-
CENTRES
Progammes & Centres
Location
As World Hepatitis Day is being observed, it is imperative to be aware of this public health threat, especially since the incidence of hepatitis cases has increased substantially in post-COVID times.

Hepatitis is a global public health burden, affecting 354 million globally. About 296 million and 58 million people are living with hepatitis B with C, respectively. According to the World Health Organization (WHO), viral hepatitis has led to 1.1 million deaths, and its effects include liver cancer, cirrhosis, etc. Viral hepatitis is preventable, and deaths can be averted by timely diagnosis and treatment. While Hepatitis A and B can be prevented by safe and effective vaccines, Hepatitis E can be reduced with improved sanitation, food safety, and drinking water. Global coverage of the Hepatitis B vaccine in children is 42 percent, with 78 percent coverage in the Western Pacific region and low coverage of 17 percent in the African region.
The target was a 90-percent reduction in new infections and a 65-percent reduction in viral hepatitis-related morbidity by 2030.
In 2016, the World Health Assembly adopted the Global Health Sector Strategy (GHSS) with 2020 and 2030 set as targets for hepatitis elimination. The target was a 90-percent reduction in new infections and a 65-percent reduction in viral hepatitis-related morbidity by 2030. Most countries have failed to meet the 2020 target. At the 75th World Health Assembly 2022, the GHSS 2022-2030 was launched to end viral hepatitis by 2030 in alignment with the Sustainable Development Goals. Following this strategy, WHO has developed a framework for guiding countries and stakeholders seeking validation for the elimination of viral hepatitis with a focus on the hepatitis B virus (HBV) and the hepatitis C virus (HCV).
India has an “intermediate to high endemicity” for Hepatitis B, contributing 25-30 percent of the global load. Hepatitis E virus is a common epidemic in India, while the most dreadful being HBV affects children and HCV causes chronic liver diseases.
In 2018, the Ministry of Health & Family Welfare launched the ‘National Viral Hepatitis Control Programme’ to eliminate HCV and reduce infection, morbidity and mortality rates by HBV & HVC by 2030 in harmony with SDG 3.3. Further to this, in 2019, the ‘National Action Plan for Viral Hepatitis’ was developed to combat the virus through holistic prevention, diagnosis, and treatment strategy.
Despite this, the Global Burden of Disease 2019 estimates 2.93 percent HBV and 0.83 percent HCV prevalence in India. Estimates further reveal that the prevalence, incidence, and death rate from the deadly Acute Hepatitis B and C are highest amongst the Northeastern states led by Arunachal Pradesh, Assam, Meghalaya, and Manipur. It commonly presents as co-infections with HIV/AIDS in the region. While on the other hand, the Empowered Action Group (EAG) states, Uttar Pradesh, Bihar, Jharkhand, and Chhattisgarh have high prevalence and incidence of Acute Hepatitis A and E (fig 1).
Figure 1: Prevalence (per 100,000 population) of Acute Hepatitis for Male and Females across all ages
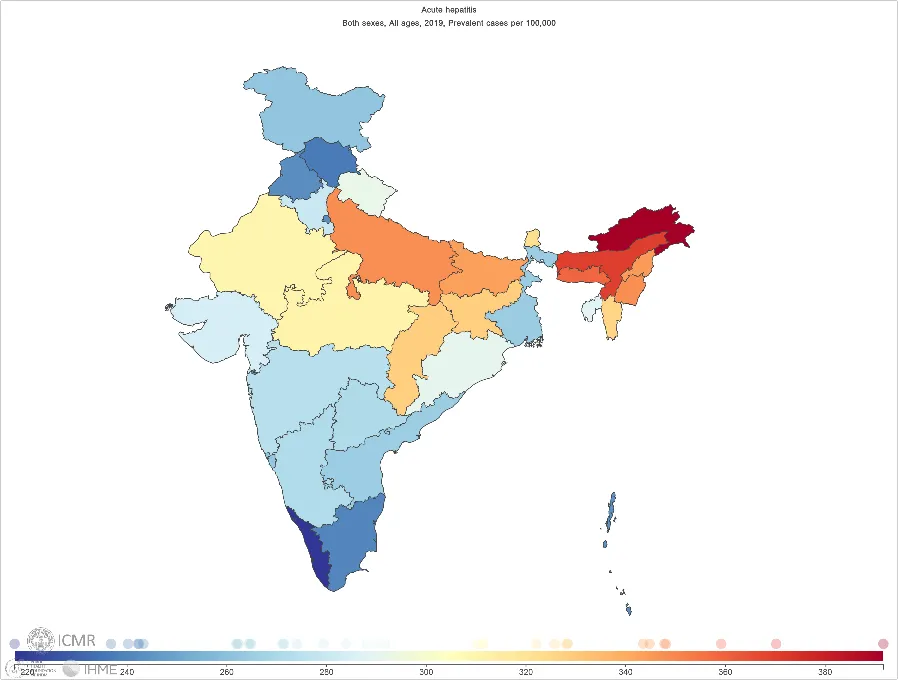 Source: Global Burden of Disease Study (2019)
Source: Global Burden of Disease Study (2019)
A 2014 review on viral hepatitis in India urges the need for increased awareness amongst the public and medical professionals, improved sanitation and safe drinking water and safe blood transfusion to be able to achieve the target of viral hepatitis eradication by ‘2080’. Various factors, including maternal health care utilisation, mother’s education, and family wealth status, show increased chances of HBV vaccination. The high incidence of HBV in Arunachal Pradesh among children is one such likely example of vertical transmission from an infected mother. Other than low immunisation coverage, challenges including lack of awareness of the disease and its mode of transmission, high endemicity sectors like tribals and isolated communities, and stigma and discrimination, also contribute to the prevalence of viral hepatitis.
Despite the coverage increasing significantly from 62.8 per cent in 2015–16 to 83.9 percent in 2019–21, studies have shown marked variation among socio-economic and demographic indicators along with regional variation. This is evident from the National Family Health Survey Report 2019-21 which shows the concentration of poor coverage in the Northeastern region (fig 2).
Figure 2: Vaccination coverage of Hepatitis B vaccine among children aged 12-23 months
As COVID-19 continues to rage on, emerging evidence points towards the delayed presentation of liver diseases. Research has shown that gastrointestinal and liver manifestations in active COVID-19 infection are well-recorded, and its risk factors increase severely with existing comorbidities. These can occur as a new onset of symptoms, resulting from a reaction to the curative drugs or develop post-infection. It has been found in both adults and children leading to liver and kidney disorders.
Pediatric studies from Israel among children who successfully recovered from mild or asymptomatic coronavirus infections found that they later developed acute liver failure with classic hepatitis symptoms. Although it is rare for children to develop hepatitis, the United Kingdom (UK), the United States (US), Denmark, Japan, Italy, France, Canada, and more have reported sudden onset of gastroenteritis illnesses (diarrhoea and nausea) of unknown cause, followed by jaundice. Most of these children tested negative for the 5 hepatotropic viruses but were found positive for adenoviruses (common flu-like viruses). The most widely accepted theory is that the SARS Cov-2 virus may be triggering a severe, atypical response to the immune system together with the adenovirus. In India, too, a systematic Madhya Pradesh study called this phenomenon COVID-Associated-Hepatitis in Children (CAH-C).
Pediatric studies from Israel among children who successfully recovered from mild or asymptomatic coronavirus infections found that they later developed acute liver failure with classic hepatitis symptoms.
Recognising early signs, the incidence of liver diseases and hepatitis will increase in the post-COVID world. As community-level screening and monitoring become deficit, it can become a substantial threat soon. Moreover, a prime concern in Hepatitis management, India lacks national or sub-national data on cases of Hepatitis B and C leading to blinded government efforts. With no effective vaccine for Hepatitis C at the moment, preventative measures become extremely crucial.
The pandemic has further pushed the progress made in eliminating viral hepatitis. A global survey by the World Hepatitis Alliance to assess the impact of COVID-19 on viral hepatitis services indicated a massive disruption of services along with a lack of information on COVID-19 for people with hepatitis. The recent issue of Lancet suggests that despite the challenges, it is possible to achieve the target of eliminating viral hepatitis by expanding efforts and funding.
Figure 3: Key Strategies for elimination of Hepatitis
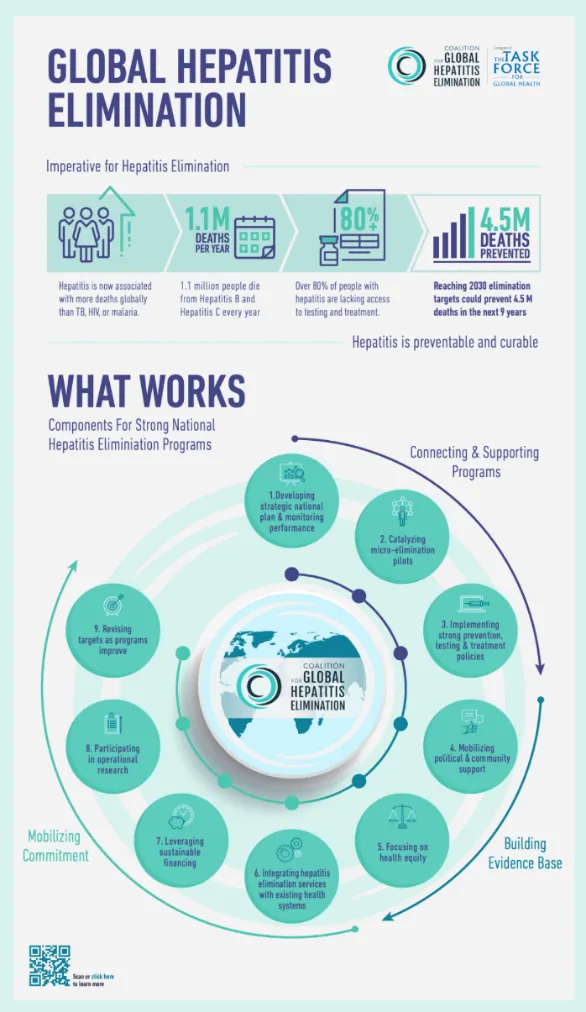 Source: World Hepatitis Alliance
Source: World Hepatitis Alliance
With rising outbreaks, hepatitis management requires special focus as it can easily advance into chronic liver diseases, cancers and cirrhosis. Hepatitis is curable (fig 3) and requires preventive strategies—vigorous screening of the high-risk groups, ensuring safe water and improved sanitation, vaccination, effective monitoring and surveillance of programmes and raising awareness of the risk of viral hepatitis to control the problem.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Mona is a Junior Fellow with the Health Initiative at Observer Research Foundation’s Delhi office. Her research expertise and interests lie broadly at the intersection ...
Read More +
Dr. Shoba Suri is a Senior Fellow with ORFs Health Initiative. Shoba is a nutritionist with experience in community and clinical research. She has worked on nutrition, ...
Read More +