At the press briefing on 16 March 2020, Mr Lav Agarwal, Joint Secretary of the Ministry for Health and Family Welfare made it clear that avoiding unnecessary panic is behind the decision to keep the testing strategy for COVID-19 narrow-based. Later in the day, ICMR also released latest data on testing. As of 17th March, India has tested 12513 samples from 11623 individuals (Graph 1). By 19th March 10 am, India has tested around f 13316 samples from 12426 individuals, and the number of tests is accelerating at more than 1000 a day. At an estimated capacity for testing more than 10000 samples a day, only a small proportion is being utilized as of now, according to ICMR.
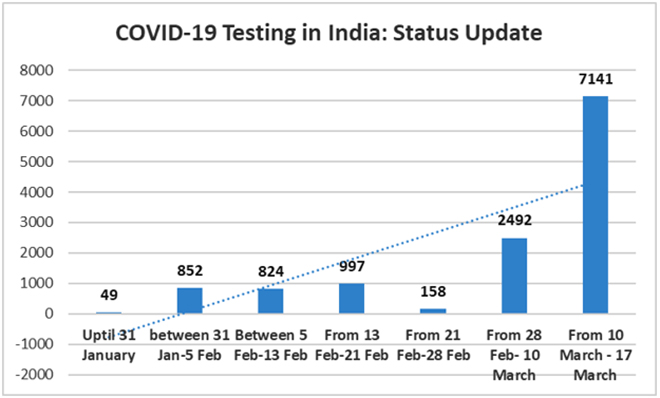 Source: ICMR and various other Government of India sources
Source: ICMR and various other Government of India sources
For a fund-starved health system like India, a viral disease like COVID- 19 which can spread fast undetected and kill already immunocompromised populations – like the aged, and those with chronic non-communicable diseases- presents a nightmare scenario. With many countries, the number of COVID-19 patients has been a function of testing and surveillance capacity of the health system. It is highly likely that the relatively low numbers currently reported in India are a result of this, and the real extent of how fast and how far the virus has spread will emerge only later.
Given that India is still in Phase 2 of the epidemic, with some localised transmission possibly taking place in pockets, there is a need to use testing, isolation and contact tracing as the backbone of our approach. A comprehensive approach led by testing and supported by social distancing and measures like hand washing is needed. Breaking the chains of transmission is extremely important, given India’s very limited healthcare delivery capacity. There is a strong case for broadening the testing strategy, which currently only includes a subset of symptomatic people- those who have undertaken international travel or are contacts of laboratory tested positive patients. Such an expansion is possibly in the cards, with the government inviting private laboratories to join force.
India is perhaps justified in not starting with a broad testing strategy given the lack of preparedness in the system to handle population panic. Had India tested more categories, including old patients or those with preconditions like heart disease, respiratory illness or high blood pressure reporting severe pneumonia and managed to find clusters and cases, it is likely that it may have caused panic, overwhelmed hospitals with people with mild symptoms rushing to get tested and treated. This may have paved way for localised intensive transmission within hospitals themselves, that too for people who are old and immunocompromised. Also, during epidemics like Ebola, there are known instances where many more with measles and malaria die just because of disruptions in the health system.
There are already anecdotes of people with mild symptoms visiting at least three large hospitals, on multiple days, with the aim of getting tested for Covid-19 and yet being turned back by the authorities. Panic may be triggering this urge to get tested, but people with symptoms thronging our already crowded hospitals is a recipe for disaster. There is a dire need to avoid high risk populations getting infected within hospital settings. Broad based testing also will introduce risks with false negatives as well as false positives - with false negatives spreading disease, and false positive acquiring it.
On the other hand, not expanding the testing strategy will mean that the mildly infected may keep spreading the virus to risky patients, until the infected population is too big to handle, resulting in huge human costs. Negotiating this difficult double-bind is possible only through educating, empowering and engaging the public, while ramping up the testing capacity. We do not know yet how many pockets within India may have sustained local transmission of the virus, since the ICMR’s testing of a small random sample may not be able to capture it. However, what we know is that most parts of India may still be in the containment phase where we can considerably suppress and slow down the virus by testing every suspect patient, identifying and isolating contacts of patients, and testing if they show symptoms. Perhaps Prime Minister Shri Narendra Modi’s planned address to the nation will allay people’s fears and set the context for an aggressive testing strategy.
According to the press briefing by ICMR, and reflected in data, India is already moving towards testing more cases. As of now, all asymptomatic suspected patients including travelers and contacts of positive cases will be put in home isolation, and will be tested as soon as they become symptomatic. India already has 72 functional laboratories, and 49 more will be activated by the end of this week along with 51 NABL certified private laboratories are also being engaged. It is also made clear that testing kits will not be a binding constraint.
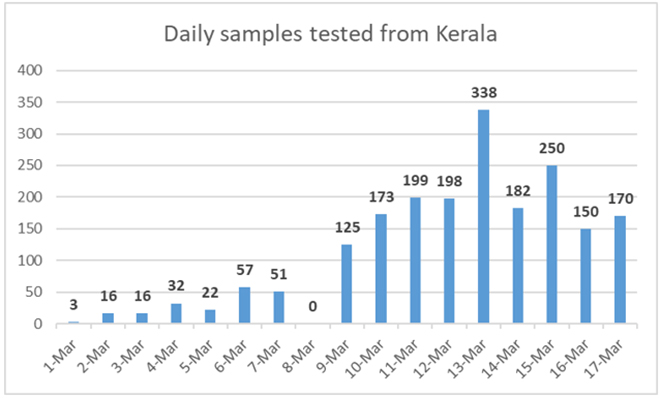 Source: http://dhs.kerala.gov.in/
Source: http://dhs.kerala.gov.in/
Even as officials claim that only 10% of the capacity is being currently utilised, there are some concerns regarding the testing capacity of the public sector on paper and in actual terms. There is no regular dissemination of national level data regarding testing with only rudimentary data being made available. However, Kerala shares data on testing and other parameters every day. Looking at the testing data from Kerala (Graph 2), a spike in the number of daily tests is clearly visible in the second week of March onwards.
The worry is that the backlog (the difference between samples tested and results known) has dramatically increased over the last two weeks. On 1st March, the backlog was just around 15, which increased to more than 50 on 8th March, and on 17th March, it has grown to a worrying 650. This indicates limits and bottlenecks in the public sector’s capacity to test and underlines the need to engage the private sector and ramp up capacity immediately. There is a need to disseminate clear data in order to avoid fake news and resulting panic among people.
These are anxious times. After almost no new cases being reported for weeks, India has been reporting COVID-19 patients regularly in March, and the number has reached 166 with three deaths. With media coverage of Coronavirus picking up and the stock market crashing, situation is ripe for fear and panic to set in. Coronavirus has exposed vulnerability of governments across political systems across the globe. The cases from China seem to be declining with the rest of the world reporting almost all cases and fatalities. However, not many other countries can try to do what China managed to do by using old fashioned classic public health interventions, with no regard for human rights. Testing actively, finding the pockets of infection followed by strong actions to suppress the virus will have to be the mainstay of India’s response.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.



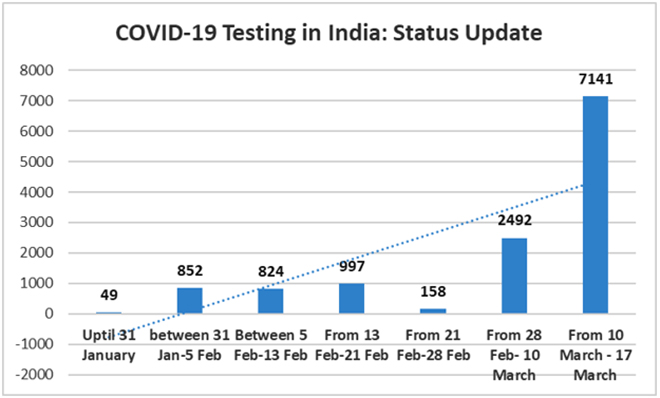 Source: ICMR and various other Government of India sources
Source: ICMR and various other Government of India sources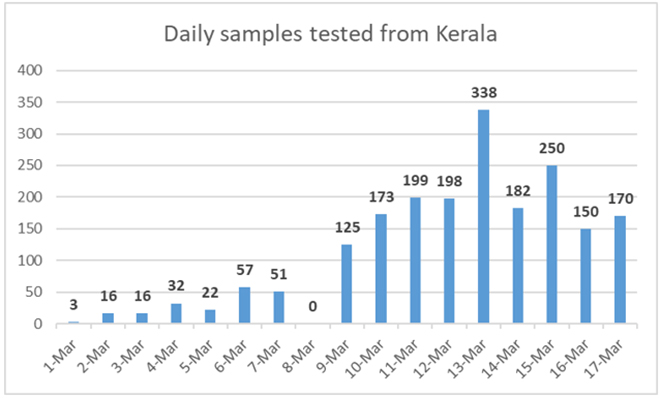 Source:
Source:  PREV
PREV