 Malaria
Malaria is a life-threatening disease caused by parasites, with an
estimated 228 million cases and 405,000 deaths occurring globally. Countries in sub-Saharan Africa and India carry almost 85 percent of the global malaria burden. COVID-19 was declared a global pandemic in March 2020 and has
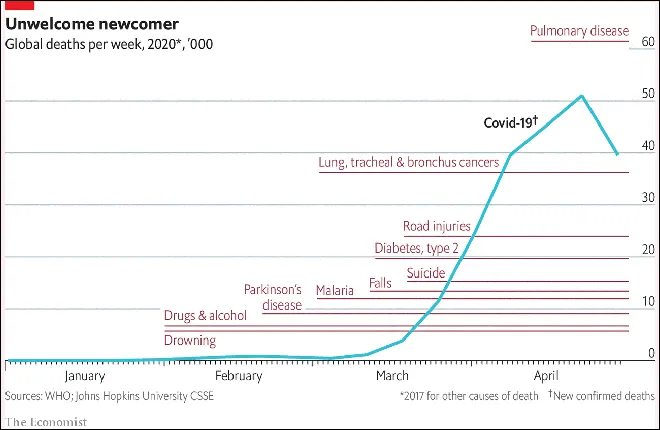
affected more than 140 million people and caused more than three million deaths around the world. Malaria and COVID-19 mask each other’s
symptoms leading to misdiagnosis of both, especially with co-infection tending to lead to worse outcomes. The figure below indicates causes for global death tally for 2020 with COVID-19 deaths far exceeding breast cancer or malaria.
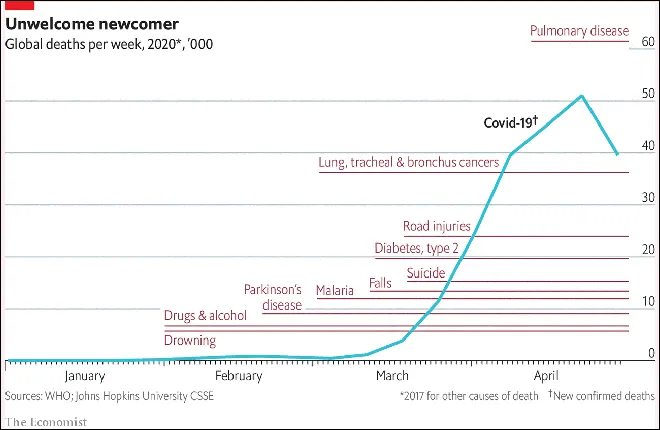 Source: https://www.economist.com/graphic-detail/2020/05/01/covid-19-has-become-one-of-the-biggest-killers-of-2020
Source: https://www.economist.com/graphic-detail/2020/05/01/covid-19-has-become-one-of-the-biggest-killers-of-2020
The implications of COVID-19 and malaria epidemics can be devastating, especially in
low- and middle-income countries with weak health infrastructure and poor human and financial resources. The COVID-19 pandemic has led to
disruption in health delivery systems, with the inappropriate treatment of malaria leading to increased morbidity and mortality. Similar disruption was observed during the
Ebola outbreak, with more deaths from malaria than the Ebola virus.
Low- and middle- income countries continue to be
burdened with lower average life expectancy and morbidity due to infectious diseases, malnutrition, tuberculosis and malaria. Although it is important to note that
COVID-19 has been less aggressive in children as compared to malaria, which is known to affect children under five years of age. However, economic and behavioural changes due to COVID-19 has impacted families, leading to increase in malaria morbidity and mortality in children.
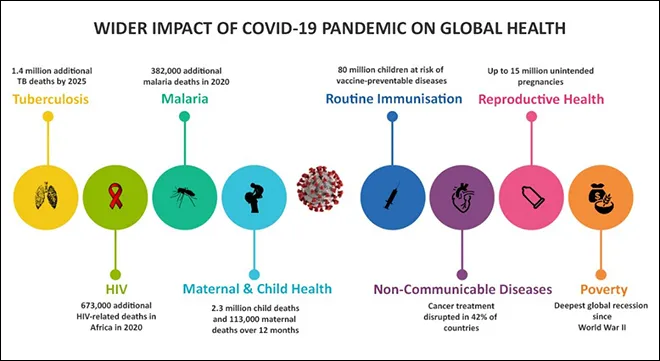 Source: The Printhttps://theprint.in/health/how-covid-is-making-it-tougher-to-tackle-tb-aids-malaria-and-child-health/443658/
Source: The Printhttps://theprint.in/health/how-covid-is-making-it-tougher-to-tackle-tb-aids-malaria-and-child-health/443658/
A
case study from Africa indicates the ‘need for malaria-endemic countries to consider measures for preparation and prevention, focusing on not only the threat of COVID-19 but also the possible impact of other diseases, especially malaria’.
Research indicates the possible role of antimalarials in the treatment/management of COVID-19 reducing the extent of the viral disease.
A
study from Africa to assess the syndemic of COVID-19 pandemic and malaria suggests early intervention for COVID-19 to effectively reduce the scale of the epidemic and mitigate its impact on malaria transmission potential.
Cameroon and
Zimbabwe have reported a surge in malaria cases and deaths during the COVID-19 pandemic. The
Lancet indicates a reversal of two decades of progress against malaria for Africa with significant increase in malaria mortality due to the indirect effects of COVID-19. Malaria deaths are projected to double in Sub Saharan Africa due to the impact of COVID-19 on health services, according to
WHO.
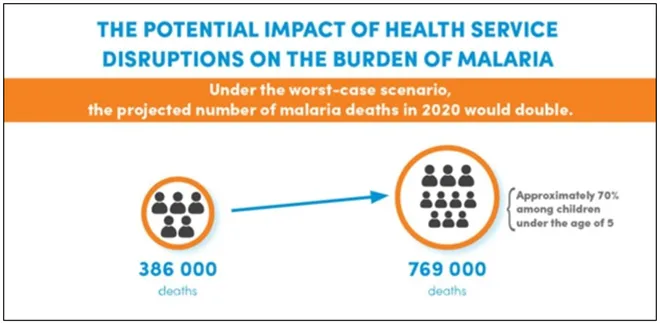 Source: World Economic Forum
WHO
Source: World Economic Forum
WHO calls for National and local programmes to ensure non disrupted preventive care and management for malaria control while facing the COVID-19 response. Preparedness, readiness and response actions are crucial to overcome the challenges posed by COVID-19. A report by the
Lancet Commission concludes ‘malaria eradication by 2050 remains ambitious, achievable, and necessary, and will contribute to a healthier and more secure world.’ This will allow allocation of human and financial resources to other health priorities and pandemic preparedness.
Malaysia sets an example in being certified ‘malaria free’, with strong program leadership in ensuring malaria control and prevention activities are not interrupted even during COVID-19. Recently,
El Salvador was certified malaria free by WHO. However, the impact of COVID-19 on malaria elimination poses a challenge in achieving the
goal of eliminating and eradicating malaria in at least ten countries by 2020 and 35 countries by 2030.
Malaria endemic countries are to follow WHO guidelines and diagnose both malaria and COVID-19 for suspected cases.
India is one of the 11 most
malaria affected countries in the world accounting for 3 percent of world malaria burden. However, India has shown considerable progress in reducing its malaria burden, reporting a decline of 17.6 percent in 2019.
COVID-19 is an impending risk in the progress made so far and signifies a need for preventive measures and awareness campaigns.
WHO calls for reinvigorated action to fight malaria to overcome access gaps, COVID-19 and a fund crunch. The
global projections indicate that targets for malaria reduction will be missed 37 percent and mortality reduction by 22 percent mortality due to the formidable challenge posed by COVID-19 to malaria response. A moderate disruption to effective antimalarial treatment can cause considerable loss of life.
Despite the overwhelming impact of the pandemic world over, one cannot neglect malaria and other vector borne diseases that continue to devastate entire populations. For
India to achieve target of being malaria free by 2030, intensive focus and sustained efforts to control malaria is required.
To overcome the challenge posed by the
syndemic, preparedness of the health care system in malaria endemic countries to tackle effects of COVID-19 is crucial. Efforts to prevent, control and
eliminate malaria contributes to achieving several of the sustainable development goals including Goal 1 (no poverty), Goal 4 (quality education), Goal 5 (gender equality), Goal 8 (promote sustained, inclusive and sustainable economic growth), and Goal 10 (reduce inequality).

The Global Technical Strategy for Malaria 2016-2030 indicates 40 times return on investment if a country becomes malaria free. A cost benefit analysis for malaria elimination from
Thailand projects US $ 2 to US $ 15 return on investment for every 1 US dollar. For
India, there is a 20 times benefit on investment for malaria control besides saving lives. The cost of
inaction will be devastating with loss of life and economic burden.
Thus, to eliminate malaria by 2030, improving interventions and tools, sustained investment along with effective communication strategy for social and behaviour change of community will be vital. Malaria vaccine would be the most effective and preventive measure and there is hope with the success of the
first malaria vaccine trial.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.




 Source:
Source: 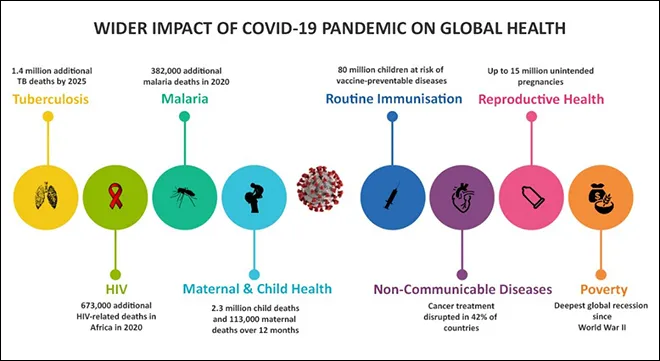 Source:
Source: 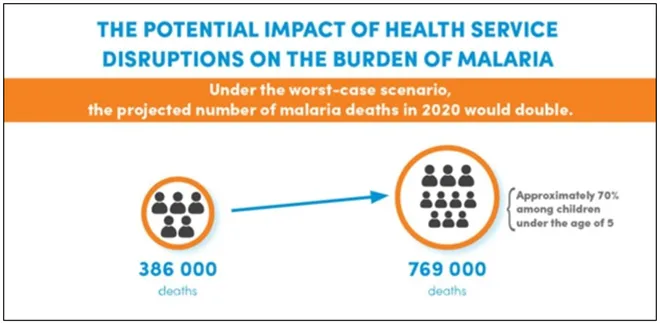 Source:
Source:  The Global Technical Strategy for Malaria 2016-2030 indicates 40 times return on investment if a country becomes malaria free. A cost benefit analysis for malaria elimination from
The Global Technical Strategy for Malaria 2016-2030 indicates 40 times return on investment if a country becomes malaria free. A cost benefit analysis for malaria elimination from  PREV
PREV


