Introduction
In India, a country with a vast population and a diverse socio-economic fabric, healthcare remains fraught with challenges including disparities in access. These socio-economic disparities are deep, and they influence health outcomes.
It is imperative to bridge these gaps amid the ongoing epidemiological, nutritional and demographic transitions that are bringing about massive challenges in healthcare. Cancer, for example, has emerged as a significant cause of mortality across the country. The impact of cancer in India transcends health and affects the economic and social spheres of people’s lives. A key aspect of this challenge is the financial burden borne by families dealing with the illness: According to the latest available data from 2018, out-of-pocket (OOP) expenditure accounts for over 50 percent of total health spending.[1] This financial burden is exacerbated by inequities in access to and the affordability of cancer treatment.
Compounding the scenario is the distribution of healthcare facilities between the public and private sectors. Approximately 42 percent of the population, primarily in the rural regions, rely on public hospitals for hospitalised treatment; the majority, mostly living in urban areas, turn to private hospitals. This divide is more pronounced in outpatient care, with a large portion of ailments being treated by the private sector, particularly in urban areas.[2]
Latest available data (2017–18) on the healthcare expenditure landscape of India (Table 1) highlights the financial demands on those seeking medical care for various ailments. Cancer treatment stands out as the most financially demanding ailment, with average expenditures in private hospitals approaching INR 93,305 per hospitalisation; in public hospitals, the average is INR 22,520.[3]
When considering the cost across all hospitals, including charitable and trust-run institutions, cancer care averages INR 61,216 per hospitalisation—a massive financial challenge for large portions of the population.[4] This figure dwarfs expenses associated with other serious conditions such as cardiovascular and neurological disorders. These numbers are of particular concern in the broader context of India’s healthcare system, where OOP expenses account for a significant portion of healthcare financing.[5] High OOP expenses can lead to catastrophic spending for households, potentially pushing families into poverty, especially in a country where a large segment of the population rely on daily wages or are part of the informal sector.
The financial implications extend beyond immediate treatment costs to long-term impacts on the economic well-being of individuals and communities. For many, the high costs of treatment in private hospitals translate to outright denial of access to healthcare services. The economic strain is compounded by the lack of comprehensive health insurance coverage for a majority of the population, making the need for effective healthcare policies and financial protection mechanisms more critical than ever.[6] The data should urge policymakers to bolster the public healthcare system and improve the affordability and accessibility of medical care, ensuring that the financial burden of illness does not become a debilitating life sentence for India’s poor.
Table 1: Average Medical Expenditure per Hospitalisation (2017-18)
| Category of Ailment |
Public Hospitals |
Private Hospitals |
All Hospitals* |
| Cancers |
22,520 |
93,305 |
61,216 |
| Psychiatric and neurological ailments |
7,235 |
41,239 |
26,843 |
| Cardio-vascular ailments |
6,635 |
54,970 |
36,001 |
| Musculo-skeletal ailments |
5,716 |
46,365 |
32,066 |
| Genito-urinary ailments |
5,345 |
33,409 |
24,770 |
| Gastro-intestinal ailment |
3,847 |
29,870 |
19,821 |
| Respiratory ailments |
3,346 |
24,049 |
13,905 |
| Eye ailments |
2,605 |
18,767 |
10,912 |
| Infections |
4,052 |
15,208 |
9,064 |
| Overall |
4,452 |
31,845 |
20,135 |
*’All Hospitals” includes charitable, NGOs, and trust-run hospitals. All values are average medical expenditure in Indian rupees (INR) per case of hospitalisation.
Source: Ministry of Statistics and Programme Implementation (2018)[7]
Table 2 further disaggregates the average medical expenses for hospitalisation by rural and urban regions. In the rural areas, where incomes are generally lower and access to healthcare is more challenging, the average expenses for the treatment of any ailment in public hospitals are lower (INR 4,290) compared to their urban counterparts (INR 4,837). However, this relief is overshadowed by the exorbitant costs in private hospitals, with rural inhabitants paying as much as INR 85,326 for cancer treatments—comparable to the average annual income of an Indian farmer. Urban residents face their own set of financial challenges, with the average cost of treating cancer in private hospitals reaching INR 106,548, suggesting that urban infrastructure and healthcare accessibility may not necessarily translate to affordability.
Table 2: Average Medical Expenditure per Hospitalisation (2017-18)
| Sector |
Category of Ailment |
Public Hospitals |
Private Hospitals |
All (incl. NGOs, trust-run) |
| Rural |
a. Infections |
2,149 |
14,102 |
8,005 |
| b. Cardio-vascular ailments |
6,919 |
42,759 |
27,136 |
| c. Gastro-intestinal ailment |
3,456 |
26,745 |
16,833 |
| d. Respiratory ailments |
3,386 |
19,846 |
11,625 |
| e. Genito-urinary ailments |
5,284 |
26,611 |
19,674 |
| f. Musculo-skeletal ailments |
4,722 |
37,729 |
25,572 |
| g. Psychiatric and neurological ailments |
6,868 |
33,654 |
21,806 |
| h. Eye ailments |
2,421 |
15,767 |
8,747 |
| i. Cancers |
23,905 |
85,326 |
56,996 |
| Any ailment |
4,290 |
27,347 |
16,676 |
| Urban |
a. Infections |
1,822 |
16,843 |
10,992 |
| b. Cardio-vascular ailments |
6,152 |
68,920 |
47,788 |
| c. Gastro-intestinal ailment |
5,003 |
35,442 |
26,202 |
| d. Respiratory ailments |
3,274 |
30,111 |
17,670 |
| e. Genito-urinary ailments |
5,468 |
44,001 |
33,272 |
| f. Musculo-skeletal ailments |
8,164 |
60,657 |
44,526 |
| g. Psychiatric and neurological ailments |
8,052 |
53,420 |
36,082 |
| h. Eye ailments |
3,031 |
23,568 |
15,064 |
| i. Cancers |
19,982 |
106,548 |
68,259 |
| Any ailment |
4,837 |
38,822 |
26,475 |
Source: Ministry of Statistics and Programme Implementation (2018)[8]
The high costs in private hospitals across both rural and urban sectors imply that, without adequate insurance coverage, families are likely to incur considerable financial strain. The threat of slipping into poverty increases too, due to such healthcare expenses. There is an urgent need for a more equitable healthcare system that can mitigate OOP expenditures for the average Indian, particularly in life-threatening ailments such as cancer, and bridge the gap between rural and urban healthcare economies. The introduction in 2018 of Pradhan Mantri Jan Arogya Yojana (PMJAY), a national health insurance scheme covering a vast number of poor households across the country may have changed the situation, although the absence of more recent survey data does not allow a proper comparison of the current situation with the pre-PMJAY days analysed here.
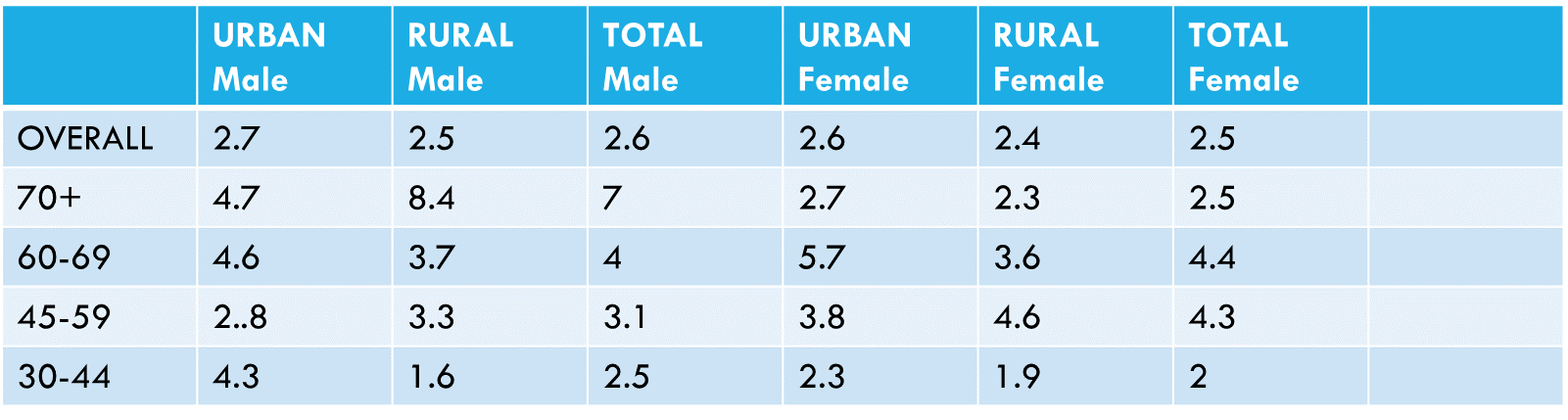
The distribution of hospitalised cancer cases in India for 2017–18, as a percentage of total hospitalisations (Table 3), reveals notable disparities across gender and urban-rural divides. Overall, the incidence of hospitalisations due to cancer is slightly higher for males (2.6 percent) than for females (2.5 percent), with the most pronounced difference observed in the rural elderly population, where 8.4 percent of males over 70 are hospitalised for cancer, compared to 2.3 percent of females. This suggests higher exposure to risk factors or delayed healthcare access among rural males. Urban women aged 60–69 have a higher hospitalisation rate for cancer (5.7 percent) than rural women (3.6 percent), potentially indicating better detection and healthcare access in urban areas. However, rural females aged 45–59 have a higher hospitalisation rate (4.6 percent) than urban females (3.8 percent). This data hints at the complex interplay of environmental, lifestyle, and socio-economic factors that affect cancer incidence and the utilisation of healthcare services. Therefore, there is also a need for tailored healthcare strategies that address the specific needs and challenges of different demographic groups in the context of cancer care in India.
Table 3: Percentage Distribution of Hospitalised Cancer Cases (2017-18)
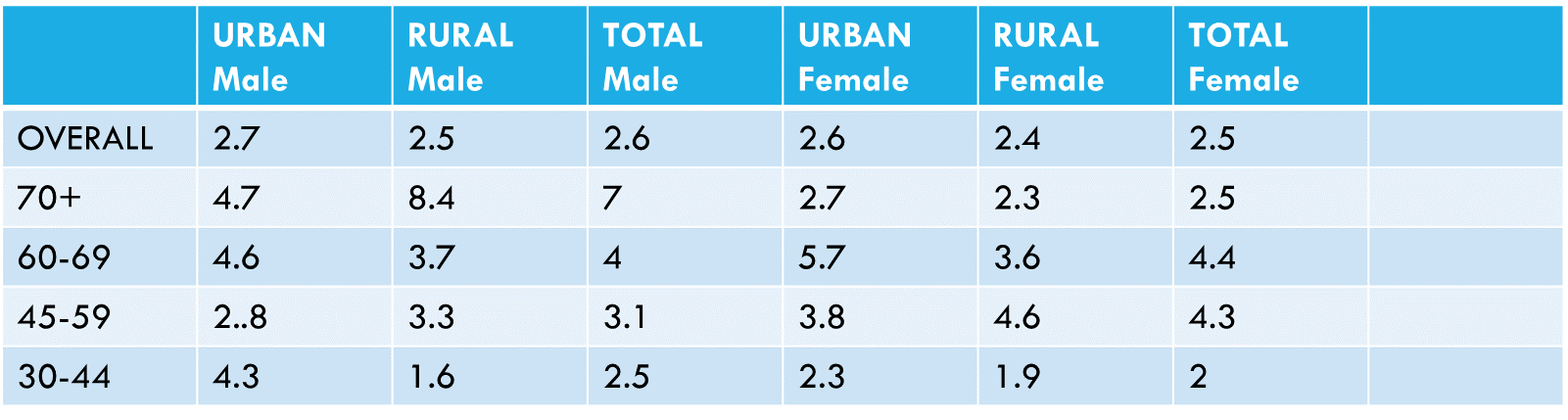
Source: Compiled by the author, from Ministry of Statistics and Programme Implementation (2018)[9]
The data on outpatient care (Table 4) indicates that cancer treatment incurs substantial costs across different types of healthcare facilities. The average expenditure for cancer treatment is highest in private hospitals, with an average cost of INR 4,475 per outpatient visit. This is higher than in government or public hospitals, where the average cost is INR 2,231. Charitable or trust-run NGO hospitals also have lower average costs (INR 1,579) than private clinics. The average expenditure in informal healthcare providers is INR 1,905, which is higher than both private clinics and NGO-run hospitals, suggesting that patients might be paying a premium even in less formal settings, potentially due to the perceived urgency or unavailability of services in other sectors.
This high cost of cancer treatment in private settings could be indicative of more advanced or specialised care, or more expensive drugs and therapies that are not available in public or NGO-run facilities. The data underscores the financial challenges faced by cancer patients, particularly if they require or opt for treatment in private healthcare facilities.
Table 4: Average Medical Expenditure per Outpatient Visit (2017-18)
| Broad Ailment Category |
Govt./Public Hospitals |
Charitable/Trust/NGO-run Hospitals |
Private Hospitals |
Private Doctors/Clinics |
Informal Health Care Providers |
All (incl. n.r.) |
| Infection |
265 |
391 |
1,106 |
556 |
273 |
541 |
| Cancers |
2,231 |
1,579 |
4,475 |
1,768 |
1,905 |
2,869 |
| Blood diseases |
217 |
1,137 |
3,443 |
1,505 |
85 |
1,509 |
| Endocrine, metabolic |
229 |
1,037 |
807 |
717 |
222 |
552 |
| Psychiatric & Neurological |
597 |
1,366 |
1,770 |
638 |
336 |
964 |
| Eye |
361 |
410 |
1,592 |
510 |
237 |
690 |
| Ear |
435 |
850 |
786 |
599 |
1,602 |
621 |
| Cardio-vascular |
819 |
481 |
747 |
570 |
309 |
540 |
| Respiratory |
251 |
211 |
962 |
474 |
171 |
482 |
| Gastro-intestinal |
362 |
453 |
1,147 |
796 |
582 |
751 |
| Skin |
384 |
400 |
809 |
650 |
335 |
602 |
| Musculo-skeletal |
441 |
494 |
969 |
794 |
264 |
766 |
| Genito-Urinary |
844 |
2,563 |
1,841 |
1,143 |
918 |
1,743 |
| Obstetric |
694 |
308 |
963 |
929 |
138 |
1,694 |
| Injuries |
801 |
446 |
2,463 |
929 |
338 |
1,256 |
| Other |
518 |
1,214 |
3,095 |
628 |
156 |
1,331 |
| All |
331 |
732 |
1,062 |
624 |
552 |
636 |
Source: Ministry of Statistics and Programme Implementation (2018)[10]
This report examines the interplay of health and socio-economic contexts in cancer care in India with the aim of highlighting the multifaceted challenges posed by cancer, including rising incidence rates due to epidemiological changes, the financial burden on families, and the societal implications of these health and economic pressures. The report seeks to provide insights into the complexities of managing cancer care in a socio-economically diverse and populous nation like India.
Economic and Social Burden of Cancer in India
The financial burden of healthcare can often lead to impoverishment, compounded by indirect costs like loss of income and decreased productivity.[11] These economic challenges are not isolated but create ripple effects through the economy, affecting societal welfare and development. For those suffering from cancer, the financial cost is even higher.
Cancer also has an associated stigma that can lead to isolation and discrimination, severely impacting the mental health and well-being of patients. This stigma, rooted in cultural beliefs and lack of awareness, exacerbates the challenges faced by patients, hindering timely and effective treatment. The psychological toll of cancer extends to caregivers and families, disrupting family dynamics and often leading to a diminished quality of life.[12] Such emotional burden of the disease is often overlooked but is equally debilitating.
The demographic shifts towards an aging population and changes in lifestyles are contributing to an increase in the prevalence of cancer, presenting additional challenges for India’s healthcare system. The imperative is to re-evaluate health priorities and resource allocation to cater to the evolving landscape of cancer care.[13] Furthermore, the disparities in cancer incidence and outcomes across different socio-economic and geographical regions highlight the unequal burden of cancer in the country; patients in rural or economically disadvantaged areas face more significant challenges in accessing care, leading to worse outcomes.[14]
Addressing the multifaceted challenges posed by cancer in India requires a multidimensional approach that encompasses medical interventions, financial support, social awareness programmes, and policies targeting the broader socio-economic factors that influence cancer incidence and outcomes. Such an approach should aim to reduce the stigma associated with cancer, improve accessibility and affordability of care, and enhance the support systems for patients and families. By tackling these issues, India can make strides towards a more comprehensive and equitable cancer care system.
Public and Private Healthcare in Cancer Care
In India, the public healthcare system plays a crucial role in providing cancer care, particularly for populations in rural and underserved areas. However, the public healthcare sector faces various challenges, including inadequate infrastructure, a shortage of healthcare professionals, and limited access to advanced cancer treatments.[15] These limitations often result in disparities in cancer care availability and quality. Meanwhile, the private healthcare sector offers cutting-edge technology and specialised cancer care. The high costs, however, make private-sector care inaccessible to a large proportion of the population.[16]
In recent years, there has been a growing focus on public-private partnerships and initiatives aimed at bolstering the capacity of the public healthcare system in order to address these challenges. These efforts include the establishment of more comprehensive cancer centres, enhanced training for healthcare professionals, and increased government investment in healthcare infrastructure. Such initiatives are critical in bridging the gap between the public and private healthcare sectors, ensuring that advanced cancer care becomes more accessible and equitable across all sections of society.
These measures extend beyond improving healthcare facilities to also involve a paradigm shift in how cancer care is approached in the country. Enhancing the synergy between public and private sectors leads to increased potential to create a more integrated and efficient healthcare system that can provide high-quality cancer care to all, irrespective of their economic status or geographical location. This collaborative approach is essential to ensure that India’s cancer care system is responsive, resilient, and capable of meeting the diverse needs of its population.
Government Initiatives and Policies in Cancer Care
The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PMJAY) offers health insurance up to INR 5 lakhs per family per year for secondary and tertiary care hospitalisation, covering many cancer-related treatments. Additionally, the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS) aims to prevent and control chronic non-communicable diseases, including cancer. Another critical initiative is the Rashtriya Arogya Nidhi (RAN), which provides financial assistance to patients living below the poverty line who suffer from life-threatening diseases, including cancer, allowing them to receive medical treatment at government hospitals.
For their part, the State Illness Assistance Funds, set up by various state governments, offer financial aid to poor patients to cover treatment costs for different diseases, including cancer. Furthermore, the Health Minister’s Cancer Patient Fund (HMCPF) within Rashtriya Arogya Nidhi provides financial assistance for cancer treatment through the procurement of generic drugs. The Tertiary Care Cancer Centres (TCCC) scheme aims to set up state cancer institutes and tertiary care cancer centres across the country to improve facilities for cancer treatment. This is complemented by the Pradhan Mantri Swasthya Suraksha Yojana (PMSSY), which includes the establishment and upgrade of government medical colleges and institutions, enhancing resources for cancer care and strengthening the National Cancer Grid (NCG). NCG is a network of cancer centres (both public and private), research institutes, patient groups, and charitable institutions across India that aim to establish uniform standards of patient care for the prevention, diagnosis, and treatment of cancer and provide specialised training and education in oncology.[17]
Policy measures targeting tobacco control and the promotion of healthy lifestyles are vital in reducing the risk factors associated with cancer. Public awareness campaigns about cancer that emphasise the importance of early detection and lifestyle changes are a crucial part of the government’s strategy.[18] These campaigns are aimed not only at educating the public but also reducing the stigma associated with cancer, thereby encouraging more people to seek timely medical help.
Integrating these cancer-specific initiatives with broader health policies is essential for a comprehensive approach to cancer care in India. By aligning cancer care strategies with overall health system strengthening, the government can ensure a more effective and sustainable impact. This integrated approach is crucial for addressing the complex challenges posed by cancer, including the need for improved healthcare infrastructure, better-trained healthcare professionals, and more equitable access to advanced treatments.[19] These initiatives underscore the need for ongoing efforts to enhance cancer care in India, including additional investments in infrastructure, research, and human resources, as well as collective action for research collaboration and awareness to improve cancer care and outcomes across the country.
One of the most promising steps in cancer care in India is the First Cancer Care (FCC) initiative, introduced in 2022. This forward-thinking programme utilises advanced technology to transform cancer prevention and treatment, focusing on quality, timeliness, precision, and fairness. The FCC initiative provides a comprehensive framework that encompasses prevention, early detection, curative care, and governance. It aims to optimise the entire patient journey. Incorporating data analytics and AI, the initiative is poised to usher in a new era of predictive modelling in cancer care, enabling personalised and more effective treatment strategies.[20] This approach could serve as a beneficial model for other countries in the Global South, demonstrating India's role in integrating technology with healthcare.
Societal Behaviours and Stigma
In India, societal attitudes and behaviours play a critical role in shaping cancer care outcomes. Stigma associated with cancer often leads to delayed diagnosis and treatment, adversely affecting survival rates. Cultural beliefs and misconceptions about the disease contribute to this stigma, resulting in social isolation and psychological distress for patients as well as their families.[21]
To address this challenge, concerted efforts in the form of awareness campaigns, community engagement programmes, and educational initiatives are crucial. These efforts can serve to dispel myths and misconceptions about cancer, reduce the associated stigma, and encourage early screening and treatment.[22] Public awareness campaigns, particularly those involving survivors who share their experiences, can help change perceptions and reduce fear and misinformation surrounding the disease. Moreover, integrating cancer education into broader health and wellness programmes can help normalise discussions about cancer and its treatment. Community engagement, especially in rural and semi-urban areas, is vital to reach a wider audience. Empowering community health workers to spread awareness and promote early detection practices can also impact cancer care outcomes.
A supportive and understanding environment for cancer patients can be fostered by changing societal perceptions and reducing stigma. This shift is essential for improving cancer outcomes and ensuring that patients receive the care and support they need in their treatment journey. Addressing these societal barriers is a vital step towards enhancing the overall effectiveness of cancer care in India.
Challenges and Future Projections
The growing burden of cancer in India is exacerbated by demographic shifts, including an aging population and changes in lifestyle factors, which contribute to the increasing prevalence of the disease.[23] A robust response that encompasses a strengthening of healthcare infrastructure is therefore essential. This includes the need for more comprehensive healthcare facilities equipped to handle complex cancer treatment regimens and increased funding for cancer research to develop more effective and tailored treatment approaches.[24]
Future projections for cancer incidence in India highlight the urgent need for a comprehensive national cancer control plan that covers a wide range of elements, including prevention strategies, early detection methods, effective and accessible treatment options, and palliative care. The focus should also extend to addressing the broader economic and social impacts of cancer on patients and society. Reducing this burden is crucial for improving the overall outcomes and quality of life for cancer patients.
This comprehensive approach must be dynamic and adaptable, considering the rapidly evolving nature of healthcare needs and cancer treatment technologies. Collaborative efforts involving government bodies, healthcare providers, research institutions, and community organisations will be key to implementing this plan effectively. By confronting these challenges and adopting a forward-thinking strategy, India can make significant strides in improving cancer care and outcomes for its population.
Technological and Research Advancements
Advancements in medical technology and research are pivotal for enhancing cancer care. The adoption of new technologies, including precision medicine and targeted therapies, is a significant step forward. These advancements offer the potential for more personalised and effective cancer treatment. However, challenges such as the affordability and accessibility of these advanced treatments pose hurdles, particularly in under-resourced areas.[25]
Further, investment in research and development tailored to the Indian context is vital. This includes focusing on the types of cancers that are most prevalent in India and understanding the unique genetic and environmental factors influencing these cancers.[26]
Embracing technology and innovation in healthcare is key to improving the quality and effectiveness of cancer treatment in the country. This approach involves the adoption of new treatment modalities as well as leveraging digital health technologies for better patient management and care coordination.[27] By prioritising these areas, India can make strides in enhancing its cancer care capabilities, thus improving outcomes for patients.
International Collaboration and Support
International collaboration plays a pivotal role in advancing cancer care in India. Engaging with global health organisations and participating in international research collaborations offer valuable opportunities to share best practices and gain insights into advanced cancer care techniques. These partnerships can be instrumental in bringing expertise, resources, and innovative approaches to India, enhancing the country’s ability to address the complexities of cancer care.[28] Collaborations with international research institutions also foster a culture of innovation within India, which can lead to groundbreaking advancements in cancer treatment and care.
These international collaborations also enable alignment with global cancer care standards and protocols. Support from international entities in the form of funding, technical assistance, and knowledge exchange is vital for developing India’s healthcare infrastructure. This includes the construction of facilities as well as the training of healthcare professionals in the latest cancer treatment and care methodologies. Additionally, implementing effective cancer control strategies that are influenced by successful models from around the world can significantly improve the scope and quality of cancer care in India.
Engaging in a global dialogue about cancer care is essential for India to effectively manage and mitigate its growing cancer burden.[29] Such engagement facilitates the exchange of ideas and experiences, fostering a collaborative environment where India can both contribute to and benefit from global advancements in cancer care. This international cooperation is key to developing a more robust, comprehensive, and effective approach to cancer care in India.
The Way Forward
As India confronts the escalating challenges of cancer care, it is imperative to chart a strategic path forward, capitalising on current strengths while addressing critical gaps. The following recommendations offer a blueprint for enhancing India’s approach to cancer management, with a focus on augmenting early detection, optimising healthcare infrastructure, and leveraging sustainable financing and community engagement. Implementing these strategies will not only align with the nation’s healthcare objectives but also advance India’s capacity to provide comprehensive, equitable, and patient-centred cancer care.
- Enhanced early detection and comprehensive data management
The integration of the upgrade of health and wellness centres for cancer screening of common types such as breast, cervical, and oral cancer with making cancer a notifiable disease would enhance data accuracy and tracking, enabling targeted interventions and policy decisions. Enhancing rural population-based cancer registries and employing advanced technologies for efficient data management would further streamline care across various facilities. This approach aligns with the government’s initiatives, such as PMJAY, which offers coverage for secondary and tertiary care hospitalisation up to INR 5 lakhs per family per year.
- Infrastructure development and optimised resource allocation
The government’s focus on the expansion of healthcare infrastructure and financial protection, as seen in initiatives like the Health Minister’s Cancer Patient Fund and the Health Minister’s Discretionary Grants, provides financial assistance for cancer treatment, especially for those living below the poverty line. Enhancing initiatives like NCG through pooled procurement strategies for infrastructure and equipment, along with providing comprehensive training for healthcare workers, can maximise the utilisation of resources. The replication and integration of successful initiatives like Tata Memorial Centre’s (TMC) hub-and-spoke model in public healthcare systems, with a focus on telemedicine, aligns with the government’s objective to provide equitable healthcare access across India.
- Sustainable financing and community engagement
Innovative financing mechanisms, such as incorporating corporate social responsibility (CSR) funds into cancer care, can provide support to government initiatives like the Prime Minister’s National Relief Fund and the State Illness Assistance Fund, which offer coverage for cancer treatment. These funds should complement government efforts. Community engagement initiatives are pivotal in societal change and can augment government-led awareness campaigns, thus addressing social stigma and encouraging early screening. The Indian Council of Medical Research (ICMR) project to accelerate cancer screening at the district level, involving non-specialist physicians and other healthcare workers within a supportive system, exemplifies the importance of community involvement. This initiative, which aims to improve coverage and quality of cancer screening, also highlights the role of local communities and frontline health workers in promoting and conducting home-based cancer screening.
This report is based on a lecture given by the author at the Tata Medical Centre, Kolkata, on 18 November 2023.
Endnotes
[1] Government of India. "National Sample Survey 75th Round - Social Consumption in India: Health." Ministry of Statistics and Programme Implementation, (July 2017 -June 2018), New Delhi. Accessed at https://www.mospi.gov.in/unit-level-data-report-nss-75th-round-july-2017-june-2018-schedule-250social-consumption-health
[2] Government of India. " National Sample Survey 75th Round - Social Consumption in India: Health."
[3] Government of India. " National Sample Survey 75th Round - Social Consumption in India: Health."
[4] Government of India. " National Sample Survey 75th Round - Social Consumption in India: Health."
[5] Prinja, Shankar, Jyoti Dixit, Nidhi Gupta, Anushikha Dhankhar, Amal Chandra Kataki, Partha Sarathi Roy, Nikita Mehra et al. "Financial toxicity of cancer treatment in India: towards closing the cancer care gap." Frontiers in Public Health 11 (2023): 1065737.
[6] Goyanka, Roopali, Jeetendra Yadav, and Palak Sharma. "Financial burden and coping strategies for cancer care in India." Clinical Epidemiology and Global Health 20 (2023): 101259.
[7] Government of India, “National Sample Survey 75th Round - Social Consumption in India: Health”
[8] Government of India. “National Sample Survey 75th Round - Social Consumption in India: Health”
[9] Government of India. “National Sample Survey 75th Round - Social Consumption in India: Health”
[10] Government of India. “National Sample Survey 75th Round - Social Consumption in India: Health”
[11] Behera, Sasmita, and Jalandhar Pradhan. "Economic burden of cancer treatment in India: an equity perspective." Journal of Social and Economic Development (2023): 1-16.
[12] Banerjee, Dwaipayan. "Cancer and secrecy in contemporary India." BioSocieties 14, no. 4 (2019): 496-511.
[13] Kurian, Oommen C., and Shoba Suri. Weighed down by the gains: India’s twin double burdens of malnutrition and disease. Occasional Paper Vol. 193. Observer Research Foundation, 2019.
[14] Dhankhar, Anushikha, Ranjeeta Kumari, and Yogesh A. Bahurupi. "Out-of-pocket, catastrophic health expenditure and distress financing on non-communicable diseases in India: A systematic review with meta-analysis." Asian Pacific Journal of Cancer Prevention: APJCP 22, no. 3 (2021): 671.
[15] Katdare, Ninad. "Obstacles and Optimisation of Oncology Services in India." In Improving Oncology Worldwide: Education, Clinical Research and Global Cancer Care (2022), . 107-115. .
[16] Ahuja, Maninder. "Burden of cancers in India: Stumbling blocks and vision of success." Journal of Mid-life Health 13, no. 3 (2022): 195.
[17] Pramesh, C. S., Harit Chaturvedi, Vijay Anand Reddy, Tapan Saikia, Sushmita Ghoshal, Mrinalini Pandit, K. Govind Babu et al. "“Choosing Wisely” for cancer care in India." Indian Journal of Medical and Paediatric Oncology 41, no. 04 (2020): 567-569.
[18] Yadav, Amit, Prashant Kumar Singh, Nisha Yadav, Ravi Kaushik, Kumar Chandan, Anshika Chandra, Shalini Singh et al. "Smokeless tobacco control in India: policy review and lessons for high-burden countries." BMJ global health 5, no. 7 (2020): e002367.
[19] Gadiraju, Padmaja, Punam Singh, C. Vanlalhruaii, and Ranjit Kumar Dehury. "Challenges and Issues in the Treatment of Reproductive Cancer in India: A Behavioural Science Perspective." Journal of Clinical & Diagnostic Research 16, no. 4 (2022).
[20] World Economic Forum. 'The Breakthrough Technologies Transforming India's Cancer Care.' World Economic Forum, November 2022. https://www.weforum.org/agenda/2022/11/the-breakthrough-technologies-transforming-india-s-cancer-care/
[21] Epton, Tracy, Mahati Chittem, Ravali Tanikella, Senthil Rajappa, Sudha Sinha, and Peter R. Harris. "Indian patient use of cancer euphemisms: Association with psychological outcomes and health behaviours." Psycho‐Oncology 29, no. 7 (2020): 1193-1200.
[22] Kaul, Pallvi, Rahul Kumar, Mahendra Pal Singh, and Pankaj Kumar Garg. "Social taboos: a formidable challenge in cancer care." BMJ Case Reports CP 14, no. 1 (2021): e236095.
[23] Agarwal, Arunika, Alyssa Lubet, Elizabeth Mitgang, Sanjay Mohanty, and David E. Bloom. Population aging in India: Facts, issues, and options. Springer Singapore, 2020.
[24] Ahuja, Maninder. "Burden of cancers in India: Stumbling blocks and vision of success."
[25] Pramesh, C. S., Rajendra A. Badwe, Bibhuti B. Borthakur, Madhu Chandra, Elluswami Hemanth Raj, T. Kannan, Ashok Kalwar et al. "Delivery of affordable and equitable cancer care in India." The Lancet Oncology 15, no. 6 (2014): e223-e233.
[26] Smith, Robert D., and Mohandas K. Mallath. "History of the growing burden of cancer in India: from antiquity to the 21st century." Journal of global oncology 5 (2019): 1-15.
[27] Pramesh, C. S., Rajendra A. Badwe, Nirmala Bhoo-Pathy, Christopher M. Booth, Girish Chinnaswamy, Anna J. Dare, Victor Piana de Andrade et al. "Priorities for cancer research in low-and middle-income countries: a global perspective." Nature medicine 28, no. 4 (2022): 649-657.
[28] Cortes, Javier, Jose Manuel Perez‐García, Antonio Llombart‐Cussac, Giuseppe Curigliano, Nagi S. El Saghir, Fatima Cardoso, Carlos H. Barrios et al. "Enhancing global access to cancer medicines." CA: a cancer journal for clinicians 70, no. 2 (2020): 105-124.
[29] Horgan, Denis, Rizwana Mia, Tosan Erhabor, Yosr Hamdi, Collet Dandara, Jonathan A. Lal, Joel Fokom Domgue et al. "Fighting Cancer around the World: A Framework for Action." In Healthcare, vol. 10, no. 11, p. 2125. MDPI, 2022.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

 PDF Download
PDF Download


 PREV
PREV


