Multimorbidity is becoming a significant health concern in metropolitan regions of India. The World Health Organization (WHO)
defines multimorbidity as the co-occurrence of two or more chronic conditions, significantly straining an individual's overall health and well-being. Anaemia, asthma, diabetes, hypertension, and obesity
are the most common multimorbidities in urban India. Low- and middle-income countries that typically witness a large-scale rural-urban migration
struggle more with this health burden, mainly because of the drastic lifestyle changes experienced when living in or moving to cities. Low-income groups are also more susceptible to many more vulnerabilities as extreme climate events, such as the urban heat island effect, flooding, droughts, etc.,
have direct health implications.
Patterns of occurrence of multimorbidities in urban India
A heterogeneous population in cities because of rapid urbanisation and high rates of in-migration is one of the primary reasons for the higher prevalence of multimorbidities in urban areas. South Indian states of Andhra Pradesh, Tamil Nadu, and Telangana, observed the multimorbidity rates, particularly in large cities such as
Visakhapatnam and
Hyderabad. A
study on the ‘Patterns of Multimorbidity in India’ concluded that uneven access to healthcare between men and women is more pronounced in urban areas, with women being the marginalised group most at risk of developing multimorbidities.
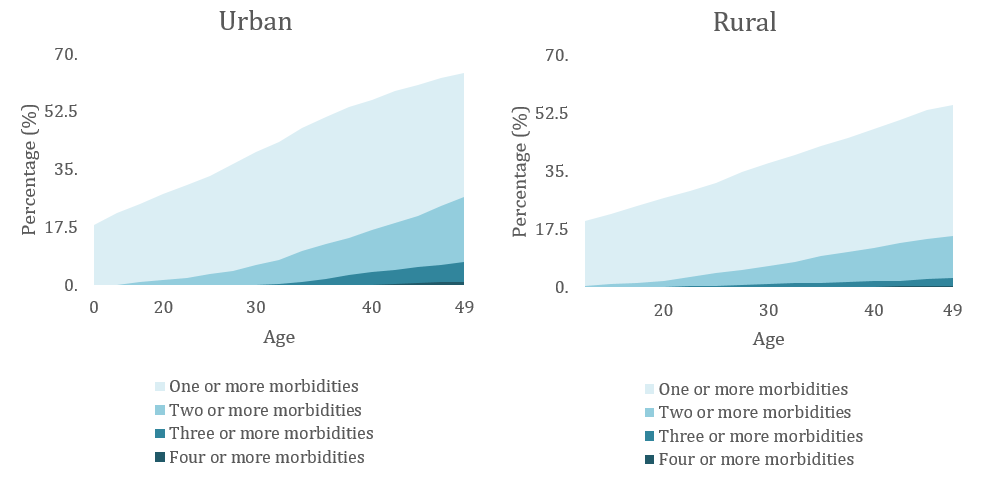
Figure 1: Prevalence of the most common multimorbidities in India
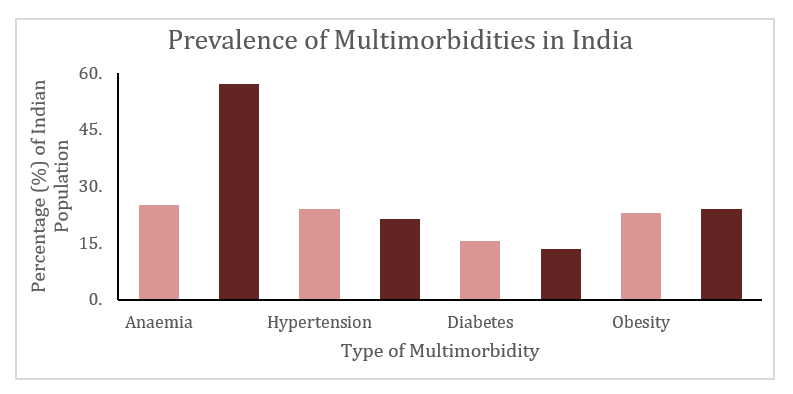
Source:
National Family Health Survey (2019-21)
Rapidly growing population and
epidemiological transitions pose a significant health challenge to India. The prevalence of multimorbidity was higher in urban (9.7 percent) than in rural areas (5.7 percent). The occurrence of at least one multimorbidity in adults between the age 40-49 in urban areas is between 56 to 64 percent, while it is between 39 to 50 percent in rural areas.
Figure 2: Prevalence of multimorbidity in urban vs rural regions in India
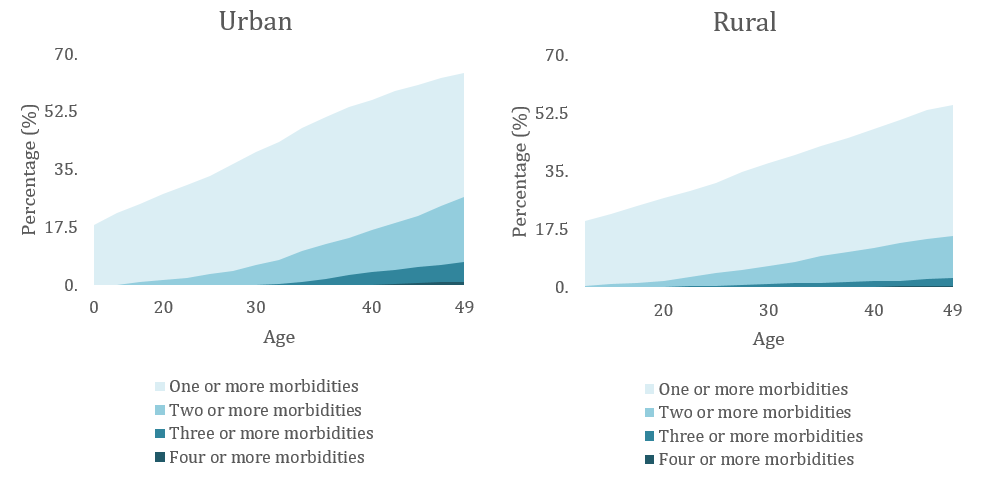
Source:
Patterns of multimorbidity in India: A nationally representative cross-sectional study of individuals aged 15 to 49 years
A study on the ‘Patterns of Multimorbidity in India’ concluded that uneven access to healthcare between men and women is more pronounced in urban areas, with women being the marginalised group most at risk of developing multimorbidities.
The problem worsens as income disparities in cities have caused
disproportionate access to healthcare. Multimorbidity is often closely linked to
high out-of-pocket expenses, impacting lower-income groups in cities. It also imposes
significant costs on health systems. The poorest among the urban poor had a higher prevalence of multimorbidity (47.88 percent) than the poor (41.44 percent). Low-income groups tend to face more
barriers to accessing adequate healthcare, such as affordability, adequate staffing in healthcare setups and even a lack of awareness of their health, and risks posed by a lack of proper and assured access to basic amenities, such as clean drinking water and insufficient sanitation.
Regardless of the socioeconomic group they represent, most people seek treatment for short-term and minor illnesses like a common cold or flu and ignore chronic, long-term diseases.
Studies have also revealed how,
regardless of the socioeconomic group they represent, most people seek treatment for short-term and minor illnesses like a common cold or flu and ignore chronic, long-term diseases. However, even within the socioeconomic groups that get treated for long-term and chronic illnesses, such as diabetes and hypertension, known to be major comorbidities, show high inequity levels because of the significantly longer duration and higher cost of treatment. The ‘inverse care law’ sets in as extensive diagnostic and laboratory testing required for the treatment of such chronic comorbidities escalates the costs further, keeping low-income groups away, inevitably causing decreased access, lesser consultations and increased stress on the physicians.
The importance of tackling multimorbidity was realised during the COVID-19 pandemic, as people with co-morbidities
were more vulnerable to contracting the virus as compared to others. Data collected by various hospitals showed that cities had a higher prevalence of COVID-19 patients with multimorbidities than rural areas (Table 1).
Table 1. Prevalence of Multimorbidity in COVID-19 Patients Across Urban Cities in India
| City |
Prevalence of Multimorbidity in COVID-19 Patients (30-49 age group) |
| Bangalore |
40.7% |
| Delhi |
38% |
| Chandigarh |
29.8% |
| Mumbai |
18.72% |
| Chennai |
17.7% |
Reference:
Prevalence of co-morbidities and its association with mortality in Indian patients with COVID-19: A meta-analysis
Urban environments and its impact on health
Increasingly, cities across the world are experiencing extreme climate events, such as the urban heat island effect (
UHIE) and flash floods. UHIE causes significantly higher temperatures in cities because of the high density of concrete and modern infrastructure, such as roads and buildings, which tend to absorb rather than emit heat.
UHIE leads to increased energy consumption and higher emission of greenhouse gases and other pollutants, negatively impacting human health. For example, heat islands tend to amplify the effects of heat waves, putting individuals at a greater risk of heat stroke.
Other extreme climatic events such as flooding, droughts, and cyclones also
severely impact the health of low-income groups. Extreme heat accelerates droughts which leads to food and water shortages causing
food insecurity, nutritional deficits and diarrheal diseases like cholera. Flooding, especially in cities with poor stormwater management, can lead to water- and vector-borne diseases,
serious injuries and respiratory infections. Low-income groups are more vulnerable to the negative impacts of these climate events given their
substandard living conditions.
Gaps in the healthcare system and proposed solutions
The Indian healthcare system mainly provides vertical healthcare, focusing on single diseases. On the other hand, the millions suffering from multimorbidity require a horizontal healthcare delivery system targeting multiple underlying health conditions rather than individual diseases. A national doctor-to-patient ratio of
0.7 physicians per 1,000 people, and a preference for going to
private hospitals and clinics make healthcare more inaccessible to low-income groups. Despite having insurance schemes and aid available for low-income groups, a limited understanding of health literacy sets is the reason behind the current state of health equity in the country.
The government must, therefore, implement an integrated, horizontal and patient-centred health system on priority. Such integration is possible by increasing screenings under the existing government programmes, such as the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS). More extensive screening of the population would help detect multimorbidities early and work towards their prevention. Furthermore, the government must also establish a more broad-based programme that looks at health conditions such as hypertension, obesity and anaemia collectively.
Ayushman Bharat, or the Pradhan Mantri Jan Arogya Yojana (PM-JAY), is a novel, fully government-financed mission that provides the world’s largest public health insurance and accessible and affordable healthcare, especially to low-income groups. With an insurance cover of INR 500,000 per family, the programme aims to integrate a more horizontal approach by providing comprehensive rather than selective health services. Recently developed programmes such as the Ayushman Bharat Digital Mission (ABDM) aims to support integrated digital health infrastructure in the country. It is working toward preventing multimorbidities and other diseases by improving access to healthcare for low-income groups. This is a constructive step towards integrating a horizontal healthcare system. However, the effectiveness of Ayushman Bharat can be increased significantly by increasing the number of ‘Health and Wellness Centres’ near urban slums so that the urban poor can have easier access and lesser out-of-pocket expenditure on healthcare. The government must also conduct community awareness and training workshops to enable ABDM’s more extensive utilisation.
Conclusion
It is vital to understand that there is a strong correlation between living in urban areas and socioeconomic standing with access to healthcare. Several
studies have shown that India’s rapid urbanisation and in-migration to cities have caused large disparities in access to healthcare between high-income and low-income groups. It is imperative to address these gaps to reduce the spread of multimorbidities and other chronic health conditions.
Anagha Nair is a Research Intern at Observer Research Foundation.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.



 Multimorbidity is becoming a significant health concern in metropolitan regions of India. The World Health Organization (WHO)
Multimorbidity is becoming a significant health concern in metropolitan regions of India. The World Health Organization (WHO) 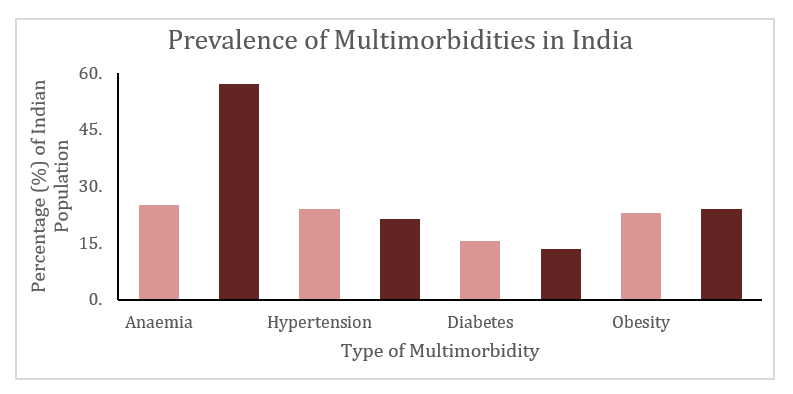
 PREV
PREV