Climate change affects both physical and mental health, and in many different ways. Heat and extreme weather events not only lead to increased human mortality and morbidity but also longer-term food and water shortages, air pollution, and disease. Increased exposures to wildfire smoke, atmospheric dust, and airborne allergens are associated with cardiovascular and respiratory distress. Untimely rain and flooding increase the occurrence of food- and water-borne diseases and disrupt health services. All these, thus, have economic and societal impacts.
Rising vector-borne diseases
Reducing GHG emissions and better vector control would lower the epidemic potential of dengue and other mosquito-borne diseases in Europe and other temperate regions.
The spread of mosquito-borne diseases is sensitive to temperature due to its broad
effects on the life cycle, biting rates, and acquisition and transmission of pathogens by mosquitos. The most prominent vectors of disease transmission in humans are the
Anopheles and
Aedes mosquitos—the former for malaria and the latter for several diseases such as chikungunya, dengue, filariasis, rift valley fever, yellow fever, and zika. By 2050 about 50 percent of the world’s population is estimated to live in places inhabited by the
Aedes mosquito, and by 2080 about one billion people could face their first exposure to mosquito-borne diseases.
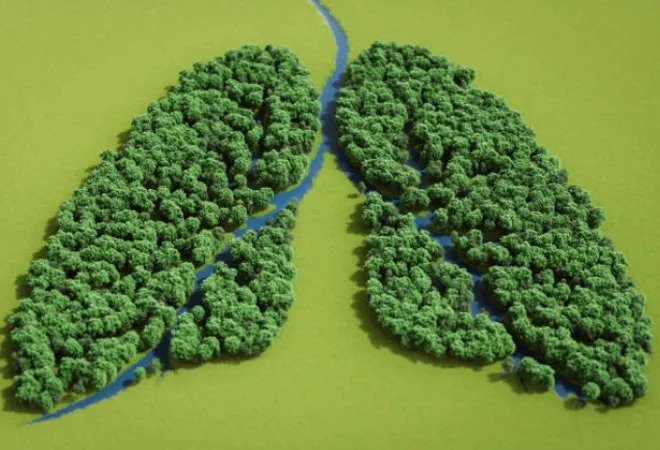
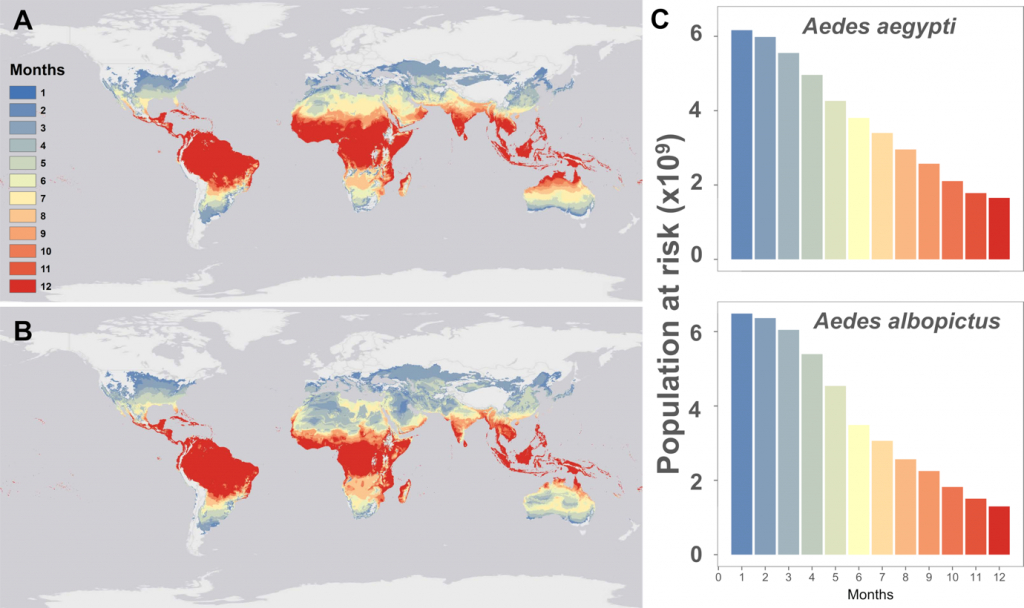
Models suggest transmissions to be year-round or extended in tropical and subtropical regions, and extend beyond the summer months in temperate regions of the world (Figure 1). With increasing emissions, the
Anopheles mosquito would also experience increased range, population, and distribution density.
By 2070 the epidemic belt for dengue and malaria is expected to expand towards temperate regions, placing an additional 4·7 billion people at risk.
Models for dengue transmission in Europe show a broad correlation with greenhouse gas (GHG) emissions. Thus, reducing GHG emissions and better vector control would lower the epidemic potential of dengue and other mosquito-borne diseases in Europe and other temperate regions.
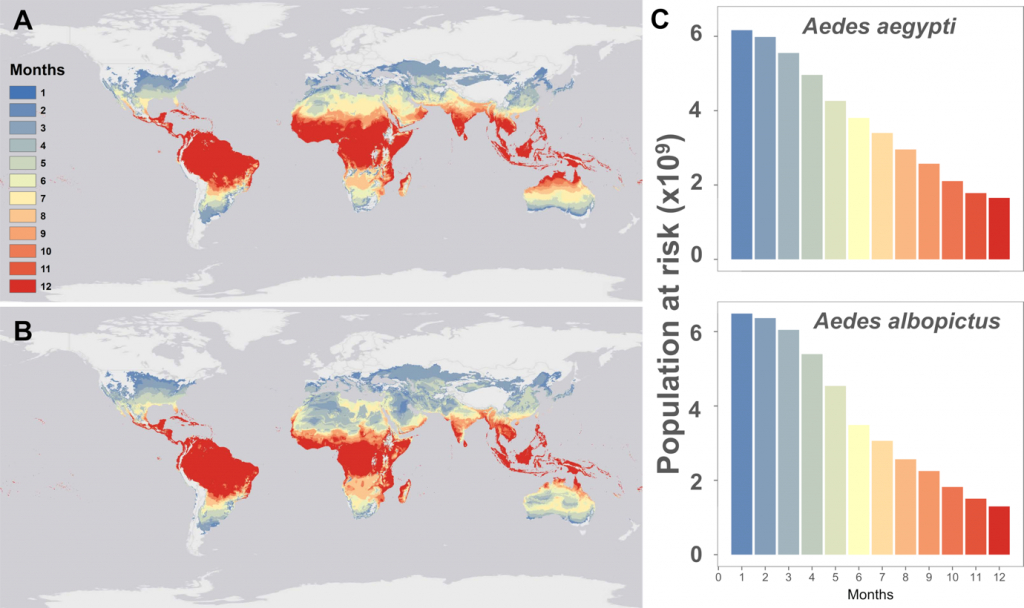 Figure 1. Maps of monthly suitability for transmission based on mean temperatures for(A) Aedes aegypti and (B) Aedes albopictus, and (C) the number of people at risk as a function of their months of exposure for Aedes aegypti or Aedes albopictus.
Figure 1. Maps of monthly suitability for transmission based on mean temperatures for(A) Aedes aegypti and (B) Aedes albopictus, and (C) the number of people at risk as a function of their months of exposure for Aedes aegypti or Aedes albopictus.
Spillover of viral zoonoses
Between 1940 and 2004, the global distribution of
emerging infectious disease (EID) events was non-random and predominantly zoonotic, i.e., transfer from wild animals and transfer to humans. Spillovers can happen directly through animal bites, consumption of raw or undercooked meat or through contaminated water, and indirectly through vectors such as mosquitoes, ticks, etc. Domestic animals and species that co-habit with humans and wild animals whose habitats have been exploited or destroyed have the greatest
spillover potential. Anthropogenic activities and environmental change remain its biggest drivers.
The
geographical distribution of species is affected by climate change, as are the location and frequency of animal-human encounters. Species and virus richness for various mammal groups, and their abundance are key determinants of
spillover risk. Rodents and bats comprise 45 percent and 20 percent of mammals, and host an estimated 60 percent and 30 percent of zoonotic viruses, respectively. They are the key transmitters and humans being the most abundant species are their biggest target. At least
10,000 different viruses can potentially infect humans, with the vast majority circulating silently in wild animals. When the animals move, they bring along these viruses, offering new opportunities to spread and evolve. Over the next 50 years, climate change may lead to more than
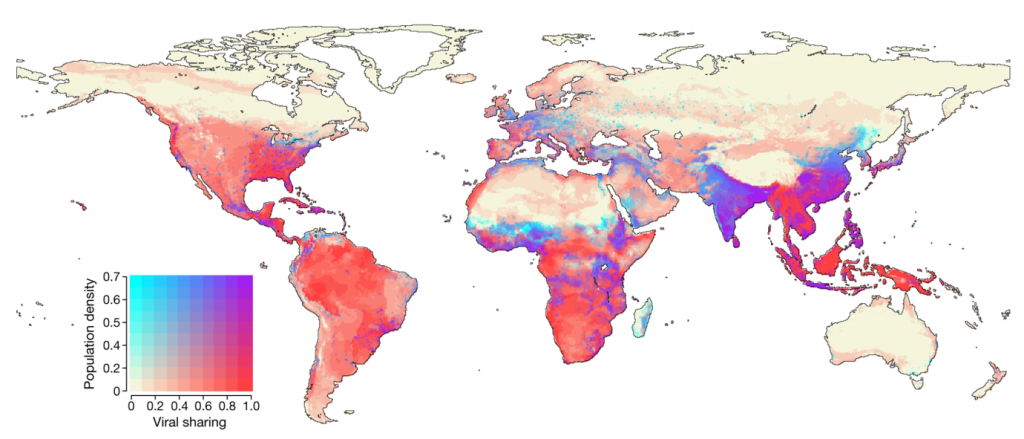
15,000 new cases of virus exchanges between mammalian species, including humans, especially in densely populated areas. India, Indonesia, and the African Sahel are the predicted hotspots for new disease emergence (Figure 2).
 Figure 2. Models show that by 2070 and with a 2oC rise in average temperatures relative to pre-industrial times, regions with the highest chances of virus sharing between mammals will overlap with dense human population centres. Source: Carlson et al, https://doi.org/10.1038/s41586-022-04788-w.
Figure 2. Models show that by 2070 and with a 2oC rise in average temperatures relative to pre-industrial times, regions with the highest chances of virus sharing between mammals will overlap with dense human population centres. Source: Carlson et al, https://doi.org/10.1038/s41586-022-04788-w.
Global warming could also unleash ancient microbes that lie dormant under the permafrost and in glaciers as evident from a 2016
anthrax outbreak in Siberia. Novel viruses were also found in
glacial ice cores dating back to 15,000 years, and in 30,000 years old
Siberian permafrost. Unknown pathogens may be lurking in environments that have been made more accessible by global warming.
A
recent study looked at the impacts of 10 climatic hazards sensitive to GHG emissions on known human infectious diseases. It found half of the diseases to be aggravated by climatic hazards through over 1,000 unique pathways. This complexity emphasises that societal adaptations alone will be insufficient to address the problem unless GHG emissions are also reduced urgently.
Climate crisis worsens mental health
These direct climate-driven mental health effects are not equally distributed. Women, children, the poor, especially those in low- and middle-income countries are the most vulnerable and share a disproportionately higher mental health burden.
The climate crisis has also affected the mental health of hundreds of millions of people. Floods, wildfires, and other natural disasters increase the number of people experiencing post-traumatic stress disorder (PTSD), depression, and addiction. These direct climate-driven mental health effects are not equally distributed. Women, children, the poor, especially those in low- and middle-income countries are the most vulnerable and share a disproportionately higher mental health burden. People experience ‘eco-anxiety’ through anticipation of climate-related impacts on themselves by observing it on others. This was revealed in a
global survey in which around 40 percent of young people feared having children due to the climate crisis. Long-term economic and societal impacts of climate change will also affect mental health and well-being globally. Repeated droughts, untimely rain and floods destroy crops, leading to loss of incomes and access to food. Rising sea levels, desertification and deforestation lead to loss of land and space for people to grow and seek food, live and work. Climate-driven loss of livelihoods and safe spaces would increase conflict, displacement, and forced migration, and this too disproportionately affects the poor.
Poor mental health and its impact on overall health and productivity was
estimated to cost the world economy about US$2.5 trillion annually in 2010, with a projected rise to US$6 trillion annually by 2030. Worsening mental health due to climate change will bring huge additional costs, and therefore, actions to mitigate climate change and efforts to improve mental health can be a win-win situation. However, since climate actions and policy are often not sensitive to their mental health impact, understanding the barriers and creating an enabling framework will be crucial.
Between 2030 and 2050, the World Health Organization (WHO) estimates that climate change will cause
250,000 extra deaths annually from diarrhoea, heat stress, malaria, and malnutrition. It also estimates that by 2030 the near-term direct costs to health from climate change will reach US$2-$4 billion annually. At this rate, climate change is predicted to push more than
100 million people into poverty over the next 10 years.
For its negative impacts on health, the world must take immediate and sustainable steps to start reducing emissions, both in the short and long term. Preparedness will include strengthening health systems and the ability to detect, diagnose, and study diseases, and increase surveillance of animal pathogens to better manage zoonotic spillovers at the source. We must also create the pathways necessary for research, development, manufacturing, and market access for drugs (especially new antibiotics) and new vaccines. Most importantly, access to affordable healthcare, which closes the health gap between rich and poor countries is in everyone’s interest. COVID showed us that a new disease emerging in any part of the world can quickly spread to major economic and population centres and cause severe disruption.
Read Part III of the series that delves into the climate change and food security.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.



 Climate change affects both physical and mental health, and in many different ways. Heat and extreme weather events not only lead to increased human mortality and morbidity but also longer-term food and water shortages, air pollution, and disease. Increased exposures to wildfire smoke, atmospheric dust, and airborne allergens are associated with cardiovascular and respiratory distress. Untimely rain and flooding increase the occurrence of food- and water-borne diseases and disrupt health services. All these, thus, have economic and societal impacts.
Climate change affects both physical and mental health, and in many different ways. Heat and extreme weather events not only lead to increased human mortality and morbidity but also longer-term food and water shortages, air pollution, and disease. Increased exposures to wildfire smoke, atmospheric dust, and airborne allergens are associated with cardiovascular and respiratory distress. Untimely rain and flooding increase the occurrence of food- and water-borne diseases and disrupt health services. All these, thus, have economic and societal impacts.
 PREV
PREV


