
India has grown leaps and bounds over the last few decades, in terms of healthcare and social development. Access to healthcare for all classes of society has been a key objective to that end. However, a question that still lingers is have we achieved this objective? The answer lies in achieving Universal Health Coverage(UHC) across all boards, and sections of the population. The National Health Policy 2017 advised the commencement of ‘
Ayushman Bharat’ to realise the goal of UHC. In a nation that invests very little funds into healthcare, the out-of-pocket expenses (OOPE) alone account for
64.7 percent of the total cost of healthcare. This is greater than the global average, and families in the low-income category may experience catastrophic health expenditures (CHE)—an important determinant of a nation's poverty and poor health. The PMJAY programme was created to provide the most disadvantaged people in our country with financial security against hospitalisation and was partly a response to the high Out-of-Pocket (OOP) spending. It provides a cover of up to INR 5 lakhs per family per year, to over 10.74 crore vulnerable entitled families, for secondary and tertiary care hospitalisation. Despite questionable utilisation across states, the
world’s largest government-funded health insurance scheme has exceeded expectations in a few states, especially in Tamil Nadu.
The PMJAY programme was created to provide the most disadvantaged people in our country with financial security against hospitalisation and was partly a response to the high Out-of-Pocket (OOP) spending.
Implementation
Motivated by the federalist spirit, PMJAY gives states much latitude in how they administer the programme and is implemented in three formats—trust model, insurance model and the hybrid model. The trust model is followed across 22 states, where a public buyer (the state health agency) directly acquires services from empanelled hospitals and similar providers, thus making it completely state-funded. In eight of the states, the ‘insurance model’ is followed, where the state pays an insurance company a fixed premium for the predefined list of services for each household (HH) enrolled. In the ‘hybrid model’, which is followed by three states, the dependence on insurance companies to process claims is partially transferred to a state-run trust.
PMJAY-CMCHIS in Tamil Nadu
A robust healthcare system is a prerequisite to achieving better health outputs. Being the first state to enact the Public Health Act, Tamil Nadu has always led the way with a strong hold on policy implementation. In 2009, the
“Chief Minister Kalaignar's Insurance Scheme for Life Saving Treatments” (KHIS) was introduced in Tamil Nadu to ensure that low-income and poor sections of society receive free medical care in both public and private hospitals for serious illnesses. Later, in 2011, this programme underwent an expansion in coverage and was reintroduced under the name “
Chief Minister's Comprehensive Health Insurance Scheme (CMCHIS)”. Tamil Nadu implemented PM-JAY in integration with the CMCHIS in 2018, which is collectively known as “
Pradhan Mantri Jan Arogya Yojana-Chief Minister's Comprehensive Health Insurance Scheme” (PMJAY-CMCHIS).
Statistically, as of 14 July 2022,
176,903,501 Ayushmann cards have been issued across the nation, along with
28,923,388 hospital admissions, according to the NHA. Figures for Tamil Nadu are much more impressive with
24,727,093 Ayushman cards generated and
4,838,210 authorised hospital admissions, as of 31 October 2021. The monetary value of these authorised hospital admissions comes at a price of INR
43,528,425,339.
A higher percentage of the educated population has ensured a better scale of awareness and thereby increased willingness to avail of such services.
The fluidity of the programme in Tamil Nadu’s case has been efficient as well as transparent. The numbers also support this statement. The share of claims, by volume, was the highest in Tamil Nadu (
28 percent), followed by Gujarat (17 per cent), according to PM-JAY utilisation data. Even during the COVID-19 pandemic, Tamil Nadu disbursed
INR 393.79 crore for treatments under PM-JAY, which comes to a whopping
INR 1.16 lakh per patient.
The state ranked second in the
NITI Ayog Health Index 2021 and has significantly improved on several important health indicators. According to a case study of Tamil Nadu, Haryana, and Bihar by the NHA, the awareness about PM-JAY was
80 percent in Tamil Nadu as compared to a meagre 20 percent in Bihar. A higher percentage of the educated population has ensured a better scale of awareness and thereby increased willingness to avail of such services.
The collaboration of PMJAY and CMCHIS
A sound partnership is a mandate for implementing any programme in a constructive manner. To implement the Pradhan Mantri Jan Arogya Yojana (PMJAY) scheme in collaboration with CMCHIS, a
Memorandum of Understanding (MoU) was signed on 11 September 2018 between the NHA and the Health and Family Welfare Department, Government of Tamil Nadu. Whilst PM-JAY only covered about
77 lakh (approximately 7 million) families, the CMCHIS gave benefits to an estimated
1.57 crore (15.7 million) families
Regardless of whether they were registered in the PMJAY-CMCHIS, all CMCHIS beneficiaries received the enhanced coverage amount. For beneficiaries who weren’t covered under CMCHIS, the programme has ensured that they are now covered under the revamped PMJAY-CMCHIS.
Tamil Nadu contributes a premium of INR
699 under PMJAY-CMCHIS.
The national government covers 60 percent of the cost for all eligible beneficiaries, which includes 7 million families. Tamil Nadu currently has
681 packages reserved for public hospitals under the PMJAY-CMCHIS scheme. This was only possible due to the already existing strong health system of the state.
PMJAY Modes of Implementation
PMJAY is executed using the hybrid model in Tamil Nadu.
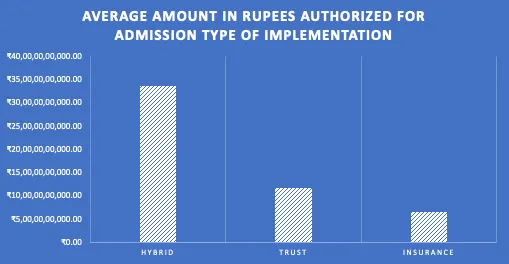
According to National Health Portal, the hybrid model has yielded better claims with the average amount authorised for admissions being markedly higher in comparison to other models. Tamil Nadu, following the hybrid model, ranks third in terms of the average number of hospitalisations/10,000 population availed under the PMJAY-CMCHIS and ranks second in authorising the largest amount of money.
One cannot overlook the fact that Tamil Nadu lags behind when the average amount of money expended per hospital is compared. However, this can be attributed to the superior number of empanelled hospitals, as compared to a considerably moderate population for a large state.
Implications
Tamil Nadu is a developed state that has delivered high-quality treatment through its health efforts even before the advent of PM-JAY. However, families in rural areas who live below the poverty line couldavail PMJAY. The major highlight of the programme is the sizable annual payment of INR 5 lakh to each enrolled family. Now, with better outreach, people below the poverty line would have access to comprehensive health care.
The middle class are not currently covered by this programme and unexpected medical expenses can push these households below the poverty line.
The opportunity to receive premium care from public hospitals and empanelled institutions in the commercial sector has now become feasible. This comes at no extra price, and also curtails the OOPE. The CHEs have also decreased, as expensive procedures for managing cancer and cardiovascular disorders are now provided without charge.
The primary benefit of PMJAY's rollout succeeding at government hospitals is that it is subsequently bolstering the public sector's healthcare offerings. All of these contribute to the nation's progress toward achieving universal health coverage (UHC). The initiative has also started bridging the inequality and health gaps between urban and rural people.
The road aheadPMJAY has become a boon for millions of people across the nation. However, despite the impressive gains, certain healthcare challenges remain in Tamil Nadu, including quality of care and variations in reproductive and child health amongst districts. Tamil Nadu is also dealing with a growing burden of NCDs accounting for nearly
69 percent of deaths in the state. The middle class are not currently covered by this programme and unexpected medical expenses can push these households below the poverty line. PMJAY neglects primary care in favour of concentrating on secondary and tertiary healthcare. This calls into question the necessity of comprehending state-specific healthcare plans, downsizing high OOPE levels, and prioritising primary and preventive healthcare.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.



 India has grown leaps and bounds over the last few decades, in terms of healthcare and social development. Access to healthcare for all classes of society has been a key objective to that end. However, a question that still lingers is have we achieved this objective? The answer lies in achieving Universal Health Coverage(UHC) across all boards, and sections of the population. The National Health Policy 2017 advised the commencement of ‘Ayushman Bharat’ to realise the goal of UHC. In a nation that invests very little funds into healthcare, the out-of-pocket expenses (OOPE) alone account for
India has grown leaps and bounds over the last few decades, in terms of healthcare and social development. Access to healthcare for all classes of society has been a key objective to that end. However, a question that still lingers is have we achieved this objective? The answer lies in achieving Universal Health Coverage(UHC) across all boards, and sections of the population. The National Health Policy 2017 advised the commencement of ‘Ayushman Bharat’ to realise the goal of UHC. In a nation that invests very little funds into healthcare, the out-of-pocket expenses (OOPE) alone account for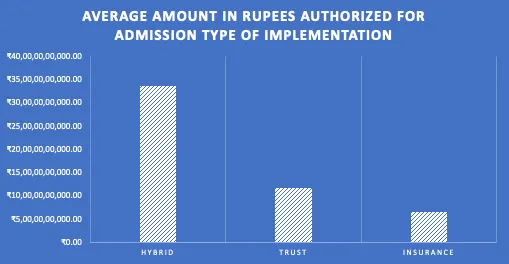
 PREV
PREV

