
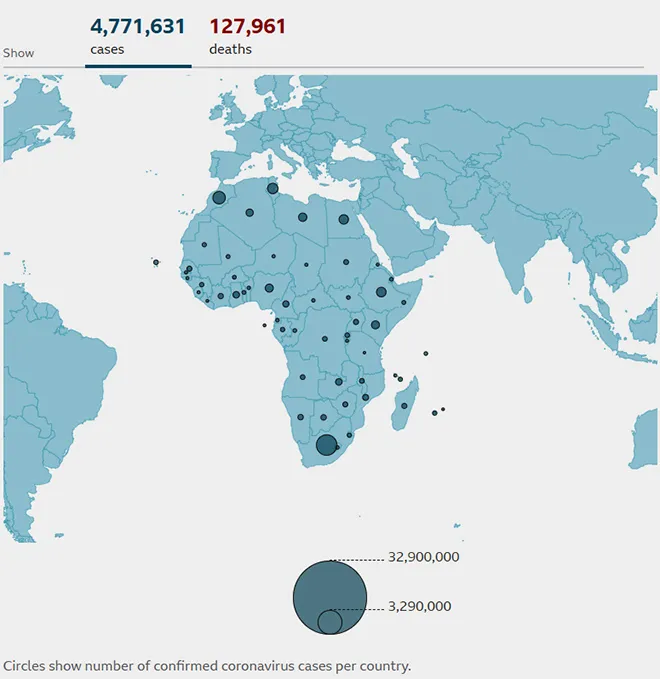
Africa reported its first case of COVID-19 on 14th February, 2020 in Egypt. Seven countries, including Benin, Eritrea, Eswatini, Liberia, Nigeria, Sierra Leone, and South Africa (figure 1) show an increase in cases; the highest number of new cases reported is from South Africa (49.4 percent). Testing in most of the African countries has seen multidimensional challenges such as lack of trained manpower and health infrastructure. The Lancet indicates slow testing, with 17 countries reporting less than the recommended ten to 30 tests per case.
Figure 1: Coronavirus status in Africa (as of 21st May 2021)
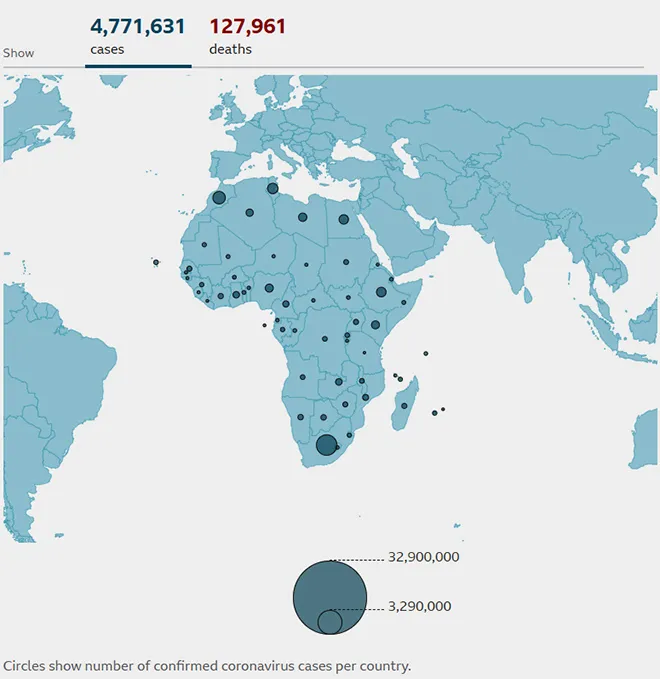 Source: Johns Hopkins University, national public health agencies
Source: Johns Hopkins University, national public health agencies
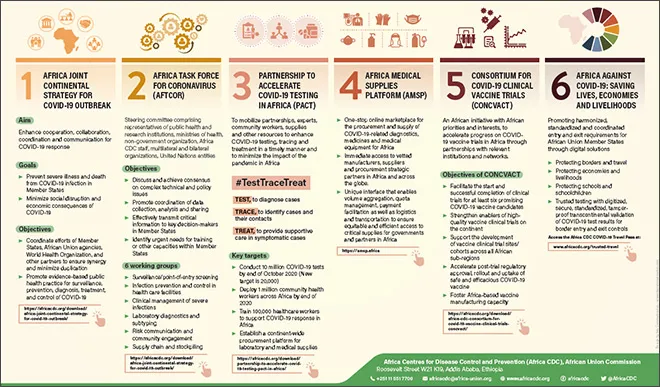
The African Centre for Disease Control and Prevention has rolled out several initiatives (figure 2) targeting surveillance and testing, medical supplies, vaccine trials, public health, and social measures for saving lives, economies, and livelihood.
Figure 2: Africa CDCs COVID-19 Pandemic Response Initiatives
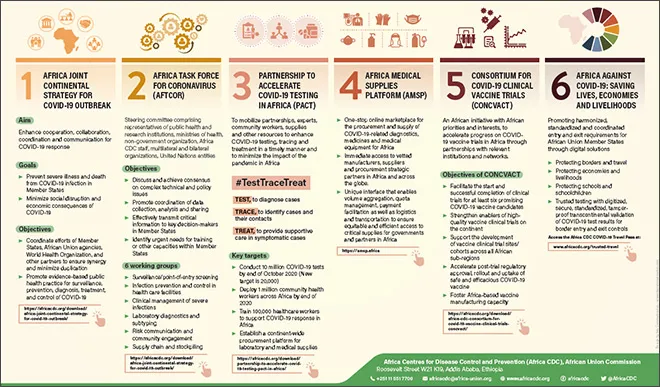 Source: Africa CDC
Source: Africa CDC
Africa’s healthcare system faces multiple challenges ranging from lack of funds, low healthcare workforce, and its high burden of disease. The pandemic has further aggravated the challenge adding to the existing double burden of communicable and non-communicable diseases along with poverty, poor health literacy, and weak health systems. Healthcare workers are also facing mental stress, physical exhaustion, and separation from families; therefore, this calls for their safety and mental well-being.
The African continent saw an aggressive second wave with many more cases by the end of 2020 as compared to the first wave. Many factors were responsible, including less stringent public health and social measures, COVID-19 variants, and lockdown fatigue. Improved monitoring of COVID-19 data and local solutions may have kept the continent safe from the angst of a third wave.
The African continent saw an aggressive second wave with many more cases by the end of 2020 as compared to the first wave. Many factors were responsible, including less stringent public health and social measures, COVID-19 variants, and lockdown fatigue
COVID-19 has caused substantial disruption to health services in African countries. A modelling study indicates an increase in deaths up to 10 percent, 20 percent, and 36 percent due to HIV, tuberculosis (TB), and malaria respectively during the pandemic for low- and middle-income countries. Sub-Saharan Africa needs to prioritise access to insecticidal nets and antimalarial treatment to prevent malaria epidemics. A study from Kenya indicates long-lasting TB burden—about 25,000 additional cases due to the lockdown disruptions. The pandemic has led to disturbance in the provision of HIV services in Sub-Saharan Africa adding to the HIV death burden. Another analysis of HIV treatment indicated that a disruption in treatment caused by COVID-19 could result in an additional 500,000 HIV deaths in Africa.
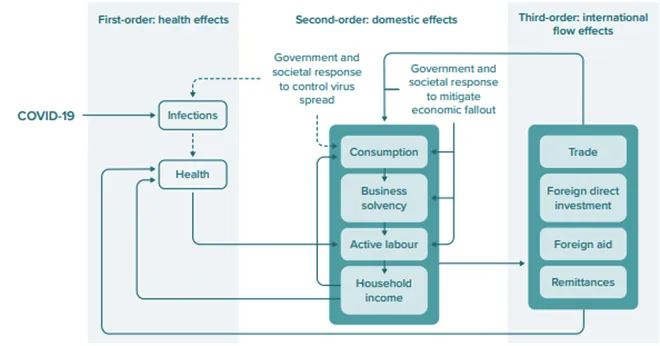
A recent report by UNDP, analysing the long-term socio-economic impact of COVID-19 in the African continent conceptualises across three systems: Human, domestic, and international flow effects (figure 3). The study states that all these factors are interlinked, with effects on human health such as changing patterns of mortality and morbidity, while simultaneously decreasing economic activity and affecting the international economic system. The long-term impact of COVID-19 will push back the gains and lead to increasing child mortality and poverty by 2025 and 2030. The report calls for increased investment in health infrastruture, children, and youth to minimise the indirect economic and health impacts on future generations.
Figure 3: Conceptual framework outlining the macroeconomic effects of COVID-19, through health effects, domestic effects and international flow effects
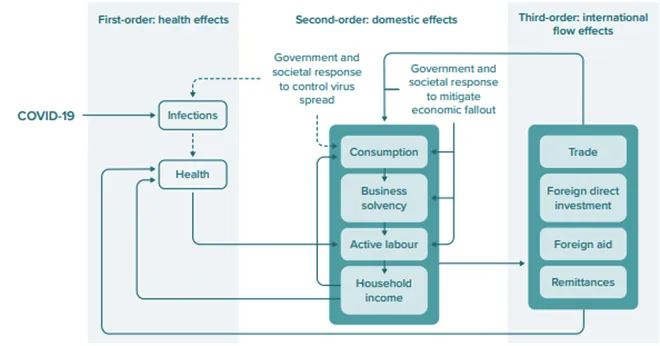 Source: UNDP
Source: UNDP
Women and children have also been disproportionately affected due to the pandemic in the African continent. With COVID-19 pushing 150 million people around the world into extreme poverty, many countries like Kenya and Nigeria have been impacted. The movement restriction due to the pandemic has had implications on food security for Africa and has led to calls for stregthening food security and safety net policies and programmes. The closure of schools has seen a direct impact on nutrition and the youth’s ability to earn, thus, leading to loss of human capital. Antenatal care services have been grossly impacted during the pandemic due to lack of healthcare resources. A report from Kenya, Tanzania, and Uganda shows adverse impact of COVID 19 on antenatal services. This will further add to the high neonatal and maternal mortality rate in the countries, pushing back the target of achieving the SDG of reducing maternal mortality ratio.
Similar to the consequences of the Ebola outbreak, the COVID-19 pandemic has severely impacted mental health in Africa. Healthcare workers, COVID-19 patients, children, youth, and the elderly suffer from anxiety and depression. The pandemic response should integrate mental health education and counselling along with psychosocial support during and after the pandemic. Findings from Kenya, Uganda, and South Africa on the indirect heath effects of COVID-19 showed disruptions in essential health services, and the consequent adverse health effects of said disruptions. It suggests to invest in the generation of local data and evidence for both facility- and community- level to tailor response measures and recovery efforts. An online survey conducted in East and West Africa finds peer-to-peer communication beneficial in promoting COVID-19 policy compliance.
While the pandemic has negatively affected the health and economy of many countries, it also provides an oppurtunity to reshape healthcare systems. Matshidiso Moeti, Regional Director for Africa at the World Health Organisation (WHO) supports ‘implementing universal health coverage programmes, emphasising primary and preventive healthcare as well as digital innovations and better preparedness for epidemics.’
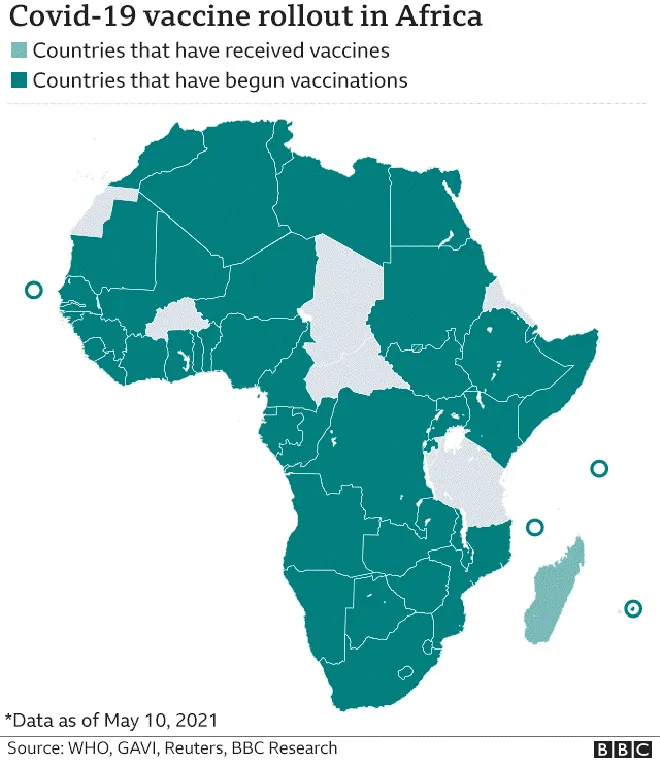
The COVID-19 vaccination drive has been off to a slow start since it began on 1 March 2021. The vaccination rollout has been varied across the African continent mainly due to scant supply of vaccines and financial crunch. Stoppage of vaccine shipment through COVAX has further added to Africa’s woes.
The COVID-19 vaccination drive has been off to a slow start since it began on 1 March 2021. The vaccination rollout has been varied across the African continent mainly due to scant supply of vaccines and financial crunch
Figure 4: COVID-19 vaccine roll out in Africa
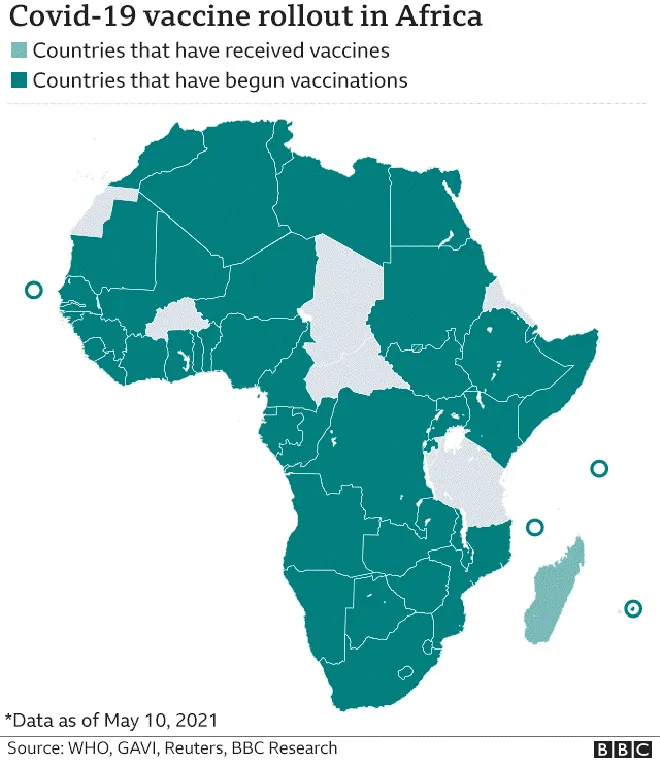 Source: WHO, GAVI, Reuters, BBC Research
Source: WHO, GAVI, Reuters, BBC Research
As of May 10, most African countries have begun vaccination (figure 4), but nine countries have administered less than a quarter the doses received, and 15 countries have given half of the doses received. Reasons for slow rate of vaccination are inequal distribution of vaccines, lack of healthcare infrastructure, and vaccine hesitancy and scepticism, to name a few. Africa’s vaccine coverage is the lowest at about eight doses as opposed to the 150 doses per 1,000 people being administered globally.
Another constraint on vaccination is from the evidence of increased breakthrough rates of coronavirus variant BNT162b2 on Pfizer-BioNTech vaccinated individuals. A recent study in The Lancet on impact and effectiveness of BNT162b2 variant of concern on coronavirus cases, hospitalisation, and deaths suggests effectivity of vaccine across age groups in preventing both symptomatic and asymptomatic SARS-CoV-2 infections. An increase in vaccine coverage have been found to decrease incidence of infection.
COVID-19 has further exposed weaknessed in African economies and heightened healthcare deficiencies. The World Bank speculates that Africa requires US $100 billion to tackle COVID-19 impact across sectors. Africa needs to scale up and adapt safety net programmes and ensure food scurity to overcome the impact of the pandemic on their livelihoods. A review of the impact of the pandemic on equitable access to essential medicines and vaccines for universal health coverage in Africa calls for a multipronged approach for sustainable healthcare reforms; and minimising social and economic risk associated with the pandemic. Investments and reforms in health-and social care and harnessing innovations like e-health is the need of the hour for a robust and sustainable recovery from COVID-19.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.




 PREV
PREV


