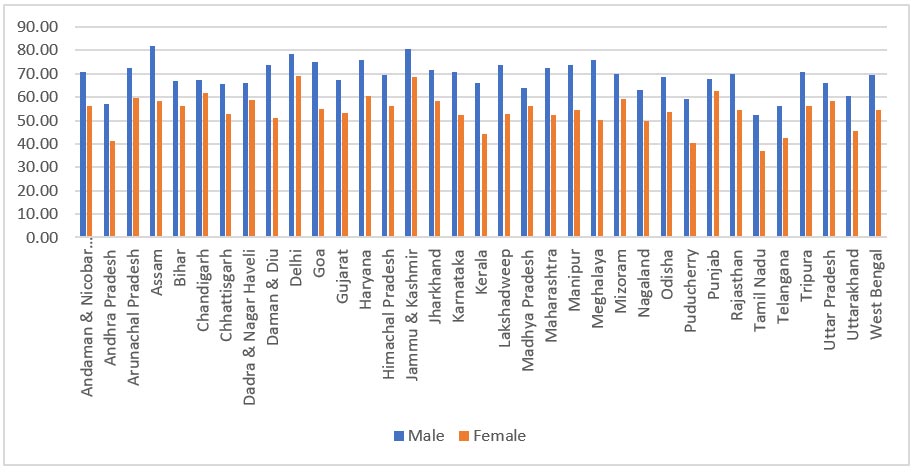
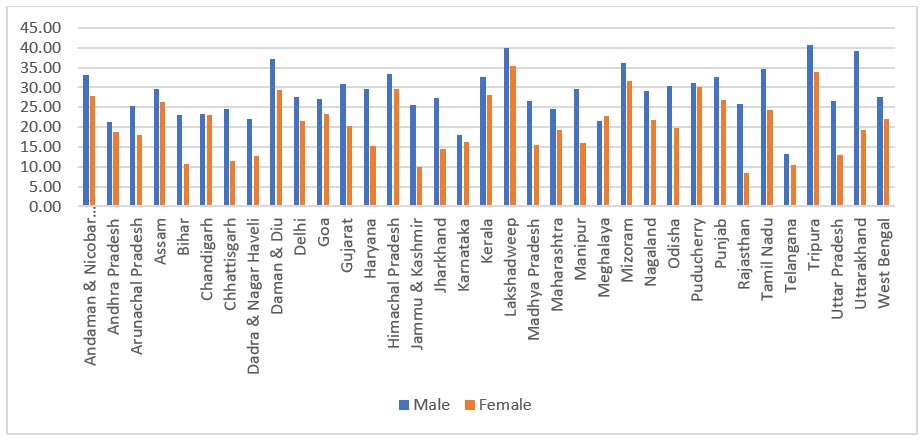
Figure 10: Education Level, 60+ years, by Gender: No Schooling
Source: LASI 2017-18
Figure 11: Education Level, 60+ years, by Gender: Schooling < 5 Years
Source: LASI 2017-18
Figure 12: Education Level, 60+ years, by Gender: 5-9 Years of Schooling
Source: LASI 2017-18
Figure 13: Education Level, 60+ years, by Gender: 10 or More Years of Schooling
Source: LASI 2017-18
Following the overall population-level trend, women have a lower education level compared to men sub-nationally. This is evident in the categories of less than 5 years, 5-9 years (Figure 12), and more than 10 years of schooling (Figure 13). The proportion of elderly women without any schooling is notably higher compared to men.
Familial Support
Social networks and families play a significant role in managing care for chronic and lifestyle diseases. Studies from China establish that self-rated health and economic status are key to the perceptions of life satisfaction among the elderly.[93] Sense of companionship, a good relationship with the spouse, perceived safety at home, and a supportive social network were noted to be vital in enhancing life satisfaction.[94] Older Hispanic immigrants in the United States, too, were more likely to have better self-health ratings when they were experiencing lesser functional limitations.[95] Further, support from family members, especially for diabetes, hypertension, and other NCDs, has been known to ensure adherence to medication, better detection of undiagnosed conditions, and behaviour management, which lead to better health outcomes.[96] This support also increases primary prevention of NCDs early on.
In India, families similarly remain the central unit for providing economic and caregiving support to older people. Analysis from the LASI data reveals that living with a spouse and children not only improves life satisfaction but also enables better management of existing morbidities. According to available data, 4.5 percent of elderly women live alone; the proportion for elderly men is 1.8 percent. The LASI report shows that approximately 30 percent of women above the age of 60 are widowed, compared to 10 percent of their male counterparts. This can be potentially explained by the lower life expectancy of males and the typical practice of women marrying men older than them. Widows, compared to widowers (48.5 percent vs 44.8 percent) have a higher prevalence of non-communicable multi-morbidities. This gender disparity in widowhood among the older adult population renders women particularly vulnerable as it can lead to limited inheritance rights and access to property, restrictions, and stigma in social interactions, which may consequently lead to depleted incomes and economic vulnerabilities.
Further analyses of the LASI datasets also reported that older adults are less likely to have close friends compared to their younger counterparts. Elderly women are even less likely to report having close friendships.[97] Moreover, the dependency on children for living arrangements was significantly higher for women at 24.4 percent, compared to only 8.6 percent for men. This can be potentially explained by the lower economic status and lower wealth accumulated by women in their lifetime. Men, across all states in India, live with support from spouses and children, compared to women.
Figure 14: Living Arrangement, 60+ years, by Gender: Living Alone
Source: LASI 2017-18
Figure 15: Living Arrangement, 60+ years, by Gender: Living with Spouse
Source: LASI 2017-18
Figure 16: Living Arrangement, 60+ years, by Gender: Living with Spouse and Children
Source: LASI 2017-18
A higher percentage of elderly men than women in all states and UTs live with either their spouse or children.
Figure 17: Living Arrangement, 60+ years, by Gender: Living with Others
Source: LASI 2017-18
Figures 15, 16, and 17 show clear sub-national patterns where a higher proportion of elderly women compared to elderly men, in most states, live with others not their spouse or children. The northern states of Uttar Pradesh, Himachal Pradesh, and Punjab, Delhi, and the UT of Dadra and Nagar Haveli are the only exceptions to this trend.
Similarly, with the exception of Haryana and the neighbouring UT of Chandigarh, nowhere in India is there a higher percentage of men above 60 years living alone.
Work Engagement and Social Protection
Engagement in economic activities is known to positively impact economic and social well-being for the elderly. Not only do elderly women suffer from poorer health conditions than their male counterparts, they also have less access to healthcare services. Roy and Chaudhari (2008) in their study showed that the probability of hospitalisation is considerably lower in elderly Indian women than in men.[98] They further contend that poorer health, as well as poorer access to healthcare among elderly women as opposed to men, can be explained by gendered differences in socio-economic status; elderly women tend to have less financial independence than men. Their study also indicates that empowering the elderly in India financially would reflect equal or better health outcomes among women. Another study in a rural setting found that diabetes and hypertension were much higher in elderly women who were unemployed.[99]
To the extent that the space of employment and labour is highly gendered, there exists a linkage between the nature of occupation and the burden of NCDs among elderly women. Certain arenas of work like agricultural activities are dominated by women, whereas businesses, markets, and organised sector employment has historically been dominated by men.[100]
The national level data shows that 62.6 percent of women compared to 51.7 percent of men are engaged in agricultural and allied activities. The mean monthly individual income generated by men is INR 6,157, compared to a far lower INR 3,840 for women. This significant parity is visible for the categories of non-agricultural business activities (INR 10,513 for men vs INR 5,225 for women) and wage and salary workers (INR 13,338 for men vs INR 7,514 for women) as well.
Figure 18: Work Engagement, 60+ years, by Gender: Agriculture & Allied Activities
Note: Agricultural work includes cropping, forestry, livestock & fishery, working for own or family’s or for other people’s farm/ fishery/ forestry.
Source: LASI 2017-18
As seen in Figure 18, in a general trend across the country, women are more represented in unorganised sectors, especially in agricultural and allied activities which are considered an extension of their domestic duties. The exceptions are Kerala, West Bengal, and Mizoram, along with the islands of Andamans and Lakshadweep, and hyper-urban geographies of Delhi and Chandigarh. This sporadic distribution needs further investigation.
Figure 19: Work Engagement, 60+ years, by Gender: Non-agriculture & Business Activities
Note: Non-agricultural business activities include own account worker, i.e., self-employed without employees or non-agricultural business owners.
Source: LASI 2017-18
In contrast to agricultural activities, business-related work (Figure 19) is dominated by men in almost all states. Historical under-representation, lower market penetration, and poor financial literacy are some of the key reasons that prevent women from participating in business activities. The northeastern states of Meghalaya, Mizoram, Manipur, and Arunachal Pradesh are the only states exhibiting contrary trends in economic engagements for elderly women.
Among the elderly in India, access to employer insurance and pension schemes is available to a mere 9 percent of rural males and 41.9 percent of males in the formal sector in urban areas. It is still lower among females—3.9 percent in rural areas and 38.5 percent in urban areas. The remainder of the workforce comprise casual or self-employed workers, who have no access to retirement or healthcare benefits.[101]
Figure 20: Work Engagement, 60+ years, by Gender: Wage & Salary workers
Note: Wage & salary work includes full-time, part-time, contract-based, temporary, or seasonal employment
Source: LASI 2017-18
LASI data indicates that only 1.9 percent of elderly women, compared to 8.4 percent of elderly men were covered by work-related pension schemes. Apart from Kerala, all states have a significantly lower proportion of women retiring out of the organised sector (Figure 21). The provident fund coverage, too, is 2.8 percent for women compared to 7.3 percent for men at the national level.[102]
Social protection mechanisms play a significant role in preventing catastrophic health outcomes as a consequence of high out-of-pocket expenditures or lack of welfare or monetary protection such as health insurance. Data from LASI points out that only 3.2 percent of elderly women used health insurance to finance their latest hospitalisation, compared to nearly double of elderly men despite near equal insurance coverage. While this can be potentially explained by poor financial literacy and lower organised sector jobs among women, it will need further exploration. Further, statistical analysis of LASI data found that individuals with health insurance were also at a higher risk of multi-morbidities. With each additional morbidity, out-of-pocket expenditure also increased.[103]
Figure 21: Social Protection Coverage, 60+ years, by Gender: Work-related Pension Scheme
Source: LASI 2017-18
Figure 22: Social Protection Coverage, 60+ years, by Gender: Provident Fund
Source: LASI 2017-18
Figure 23: Social Protection Coverage, 60+ years, by Gender: Retired from Organised Sector
Source: LASI 2017-18
As seen in Figure 23, the representation of women in the workforce remains dismal at the age of retirement. The data indicates that except for Haryana (Figure 24), elderly women are barely receiving any retirement pension.
Figure 24: Social Protection Coverage, 60+ years, by Gender: Currently Receiving Retirement Pension
Source: LASI 2017-18
Overall, it can be seen that social protection is notably higher in smaller states and UTs. The northern, eastern, and central Indian states have performed poorly in this criterion.
The Impact of COVID-19
The first wave of the COVID-19 outbreak in India saw a higher mortality risk amongst the older population, especially in those with pre-existing comorbidities and requiring special care in case of infections.[104] Evidence from 2020 indicated that elderly males had a higher overall burden, but elderly females had a higher relative risk of COVID-19 mortality.[105]
Studies from 16 countries revealed that persons aged 65 or older had remarkably higher mortality rates from COVID-19 compared to younger individuals.[106] Further, men had a higher risk of COVID-19 death than women. Countries like Colombia and Chile had as high as 86 percent of all deaths amongst the elderly.[107] Seventy percent of Peru’s deaths are accounted for by the older adult population 60 and above.
While the proportion of elderly in India is comparatively lower than in other developed nations, structural flaws and poor social protection leave them vulnerable. There is relatively lesser financial aid allotted to their care, limited geriatric health infrastructure, and scarcity of outreach activities. Nearly 70 percent of the elderly population depend on others for their day-to-day needs as per the NSS analysis from 2017–18.[108] In crises like the COVID-19 pandemic, they are bereft of social connections and care. Their stresses are amplified by their limited fluency in digital tools, which are being utilised in response measures to health emergencies.
Another concern was the far-reaching vaccine hesitancy among the elderly in India. In Tamil Nadu, for instance, 27.6 percent of the older adult population were not willing to be vaccinated against COVID-19.[109],[110] The hesitancy was found to be higher amongst the elderly men. Nagaland, another state that grappled with hesitancy and misinformation, had the country’s lowest first-dose coverage of the vaccine in 2021. The poor acceptance of vaccines is more pronounced in the 45+ years age bracket and in districts of high illiteracy.[111]
A critical public health concern among the older population is NCDs with comorbid mental disorders.[112] Available evidence indicates that mental disorders pose a risk for the emergence of other NCDs.[113],[114] In addition to alcohol and tobacco use, patients with mental disorders frequently have poor eating habits and low levels of physical activity, all of which increase their risk of developing medical comorbidities,[115] including coronary artery disease, stroke, and cancer, as well as obesity, hypertension, and metabolic syndrome.
Recommendations and Conclusion
This paper attempted to present a holistic and in-depth literature review on the incidence and risk of NCDs among the elderly. It sought to highlight the gendered impact of ageing in biological, sociological, and economic terms. This necessitates that policies push gender to the mainstream of health systems response to combatting NCDs in the country. Further, age remains a key hindrance to the accessibility of health services. To promote healthy ageing, it is vital to concentrate on preventive strategies that postpone the onset and stop the progression of NCDs. It is crucial that geriatric and long-term care is incorporated into the health system to ensure continuity of care and necessary gender-budgetary considerations be integrated into national plans.
Recommendations
- Targeted interventions are needed to tackle gender inequalities within healthcare systems and create gender- and age-sensitive policies with a special focus on the needs and use-trends of the elderly.
- Taking cognisance of the population-level trends of non-communicable diseases in the elderly, there should be renewed attention to improving health education and awareness along with preventive regular health checkups and screenings. Creating awareness of physical and mental well-being and regular screenings for these diseases can enable early prevention and detection, and better management.
- As the elderly population is growing, there is a need for workforce capacity building for healthcare professionals in dealing with the needs of the elderly.
- Collaboration and partnership between government agencies, non-government organisations, healthcare providers, and community-based organisations should be prioritised to create a holistic approach to addressing gendered NCD prevalence among the elderly.
Mona is Junior Fellow at ORF.
Shoba Suri is Senior Fellow at ORF.
The authors acknowledge the research assistance provided by Sajusha Ashok of Indian Institute of Technology, Madras, who was an intern with the Health Initiative at Observer Research Foundation.
Endnotes
[a] The National Policy on Senior Citizens (2011) defines a person 60 years and above as elderly.
[b] ‘Anaemia’ is defined by WHO as having haemoglobin levels of 12 g/dl.
[c] Smokeless tobacco includes chewing, sniffing, placing the product between the teeth and gums, or application of smokeless tobacco such as pan, gutkha, or khaini.
[1] World Health Organization, ‘Non-Communicable Diseases’, https://www.who.int/health-topics/noncommunicable-diseases#tab=tab_1
[2] Social Determinants of Health, World Health Organization, https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
[3] Population Projection 2011-2036, Report Of The Technical Group on Population Projections, MoHFW, https://main.mohfw.gov.in/sites/default/files/Population%20Projection%20Report%202011-2036%20-%20upload_compressed_0.pdf
[4] Elderly in India, National Statistical Office, Ministry of Statistics & Programme Implementation, Government of India, New Delhi, 2021, https://mospi.gov.in/sites/default/files/publication_reports/Elderly%20in%20India%202021.pdf
[5] Dung Duc Le et al.,“How Does Self-Rated Health Differ among Older Vietnamese Men and Women?”, Population Ageing 12 (2019): 69-93, https://link.springer.com/article/10.1007/s12062-018-9223-9#:~:text=Whereas%20Vietnamese%20men%20with%20three,fewer%20than%20three%20chronic%20conditions
[6] Angelique Chan et al., “Gender Differences in Health among Older Singaporeans”, International Sociology 22, no. 4 (2007), https://journals.sagepub.com/doi/10.1177/0268580907078009
[7] Maria-Victoria Zunzunegui et al., “Explaining health differences between men and women in later life: A cross-city comparison in Latin America and the Caribbean”, Social Science & Medicine 68, no. 2, (2009): 235-242, https://www.sciencedirect.com/science/article/abs/pii/S0277953608005637
[8] Duan-Rung Chen, Ly-Yun Chang, and Meng-Li Yang, "Gender-specific responses to social determinants associated with self-perceived health in Taiwan: A multilevel approach", Social Science & Medicine 67, no. 10 (2008): 1630-1640, https://www.sciencedirect.com/science/article/abs/pii/S0277953608003833?via%3Dihub
[9] Alejandra Letelier, Ignacio Madero-Cabib, Eduardo A. Undurraga, and Pedro Pérez-Cruz, "Lifetime socioeconomic determinants of health trajectories among older adults", Advances in Life Course Research 49 (2021): 100415, https://www.sciencedirect.com/science/article/abs/pii/S1040260821000149
[10] Gulam Muhammad Khan, R. K. Thappa, D. S. Adhikari, M. Rajbhandari, P. Dwa, S. Shrestha, and S. Oli, "Cancer prevalence trend in Central Region of Nepal", Journal of Chitwan Medical College 3, no. 1 (2013): 22-25, https://www.nepjol.info/index.php/JCMC/article/view/8461
[11] Shiva Raj Mishra et al., “Burgeoning burden of non-communicable diseases in Nepal: a scoping review”, Globalization and Health 11, no. 32 (2015), https://doi.org/10.1186/s12992-015-0119-7
[12] Kazuo Ono, Yuba Raj Limbu, Shiba Kumar Rai, Manabu Kurokawa, J. Yanagida, Ganesh Rai, Numaya Gurung, Madhusudan Sharma, and Chandra Kala Rai, "The prevalence of type 2 diabetes mellitus and impaired fasting glucose in semi-urban population of Nepal", Nepal Medical College Journal: NMCJ 9, no. 3 (2007): 154-156, https://pubmed.ncbi.nlm.nih.gov/18092429/
[13] K. D. Mehta, P. Karki, M. Lamsal, I. S. Paudel, S. Majhi, B. K. L. Das, S. Sharma, N. Jha, and N. Baral, "Hyperglycemia, glucose intolerance, hypertension and socioeconomic position in eastern Nepal", The Southeast Asian Journal of Tropical Medicine and Public Health 42, no. 1 (2011): 197-207, https://pubmed.ncbi.nlm.nih.gov/21323183/
[14] Stephen Ojiambo Wandera, Betty Kwagala and James Ntozi, "Prevalence and risk factors for self-reported non-communicable diseases among older Ugandans: a cross-sectional study", Global Health Action 8, no. 1 (2015), https://www.tandfonline.com/doi/full/10.3402/gha.v8.27923
[15] Huandong Lin, Qian Li, Yu Hu, Chouwen Zhu, Hui Ma, Jian Gao, Jiong Wu, et al., "The prevalence of multiple non-communicable diseases among middle-aged and elderly people: The Shanghai Changfeng Study", European Journal of Epidemiology 32 (2017): 159-163, https://link.springer.com/article/10.1007/s10654-016-0219-6
[16] Nahid Khademi, Mehran Babanejad, Atefeh Asadmobini, and Hossein Karim, "The Association of Age and Gender with risk factors of noncommunicable diseases among employees in West of Iran", International Journal of Preventive Medicine 8 (2017), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5343616/
[17] Mohamed A. Syed, Ahmed S. Alnuaimi, Abdul Jaleel Zainel, and Hamda AA, "Prevalence of non-communicable diseases by age, gender and nationality in publicly funded primary care settings in Qatar," BMJ Nutrition, Prevention & Health 2, no. 1 (2019): 20-29, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7678476/
[18] Margaret Denton, Steven Prus and Vivienne Walters, "Gender differences in health: a Canadian study of the psychosocial, structural and behavioural determinants of health", Social Science & Medicine 58, no. 12 (2004): 2585-2600, https://pubmed.ncbi.nlm.nih.gov/15081207/
[19] Nicholas Kofi Adjei, Tilman Brand, and Hajo Zeeb, "Gender inequality in self-reported health among the elderly in contemporary welfare countries: A cross-country analysis of time use activities, socioeconomic positions and family characteristics." PloS one 12, no. 9 (2017): e0184676, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0184676
[20] Saulo Vasconcelos Rocha et al., "Cluster analysis of risk factors for chronic non-communicable diseases in elderly Brazilians: Population-based cross-sectional studies in a rural town", Research, Society and Development 10, no. 17 (2021), https://rsdjournal.org/index.php/rsd/article/view/24202
[21] Maurício Feijó da Cruz, Virgílio Viana Ramires, Andrea Wendt, Grégore Iven Mielke, Jeovany Martinez-Mesa, and Fernando César Wehrmeister, "Simultaneity of risk factors for chronic non-communicable diseases in the elderly in Pelotas, Rio Grande do Sul State, Brazil", Cadernos de saude publica 33, no. 2 (2017), https://pubmed.ncbi.nlm.nih.gov/28403276/
[22] Sabit Zenu, Endegena Abebe, Yohannes Dessie, Rukiya Debalke, Tsegaye Berkessa and Mohammed Reshad, "Co-occurrence of Behavioral Risk Factors of Non-communicable Diseases and Social Determinants among Adults in Urban Centers of Southwestern Ethiopia in 2020: A Community-Based Cross-Sectional Study", Journal of Multidisciplinary Healthcare 14 (2021): 1561-1570, https://pubmed.ncbi.nlm.nih.gov/34194229/
[23] Peter Lloyd-Sherlock and Sutapa Agrawal, "Pensions and the health of older people in South Africa: Is there an effect?", The Journal of Development Studies 50, no. 11 (2014): 1570-1586, https://www.tandfonline.com/doi/full/10.1080/00220388.2014.936399
[24] Nguyen Hoang Giang, Tran Thi Mai Oanh, Khuong Anh Tuan, Phan Hong Van and Rohan Jayasuriya, "Is health insurance associated with health service utilization and economic burden of non-communicable diseases on households in Vietnam?", Health Systems & Reform 6, no. 1 (2020), https://www.tandfonline.com/doi/full/10.1080/23288604.2019.1619065
[25] Santosh Kumar Sharma, Deepanjali Vishwakarma, and Parul Puri. "Gender disparities in the burden of non-communicable diseases in India: evidence from the cross-sectional study." Clinical Epidemiology and Global Health 8, no. 2 (2020): 544-549, https://www.sciencedirect.com/science/article/pii/S2213398419304191
[26] Sumanth S Hiremath, “The Health Status of Rural Elderly Women in India: A Case Study”, International Journal of Criminology and Sociological Theory 5, no. 3 (2012), https://ijcst.journals.yorku.ca/index.php/ijcst/article/view/36067
[27] Santosh Kumar Sharma, Devaki Nambiar and Arpita Ghosh, “Sex differences in non-communicable disease multimorbidity among adults aged 45 years or older in India”, BMJ Open 13, no. 3 (2023), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10069553/
[28] Anamika Pandey and Laishram Ladusingh, "Socioeconomic correlates of gender differential in poor health status among older adults in India", Journal of Applied Gerontology 34, no. 7 (2015): 879-905, https://pubmed.ncbi.nlm.nih.gov/24652876/
[29] Ethel M.Brinda, Jørn Attermann, Ulf-Göran Gerdtham and Ulrika Enemark, "Socio-economic inequalities in health and health service use among older adults in India: results from the WHO Study on Global AGEing and adult health survey." Public Health 141 (2016): 32-41, https://pubmed.ncbi.nlm.nih.gov/27932013/
[30] T. Muhammad and Priya Maurya, "Gender differences in the association between perceived income sufficiency and self-rated health among older adults: A population-based study in India", Journal of Women & Aging (2021): 1-14, https://www.semanticscholar.org/paper/Gender-differences-in-the-association-between-and-A-Muhammad-Maurya/80dd984b0ce0370149448a883844ffaca47b2526
[31] Biplab Dhak, "Gender difference in health and its determinants in the old-aged population in India", Journal of Biosocial Science 41, no. 5 (2009): 625-643, https://www.cambridge.org/core/journals/journal-of-biosocial-science/article/abs/gender-difference-in-health-and-its-determinants-in-the-oldaged-population-in-india/E86F202B62AEAB1896B2D2EAD674D868
[32] Executive Summary, Longitudinal Ageing Study in India (LASI) Wave 1, 2017-18, International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC). https://www.iipsindia.ac.in/sites/default/files/LASI_India_Executive_Summary.pdf
[33] Sunita Patel, Arvind Sharma, and Rajesh Tiwari, "Prevalence of Non-communicable Diseases among Elderly Women", National Journal of Community Medicine 13, no. 01 (2022): 7-12. https://www.njcmindia.com/index.php/file/article/view/45
[34] Saswata Ghosh, "Exploring socioeconomic vulnerability of anaemia among women in eastern Indian States", Journal of Biosocial Science 41, no. 6 (2009): 763-787, https://pubmed.ncbi.nlm.nih.gov/19607748/
[35] Prospective Studies Collaboration, “Body-mass index and cause-specific mortality in 900,000 adults: Collaborative analyses of 57 prospective studies”, The Lancet 373, no. 9669 (2009): 1083–1096, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(09)60318-4/fulltext
[36] T. Muhammad, Bandita Boro, Manish Kumar & Shobhit Srivastava,“Gender differences in the association of obesity-related measures with multi-morbidity among older adults in India: evidence from LASI, Wave-1”, BMJ Geriatrics 22, no. 171 (2022), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8886975/
[37] Katarzyna Zatońska, Piotr Psikus, Alicja Basiak-Rasała, Zuzanna Stępnicka, Dagmara Gaweł-Dąbrowska, Maria Wołyniec, Julia Gibka, Andrzej Szuba, and Katarzyna Połtyn-Zaradna, "Obesity and chosen non-communicable diseases in PURE Poland cohort study", International Journal of Environmental Research and Public Health 18, no. 5 (2021): 2701, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7967430/
[38] Joel Negin, Robert Cumming, Sarah Stewart de Ramirez, Seye Abimbola, Sonia E Sachs, “Risk factors for non-communicable diseases among older adults in rural Africa”, Tropical Medicine & International Health 16, no. 5 (2011): 640–646, https://pubmed.ncbi.nlm.nih.gov/21320244/
[39] Nancy Phaswana-Mafuya, Karl Peltzer, Witness Chirinda, Alfred Musekiwa, and Zamakayise Kose, "Sociodemographic predictors of multiple non-communicable disease risk factors among older adults in South Africa", Global Health Action 6, no. 1 (2013): 20680, https://www.tandfonline.com/doi/full/10.3402/gha.v6i0.20680
[40] Aroor Bhagyalaxmi, Trivedi Atul, and Jain Shikha, "Prevalence of risk factors of non-communicable diseases in a District of Gujarat, India", Journal of Health, Population, and Nutrition 31, no. 1 (2013): 78-85, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3702362/
[41] World Health Organization, Non-communicable diseases in the South-East Asia Region, 2011: Situation and response, India, 2012, https://apps.who.int/iris/bitstream/handle/10665/205578/B4793.pdf?sequence=1&isAllowed=y
[42] G. K. Mini and K. R. Thankappan, "Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected Indian states: a cross-sectional study", BMJ open 7, no. 3 (2017), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5353268/
[43] Jhumki Kundu, Mrinmoy Pratim Bharadwaz, Sampurna Kundu and Dhananjay W. Bansod, "The interregional disparity in the choice of health care utilization among elderly in India", Clinical Epidemiology and Global Health 13 (2022), https://cegh.net/article/S2213-3984(21)00237-2/fulltext
[44] Roopani, Neha Dumka, Tarannum Ahmad, Erin Hannah, and Atul Kotwal, “Health facility utilization and Healthcare-seeking behaviour of the elderly population in India”, Journal of Family Medicine and Primary Care 12, no. 5 (2023), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10336929/
[45] Anamika Pandey and Laishram Ladusingh, "Socioeconomic correlates of gender differential in poor health status among older adults in India", Journal of Applied Gerontology 34, no. 7 (2015): 879-905, https://pubmed.ncbi.nlm.nih.gov/24652876/
[46] Biplab Dhak, "Gender difference in health and its determinants in the old-aged population in India", Journal of Biosocial Science 41, no. 5 (2009): 625-643, https://www.cambridge.org/core/journals/journal-of-biosocial-science/article/abs/gender-difference-in-health-and-its-determinants-in-the-oldaged-population-in-india/E86F202B62AEAB1896B2D2EAD674D868
[47] Subhojit Dey, Devaki Nambiar, J. K. Lakshmi, Kabir Sheikh and K. Srinath Reddy, "Health of the elderly in India: challenges of access and affordability", In Aging in Asia: Findings from new and emerging data initiatives (Washington DC: National Academies Press, 2012), https://www.ncbi.nlm.nih.gov/books/NBK109208/
[48] Healthy Aging and Non-Communicable Diseases, Pan-American Health Organization/WHO,
https://www3.paho.org/hq/index.php?option=com_content&view=article&id=9979:healthy-aging-non-communicable-diseases&Itemid=40721&lang=en
[49] Marsh & McLennan Companies, Societal Aging’s Threat to Healthcare Insurance, by Jonathan Tan and Jhamat Mahbubani, 2017, https://www.marshmclennan.com/content/dam/mmc-web/insights/publications/2018/dec/healthy-societies/Societal-Agings-cost-to-insurance/aprc-societal-agings-threat-to-healthcare-insurance.pdf
[50] Healthy Aging and Non-Communicable Diseases, PAHO/WHO, https://www3.paho.org/hq/index.php?option=com_content&view=article&id=9979:healthy-aging-non-communicable-diseases&Itemid=40721&lang=en
[51] Salmaan Ansari et al., “Multimorbidity and depression among older adults in India: Mediating role of functional and behavioural health”, PLOS One (2022), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269646
[52] Bollyky, Thomas J., Tara Templin, Matthew Cohen, and Joseph L. Dieleman. "Lower-income countries that face the most rapid shift in noncommunicable disease burden are also the least prepared." Health affairs 36, no. 11 (2017): 1866-1875, https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0708
[53] Noncommunicable diseases, World Health Organization, https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
[54] Executive Summary, Longitudinal Ageing Study in India (LASI) Wave 1, 2017-18, International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC), https://www.iipsindia.ac.in/sites/default/files/LASI_India_Executive_Summary.pdf
[55] G. K. Mini, "Pattern and correlates of chronic non-communicable diseases among older adults in selected states of India", BKPAI Working Paper Series II No. 3. UNFPA (2014). http://isec.ac.in/BKPAI-WP-III.pdf
[56] The Longitudinal Ageing Study in India Wave-I, 2017-18, International Institute for Population Sciences (IIPS) and NPHCE, MoHFW, https://lasi-india.org/public/documentation/LASI-FACTSHEETS-STATES%20&%20UTs_3-1-2021.pdf
[57] Mills, Katherine T., Andrei Stefanescu, and Jiang He. "The global epidemiology of hypertension." Nature Reviews Nephrology 16, no. 4 (2020): 223-237.
[58] Lalit Dandona, Rakhi Dandona, G. Anil Kumar, D. K. Shukla, Vinod K. Paul, Kalpana Balakrishnan, Dorairaj Prabhakaran, et al., "Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study", The Lancet 390, no. 10111 (2017): 2437-2460, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)32804-0/fulltext
[59] Office of the Registrar General, Government of India, Report on medical certification of cause of death 2020", New Delhi, 2022, https://censusindia.gov.in/nada/index.php/catalog/42681/download/46350/Annual_Report_on_MCCD_2020.pdf
[60] Stauder, Reinhard, and Swee Lay Thein. "Anemia in the elderly: clinical implications and new therapeutic concepts." Haematologica 99, no. 7 (2014): 1127.
[61] Tulika Singh, S. Nagesh, and T. K. Ray, "Magnitude and correlates of anemia in elderly women of a resettlement colony of Delhi", Journal of Mid-life Health 9, no. 1 (2018): 21-25, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5879843/
[62] Abhishek Pathania, Partha Haldar, Shashi Kant, Sanjeev Kumar Gupta, Chandrakant S. Pandav and Damodar Bachani, "Prevalence of anemia among elderly persons residing in old age homes in national capital territory, Delhi, India", Indian Journal of Public Health 63, no. 4 (2019): 288-292, https://pubmed.ncbi.nlm.nih.gov/32189646/
[63] Aakriti Gupta, Lakshmy Ramakrishnan, Ravindra Mohan Pandey, Hem Chandra Sati, Ritika Khandelwal, Preetika Khenduja and Umesh Kapil, "Risk factors of anemia amongst elderly population living at high-altitude region of India", Journal of Family Medicine and Primary Care 9, no. 2 (2020): 673-682, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7113975/
[64] Sheila C Vir and Shoba Suri, “The 5th National Family Health Survey of India: A Sub-National Analysis of Child Nutrition”, ORF Occasional Paper No. 315, May 2021, https://www.orfonline.org/wp-content/uploads/2021/05/ORF_OccasionalPaper_315_NFHS5-ChildNutrition.pdf
[65] Bana Manishaa Reddy et. al, “Hypertension and its Correlates in the Oldest Old Population Aged 80 Years and Above in Urban South India”, Journal of Gerontology and Geriatric Research 7, no. 3 (2018): 472, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6035005/
[66] Executive Summary, Longitudinal Ageing Study in India (LASI) Wave 1, 2017-18, International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC), https://www.iipsindia.ac.in/sites/default/files/LASI_India_Executive_Summary.pdf
[67] Nand Lal Mishra, Gursimran Singh Rana and Adarsh, “Every other elderly in urban India has hypertension: Health ministry report”, Down to Earth, January 13, 2021, https://www.downtoearth.org.in/news/health/every-other-elderly-in-urban-india-has-hypertension-health-ministry-report-75035
[68] Iciar Martín-Timón et al., “Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength?”, World Journal of Diabetes 5, no. 4 (2014), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127581/
[69] A Norhammar et al., “Type 2 diabetes and cardiovascular disease in women”, Diabetologia 56 (2013), https://link.springer.com/article/10.1007/s00125-012-2694-y
[70] Jhumki Kundu and Deepak Pihal, ‘Elderly women more overweight, obese than men’, Down To Earth, July 2021, https://www.downtoearth.org.in/blog/health/-elderly-women-more-overweight-obese-than-men--77804
[71] Prashant Mathur et al., “Prevalence, Awareness, Treatment and Control of Diabetes in India From the Countrywide National NCD Monitoring Survey”, Frontiers in Public Health 10 (2022), https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.748157/full
[72] https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269646
[73] Pal, Chandra Prakash, Pulkesh Singh, Sanjay Chaturvedi, Kaushal Kumar Pruthi, and Ashok Vij, "Epidemiology of knee osteoarthritis in India and related factors." Indian journal of orthopaedics 50 (2016): 518-522.
[74] Chandra Prakash Pal et al., “Epidemiology of knee osteoarthritis in India and related factors”, Indian Journal of Orthopaedics 50, no. 5, (2016), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5017174/
[75] T. Muhammad, Priya Maurya and Palak Sharma, “Prevalence and correlates of bone and joint diseases and its association with falls among older adults in India: Evidence from LASI, 2017–18”, Geriatric Nursing 42, no. 5 (2021): 1143-1150, https://www.sciencedirect.com/science/article/abs/pii/S0197457221002676?via%3Dihub
[76] Saddaf N Akhtar and Nandita Saikia, “Differentials and predictors of hospitalization among the elderly people in India: Evidence from 75th round of National Sample Survey (2017-18)”, medRxiv (2021), https://www.medrxiv.org/content/10.1101/2021.08.25.21262606v1.full
[77] S A Tabish, “Lifestyle Diseases: Consequences, Characteristics, Causes and Control”, Journal of Cardiology & Current Research 9, no. 3 (2017), https://medcraveonline.com/JCCR/lifestyle-diseases-consequences-characteristics-causes-and-control.html
[78] Yodi Christiani et al., “Gender Inequalities in Noncommunicable Disease Risk Factors Among Indonesian Urban Population”, Asia Pacific Journal of Public Health 28, no. 2 (2016): 138-145, https://journals.sagepub.com/doi/10.1177/1010539515626265
[79] Nalinee Jakkaew et al., “Risk of harm from alcohol use and heavy alcohol consumption: Its association with other NCD risk factors in Thailand”, Scientific Reports, (2019): 16343, https://www.nature.com/articles/s41598-019-52754-w
[80] Luke Allen et al., “Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review”, The Lancet Global Health 5, no. 3 (2017), https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(17)30058-X/fulltext
[81] Ghosal, Shishirendu, Abhinav Sinha, Srikanta Kanungo, and Sanghamitra Pati. "Declining trends in smokeless tobacco use among Indian women: findings from global adult tobacco survey I and II." BMC Public Health 21, no. 1 (2021): 1-11. Noncommunicable Diseases in the South-East Asia Region: Situation and Response, World Health Organization, India, 2011, https://apps.who.int/iris/bitstream/handle/10665/205578/B4793.pdf?sequence=1&isAllowed=y
[82] G. K. Mini and K. R. Thankappan, "Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected Indian states: a cross-sectional study", BMJ open 7, no. 3 (2017), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5353268/
[83] Ogechukwu Asogwa et al.,“Multimorbidity of non-communicable diseases in low-income and middle-income countries: A systematic review and meta-analysis”, BMJ Open 12, no. 1 (2021), https://bmjopen.bmj.com/content/12/1/e049133
[84] Steven Prus and Ellen Gee, “Gender Differences in the Influence of Economic, Lifestyle, and Psychosocial factors on Later-life Health”, Canadian Journal of Public Health 94, no. 4 (2003): 306-309, https://pubmed.ncbi.nlm.nih.gov/12873092/
[85] Bo Simonsson & Anu Molarius, “Self-rated health and associated factors among the oldest-old: results from a cross-sectional study in Sweden”, Archives of Public Health 78 (2020), https://archpublichealth.biomedcentral.com/articles/10.1186/s13690-020-0389-2
[86] Shichen Cui et al., “Are there gender differences in the trajectories of self-rated health among chinese older adults? an analysis of the Chinese Longitudinal Healthy Longevity Survey (CLHLS)”, BMC Geriatrics 21 (2021), https://doi.org/10.1186/s12877-021-02484-4
[87] Saddaf Naaz Akhtar et al., “Self-rated health among older adults in India: Gender specific findings from National Sample Survey”, i, no. 4 (2023), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0284321
[88] Nicholas Kofi Adjei, Tilman Brand and Hajo Zeeb, “Gender inequality in self-reported health among the elderly in contemporary welfare countries: A cross-country analysis of time use activities, socioeconomic positions and family characteristics”, PLoS One 12, no. 9 (2017) https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0184676
[89] Timothy C Lee et al., “Socioeconomic Status and Incident Type 2 Diabetes Mellitus: Data from the Women's Health Study”, PLoS One 6, no. 12 (2011), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0027670
[90] Sujata and Ramna Thakur, “Unequal burden of equal risk factors of diabetes between different gender in India: a cross-sectional analysis”, Scientific Reports 11, no. 1 (2021), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8608835/
[91] Takashi Oshio and Mari Kan, “Educational level as a predictor of the incidences of non-communicable diseases among middle-aged Japanese: a hazards-model analysis”, BMC Public Health 19, (2019), https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7182-6
[92] Population Reference Bureau, Noncommunicable Diseases Among Older Adults in Low- and Middle-Income Countries, In Today’s Research in Aging 26, 2012, https://www.prb.org/wp-content/uploads/2020/11/TRA26-2012-NCD-aging.pdf
[93] Sor Tho Ng et al., “What matters for life satisfaction among the oldest-old? Evidence from China”, PLoS One 12, no. 2 (2017), https://pubmed.ncbi.nlm.nih.gov/28187153/
[94] Raghunath Mandi and Dhananjay Bansod, “Association between Social Network, Social Support, and Life Satisfaction Among Elderly in India: Evidence from LASI Survey”, Research Square, 2022, https://assets.researchsquare.com/files/rs-1678844/v1/65ec0b9c-e559-4bec-8e77-5f151e96efb8.pdf?c=1665468862
[95] Rocio Calvo and Dawn C Carr and Christina Matz-Costa, “Another Paradox? The Life Satisfaction of Older Hispanic Immigrants in the United States”, Journal of Aging Health 29, no. 1 (2017), https://pubmed.ncbi.nlm.nih.gov/26772911/
[96] Rhonda Belue, “The role of family in non-communicable disease prevention in Sub-Saharan Africa”, Global Health Promotion 24, no. 3 (2016), https://www.researchgate.net/publication/300083423
[97] Lisa F. Berkman et al., “Social Networks, Family, and Care Giving Among Older Adults in India”, Aging in Asia: Findings From New and Emerging Data Initiatives, 261-278 https://www.ncbi.nlm.nih.gov/books/NBK92618/pdf/Bookshelf_NBK92618.pdf
[98] Kakoli Roy and Anoshua Chaudhuri, “Influence of socioeconomic status, wealth and financial empowerment on gender differences in health and healthcare utilization in later life: Evidence from India”, Social Science & Medicine 66, no. 9 (2008): 1951-1962, https://pubmed.ncbi.nlm.nih.gov/18313185/
[99] Sunita Patel, Arvind Sharma, and Rajesh Tiwari, "Prevalence of Non-communicable Diseases among Elderly Women", National Journal of Community Medicine 13, no. 01 (2022): 7-12. https://www.njcmindia.com/index.php/file/article/view/45
[100] Women in labour markets: Measuring progress and identifying challenges, International Labour Office. – Geneva (2010),
https://www.ilo.org/wcmsp5/groups/public/---ed_emp/---emp_elm/---trends/documents/publication/wcms_123835.pdf
[101] Irudaya Rajan, Carla Risseeuw, Myrtle Perera, Institutional Provisions and Care for the Aged, Anthem Press (2008), https://books.google.co.in/books/about/Institutional_Provisions_and_Care_for_th.html?id=RXjgac5QBx4C&redir_esc=y
[102] Executive Summary, Longitudinal Ageing Study in India (LASI) Wave 1, 2017-18, International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC), https://www.iipsindia.ac.in/sites/default/files/LASI_India_Executive_Summary.pdf
[103] Abhinav Sinha et al., “Multimorbidity Among Urban Poor in India: Findings From LASI, Wave-1”, Frontiers in Public Health 10, (2022), https://www.frontiersin.org/articles/10.3389/fpubh.2022.881967/full
[104] Didac Santesmasses et al., “COVID‐19 is an emergent disease of aging”, Aging Cell 19, no. 10 (2020), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7576244/
[105] William Joe, Abhishek Kumar, Sunil Rajpal, U.S. Mishra, and S V Subramanian “Equal risk, unequal burden? Gender differentials in COVID-19 mortality in India”, J Glob Health Sci, (2020), https://www.e-jghs.org/DOIx.php?id=10.35500/jghs.2020.2.e17#:~:text=Conclusion,require%20special%20care%20when%20infected
[106] N. David Yanez, Noel S. Weiss, Jacques-André Romand & Miriam M. Treggiari, “COVID-19 mortality risk for older men and women”, BMC Public Health 20 (2020), https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09826-8
[107] Corona Older, https://corona-older.com/
[108] Elderly in India Report, Ministry of Statistics and Programme Implementation, Government of India, 2021, http://mospi.nic.in/sites/default/files/publication_reports/Elderly%20in%20India%202021.pdf
[109] Divya Chandrababu, “TN survey shows vaccines hesitancy highest among elderly”, Hindustan Times, August 9, 2021, https://www.hindustantimes.com/cities/others/tn-survey-shows-vaccines-hesitancy-highest-among-elderly-101628452573333.html
[110] Sitara Srinivas, “The curious case of vaccine hesitancy in Tamil Nadu”, Observer Research Foundation, June 15, 2021, https://www.orfonline.org/expert-speak/the-curious-case-of-vaccine-hesitancy-in-tamil-nadu/
[111] Alice Yhoshu, “Nagaland trails in Covid vaccination; hesitancy in 45+ age group is one cause”, Hindustan Times, May 31, 2021, https://www.hindustantimes.com/india-news/nagaland-trails-in-covid-vaccination-hesitancy-in-45-age-group-is-one-cause-101622432151341.html
[112] Madur Verma et al., “Co-existing Non-communicable Diseases and Mental Illnesses Amongst the Elderly in Punjab, India”, European Endocrinology 15, no. 2 (2019): 106-112, https://pubmed.ncbi.nlm.nih.gov/31616502/
[113] M Shao et al., “Depression and cardiovascular disease: Shared molecular mechanisms and clinical implications”, Psychiatry Research 285, (2020): 112802, https://pubmed.ncbi.nlm.nih.gov/32036152/
[114] Devakshi Dua and Sandeep Grover, “Mental disorders and noncommunicable diseases: A likeness, an overlap or an affiliation?”, Journal of Geriatric Mental Health 7, no. 2 (2020): 67-69, https://www.jgmh.org/text.asp?2020/7/2/67/307593
[115] Vikram Patel and Somnath Chatterji, “Integrating mental health in care for Noncommunicable Diseases: An imperative for person-centered care”, Health Affairs 34, no. 9 (2015): 1498-1505, https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2015.0791
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

 PDF Download
PDF Download



 PREV
PREV



