-
CENTRES
Progammes & Centres
Location
 PDF Download
PDF Download 
Abstract
India has made it clear that its development goals will be in alignment with the Sustainable Development Goals (SDGs), as NITI Aayog prepares the vision document for the country’s development for the 15 years beyond the Twelfth Five-Year Plan. The global success of SDGs over the next 15 years will depend, to a large extent, on India’s performance. However, India is faced with formidable challenges not only in implementing its national health and nutrition goals, but also in tracking its progress towards those targets. In July 2016 the Observer Research Foundation organised a panel discussion on the subject, titled, “Better Data for Better Health: Developing an Indian Approach on Indicators to Achieve SDGs”. This Special Report draws policy lessons built around the key themes shared during the event. A longer paper is in progress.
In early 2016, around 200 countries agreed in principle on a global indicator framework as a starting point for the 2030 Agenda and the Sustainable Development Goals (SDG). The 17 goals and 169 targets of the SDG framework are complemented by 230 indicators, representing a five-fold increase from the 48 indicators of the Millennium Development Goals (MDG).
As India joins the global community in the pursuit of the SDGs, it faces the twin burden of implementation and official data capture. Since the 1970s, various studies of India’s health sector have shown that a third of field workers’ valuable time is often eaten up by the task of maintaining registers and records. Over the years, these trade-offs have had a negative impact on the quality of data captured by the health system.
This systemic weakness has been acknowledged by a succession of Indian governments. The National Health Policy of 2002 recognised the dire need for systematic and scientific population health statistics. Initial assessments have identified several key issues such as lack of information on non-communicable diseases and injuries, dearth of primary data on causes of death, lack of private health sector numbers, and insufficient district-level data.
Another issue is the policy relevance of the numbers that are produced. Current data on health workers, for example, are inadequate: while information is available on those employed in public health facilities, there is insufficient data on the large numbers in private practice. Professional registries are of limited use, as they do not reflect retirement, death or migration of health professionals. In this context, the Census remains a highly useful but underutilised resource. In 2016, the World Health Organization published the first definitive report on state-level health workforce in India. As it is based on Census 2001 data, however, it has lost its policy relevance, other than to function as a useful baseline. There are no known plans so far to analyse the 2011 Census data.

The MDG framework of vertical goals has contributed to a fragmented approach. This time, the SDG framework attempts to overcome this anomaly with a broader set of goals. To understand the huge regional, inter- and intra-state disparities and remedy them, large amounts of new information will be required. Given existing constraints within the system, a ‘data revolution’ is needed in terms of making disaggregated data publicly available, if India is to achieve—or get anywhere near—the ambitious SDG targets related to health and nutrition. The following are specific recommendations to streamline and build on the existing national statistical infrastructure to facilitate such a revolution.
1. Transform Civil Registration and Vital Statistics (CRVS) systems
The World Health Organization (2015) has observed that unlike other data sources such as censuses and household surveys, the Civil Registration and Vital Statistics (CRVS) systems permit continuous production of statistics even for local administrative subdivisions. It therefore provides more accurate information, and in turn, clearer ‘denominators’ for assessing progress across sectors.
India relies on sample registration and surveys to track mortality-related goals because of the inadequate coverage of its Civil Registration System (CRS). The National Population Policy 2000 had set the goal of achieving universal birth registration by the year 2010. While the country has made considerable improvement, the nationwide coverage is inadequate for informing decision-making. There are 28 States/UTs where the coverage of birth registration is more than 90 percent and 17 States/UTs where the coverage of death registration is more than 90 percent, according to official estimates (See Figure 1).
Figure 1: Coverage of Birth and Death Registration in India (2013)
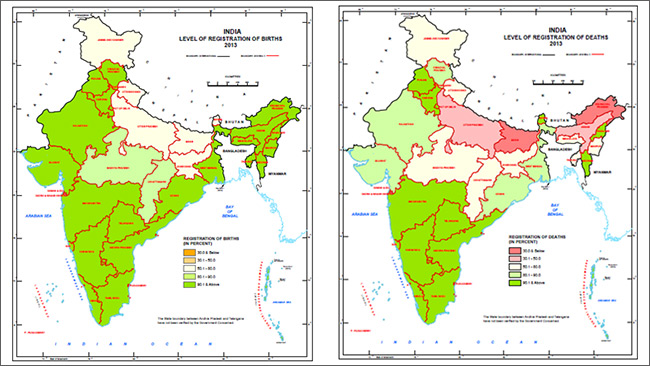
Only eight States/UTs have achieved the target of 90 percent in both birth and death registration, with 17 having reached 100-percent birth registration and 11, 100-percent death registration. Overall, birth and death registrations in India stood at 85.5 percent and 70.7 percent, respectively, in 2013. Inter-state differences are sharp: For example, if Bihar and Uttar Pradesh are excluded from the analysis, the national coverage of registration of births is at 96.8 percent and that of deaths, 85.2 percent.
The proportion of female birth registration is 47 percent and death registration, just 42 percent. Barring certain states, there is no evidence of selective under-registration of female births in CRS. Still, more research is necessary in the case of mortality—after all, the proportion of infant deaths registered in rural areas is a low 33.1 percent. A reason could be that deaths are registered at the place of death rather than at the place of residence. There is strong evidence of poor registration of infant deaths; 22.48 million births were registered in 2013 and the registered number of infant deaths was 188 thousand (187,689)—or less than nine infant deaths per 1000 births, which is quite low given India’s IMR, which is 40 according to SRS 2013. Research should be conducted to find the extent to which gender or regional variance represent a relatively low probability of registration for women or those from rural areas.
NFHS rounds have reiterated rural-urban differences in birth registration, while gender-based differences are not seen across the country, barring exceptions like Rajasthan. Studies show that inequities based on income are a major constraint in achieving universal registration. Further, there is a need to standardise actual registration processes to facilitate cross-coordination. As things are, registration is done by officials from different state departments—ranging from police to health, to revenue.
In 2014, India announced a “Vision 2020” plan, aiming to achieve universal registration of births and deaths by the year 2020. Given current trends in the low-performing states, this goal appears farfetched. However, the initiative to integrate the National Population Register (NPR) – which is set to be completed in December 2016 – with CRS offers transformative possibilities. Efforts to universalise birth and death registration, as well as integrate existing databases like the Census, NPR and CRS systems at the sub-district levels, can help track at-risk population in small areas.
2. Streamline existing national surveys
The latest round of the National Family Health Survey (NFHS 2015-16), for the first time in its history, gives district-level estimates. NFHS will now repeat every three years, and will no doubt help overcome some of the country’s health and nutrition data bottlenecks. NFHS 4 replaces the Annual Health Survey (AHS) and District Level Household and Facility Survey (DLHS) – two major sources of health data at the district level during the MDG era. However, with AHS and DLHS gone—and the National Nutrition Monitoring Bureau (NNMB), a major source of dietary intake and nutritional status shut down in 2015—there is a need to take concrete steps towards health and nutrition monitoring.
The National Sample Survey (NSS) ‘central sample’ data, which is widely used by policy researchers still does not give reliable district-level estimates for many indicators. However, considerable resources are also spent by the government to collect the currently unused ‘state sample’, which covers a matching number of respondents in each state. Pooling of central and state samples will enhance the policy relevance of NSS data, as the data can then be used to arrive at district-level estimates.
It thus becomes a policy imperative to conduct a comprehensive assessment of existing surveys with the aim of streamlining a set of health and nutrition indicators to continuously track the national targets. Some questions can be added—e.g., on location of treatment, parliamentary constituency, Food Insecurity Experience Scale (FIES)—which can expand possibilities of analysis. Further, some modules can be dropped after an assessment (e.g., PNC module in NSS health rounds), and questions can be standardised across different surveys (e.g., question on insurance coverage in NFHS and NSS). Overall surveys can also be strengthened, keeping in mind India’s double burden of communicable and non-communicable diseases.
There is a need to combine the consumer expenditure rounds with at least some modules of the social consumption of health rounds so that enhanced data is collected at more regular intervals. Robust policy documents raising precise questions are required, and data will need to be collected based on these, avoiding duplication and redundancy. A yearly survey covering all major indicators of health and nutrition coordinated by NSSO should be considered after mapping all the available surveys to assess adequacy of data. Pratham’s Annual Status of Education Report (ASER) can offer inputs towards such an endeavour.
3. Reform the national Health Management Information System (HMIS)
An efficient national health information system facilitates transparent and evidence-based decision-making, which in turn leads to improvements in health outcomes. Higher investments in HMIS offer various benefits, including: helping decision-makers to detect and control emerging and endemic health problems, monitor progress towards health goals, and promote equity.

India’s HMIS was intended as a management information system to oversee the working of the National Rural Health Mission (NRHM), now renamed the National Health Mission (NHM). NHM has around 1.8 lakh health facilities capturing data for HMIS about antenatal coverage, immunisation coverage, delivery services, family planning coverage, among other indicators, across the country.
The lack of coverage of the private medical facilities affects the usefulness of HMIS data. Other factors affecting quality are severe staff shortages and the nature of incentive structures within the system. HMIS covers only 12.7 percent of the annual estimated infant deaths and 24.8 percent of the annual estimated maternal deaths (Annual Report 2014-15). At the same time, due to under-reporting of births and reporting of immunisation on the same child by more than one facility, the percentage of fully immunised children in India is wrongly shown to be consistently above 100 percent. For it to inform evidence-based decision-making, India’s HMIS will have to be improved tremendously.
Multiple initiatives often prevent a holistic health systems approach. Various schemes and programmes announced by the ministries of health and of women and child development, should be mapped and rationalised in a way that there is a comprehensive set of indicators helping assess the system and track progress. The large, government-funded health insurance schemes can be used as a means to hasten the progress in regulation of private medical institutions and to ensure a regular flow of information from the private sector—this is a blind spot at present. An interesting model is offered by the District Information System for Education (DISE), which provides annual, self-reported data by every school in India.
4. Set Up a national Forum on Health and Nutrition Statistics
While several government departments and ministries collect data across institutions and other stakeholders, these are not often comparable, and there are instances of duplication. This calls for systematic efforts to address fragmentation at the national level, taking state governments and departments onboard.

An institutional mechanism to coordinate efforts at the national level (a Forum on Health and Nutrition Statistics), based loosely on the Forum on Child and Family Statistics of the US, should be considered. This mechanism will comprise Central government agencies and ministries which currently collect, store, analyse and distribute different sets of health and nutrition data. Its mission should be to foster coordination and collaboration and to enhance consistency in the collection and reporting of health and nutrition data. To start with, the Ministry of Home Affairs (Office of the Census Commissioner and Registrar General), Ministry of Statistics and Programme Implementation, Ministry of Health and Family Welfare (NFHS, HMIS, IHIP,MCTS, HIE), Ministry of Women and Child Development (ICT-RTM, ICDS-CAS) and the NITI Aayog should be involved, along with state-level functionaries.
Moreover, the Forum should standardise definitions, streamline collection of data, and avoid duplication in order to bring out a comprehensive set of indicators every year which will track health and nutrition progress across the country at the sub-district level, across different attributes. The Forum can take up initiatives such as pooling of NSS central and state samples so that currently under-utilised NSS datasets are of use to policymakers, academics, researchers and frontline workers. An immediate objective of the Forum should be to conduct a comprehensive study on the health workforce in India analysing the 2011 Census data, to inform policies on medical education based on decadal trends.
If gaps still remain in terms of data elements needed to track national health and nutrition targets at the district level, the Forum should facilitate, as an interim measure, an annual technology-driven survey providing panel data across parliamentary constituencies/districts that are particularly underperforming.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Oommen C. Kurian is Senior Fellow and Head of Health Initiative at ORF. He studies Indias health sector reforms within the broad context of the ...
Read More +