-
CENTRES
Progammes & Centres
Location
 PDF Download
PDF Download 
Sheila C Vir and Shoba Suri, “The Role of Maternal Nutrition in Reducing Childhood Stunting,” ORF Occasional Paper No. 355, May 2022, Observer Research Foundation.
Image Source: The Role of Maternal Nutrition in Reducing Childhood Stunting
Introduction
Maternal malnutrition is a serious public health concern in many parts of the world, including India. A woman’s health and nutrition before, during, and after pregnancy influences her child’s early growth and development.[1] Maternal undernutrition contributes to maternal mortality, foetal growth restriction, and neonatal death; it sets up a life cycle of undernutrition for the child.[2] In India, maternal undernutrition is estimated to account for one-fifth of all incidence of childhood stunting.[3] In turn, child undernutrition contributes to a massive 68 percent of under-five child deaths. During this period, poor nutrition adversely impacts the brain’s sensory, language, and cognitive functions. This carries long-term consequences, including diminished learning capacity and poor school performance in childhood, and in adulthood, reduced earnings and increased risks of chronic diseases such as diabetes, hypertension, and obesity.[4]
A regression analysis of the determinants of childhood stunting in three countries in Asia, including India, has found five important contributory risk factors: maternal height, lack of maternal education, poor healthcare, low standard of living, and lack of access to a clean toilet.[5] These observations are supported by studies in the last decade that have found an association between maternal anthropometry (height, weight or thinness) and the infant’s birth weight.[6] Maternal stunting (defined as having a height less than 145 cm) increases the risk of both term and preterm ‘small for gestational age’ (SGA) babies. A pooled analysis of 7,630 mother–child pairs from birth cohorts of five countries[a] reveals that maternal height is associated with birth weight, and with linear growth of children over the growing period.[7] An analysis of national demographic survey findings from India reveals a significant decrease in the relative risk of stunting in children for every 5-cm increase in maternal height from 160 cm.[8]
Evidence also indicates a strong association in improvement in the woman’s Body Mass Index (BMI) with reduced incidence of low birth weight (LBW) babies (see Figure 1).
Figure 1. Improvement in Women’s Body Mass Index (BMI) Reduces LBW (1980s-2000s)
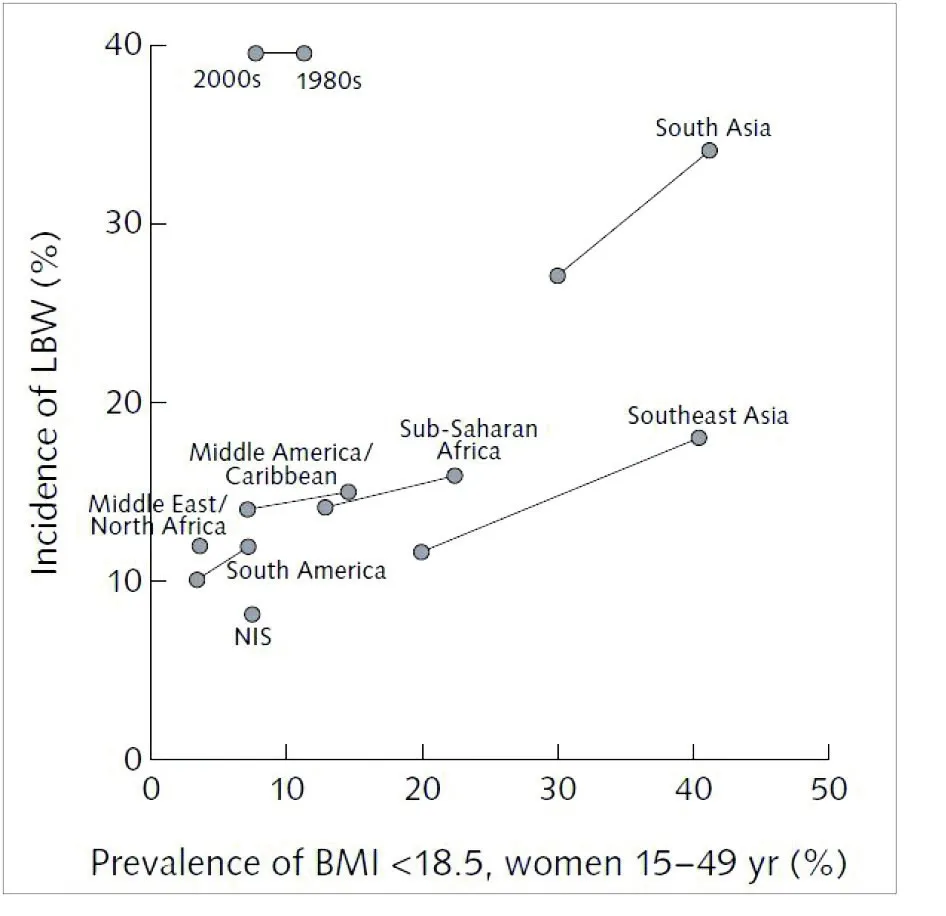
Source: Mason et al 2012[9]
LBW is associated with 2.5- to 3.5-fold higher odds of wasting, stunting, and underweight in children.[10],[11] Stunting that occurs in the first 24 months of life is largely irreversible, and contributes to an intergenerational cycle of poor growth and development: Girls who are stunted in childhood remain stunted as adults, and then have a higher chance of giving birth to stunted offspring.[12],[13]
A trend analysis of data from the 1998-99 National Family Health Survey-2 (NFHS 2) to the 2019-21 NFHS-5, shows an association between a reduction in the percentage of underweight women (i.e., defined as having BMI less than 18.5) and lower percentages of LBW and childhood stunting (see Figure 2).[14] Women who are overweight or obese (i.e., with BMI greater than 25) are found to be at increased risk of preterm births.[15] The child then grows up becoming more susceptible to a host of physical, cognitive, and social-development challenges.[16]
Figure 2: Trends in the percentage of women with low BMI (<18.5), LBW, and Childhood stunting, 1998-2021: NFHS 2 (1998-99), NFHS 3 (2005-6), NFHS 4 (2015-16), and NFHS 4 (2019-21)
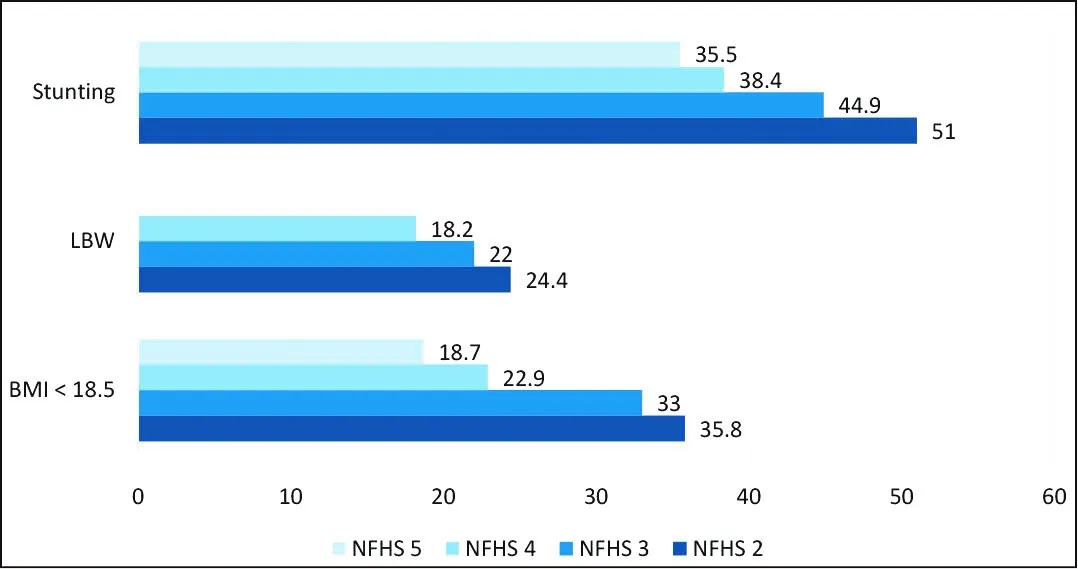
As seen in Figure 2, child undernutrition—measured as childhood stunting—has declined rather slowly, from 51 percent in 1998-99 to 35.5 percent in 2019-21.[17] This is possibly due to inadequate progress in implementing appropriate measures for improving maternal nutrition.
Maternal Malnutrition in India: Overview
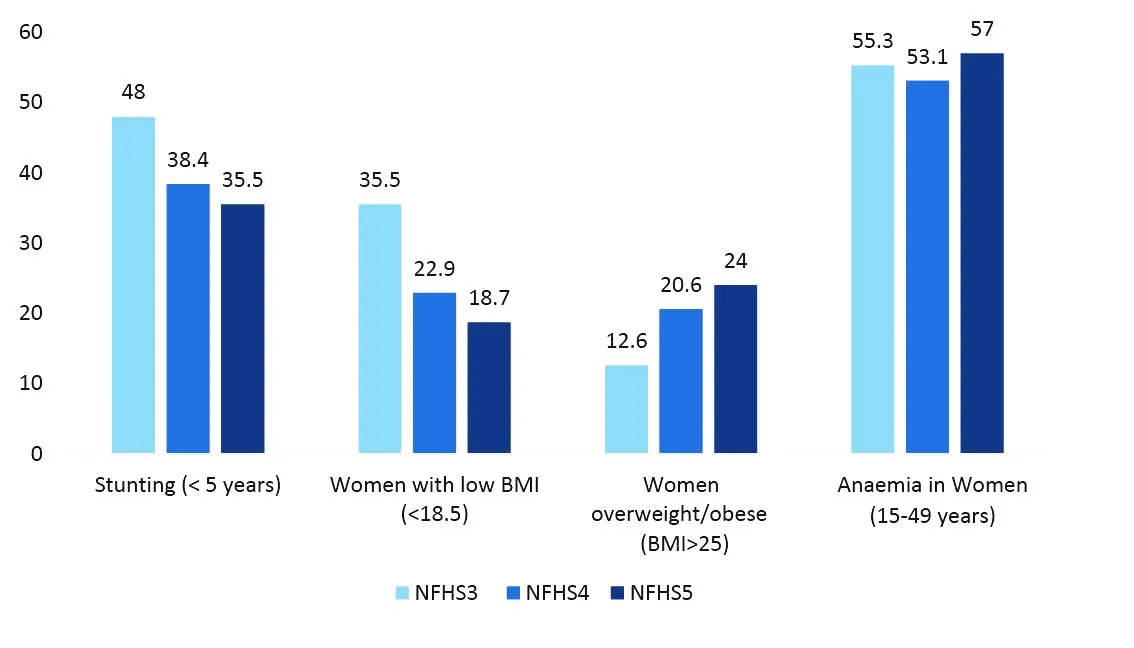
Malnutrition—in this paper, defined as comprising undernutrition, overweight, and anaemia[b]—adversely impacts pregnancy outcomes. National health surveys in India over the past two decades have found undernutrition in adult women to have declined from 35.5 percent in 2008-09 to 18.7 percent in 2019-21 (see Figure 3). Over the same period, overweight/obesity doubled, and the prevalence rate of anaemia hovered between 55.3 and 57 percent.
Figure 3: Trends in childhood stunting and Women’s nutritional status
There is wide variation in both undernutrition and overweight/obesity in women across India’s states and UTs (see Figure 4). In all except two states, there has been a decrease in the percentage of undernourished women, and an increase in overweight/obesity. Except for five states, all other states recorded an increase in the proportion of overweight/obese among adult women. In eight states, over one-third of adult women are found to be overweight/obese. Women who are overweight prior to the onset of pregnancy face additional risks during pregnancy, such as gestational diabetes, hypertension, preeclampsia, and non-natural delivery, as well as poor pregnancy and breastfeeding outcomes.[18]
The increase in overweight rates in women in India can be attributed to various factors such as changing food habits and decreased energy expenditure because of sedentary habits. Low-cost, attractively packaged unhealthy processed foods have also become more easily available—having high content of fat and sugar, these foods increase the likelihood of excess energy intake against the energy required for daily chores or mobility.
Figure 4: Prevalence rate of undernutrition and overweight/obesity in women 15-49 years, in various states/UTs of India (2019-21)

Besides the twin problems of undernutrition and overweight, micronutrient deficiencies are prevalent in women of reproductive age. Little data is available on the extent of micronutrient deficiencies in women or in pregnant women; most reliable is the data on anaemia and dietary intake from the decadal National Nutrition Monitoring Bureau (NNMB) Survey (see Table 1). NNMB surveys indicate that many women have poor diets, and they are deficient in key micronutrients (e.g., iron, folate, vitamin B12), irrespective of whether they have normal, low, or high BMI.
According to NFHS 5, anaemia, primarily due to iron and folic acid deficiencies, affects 57 percent of all adult women in India. Iron-deficiency anaemia in pre-pregnancy or early pregnancy puts the mother at increased risk of significant decrements in foetal growth, as well as preterm birth or LBW delivery.[19],[20] The prevalence of anaemia in adolescent girls (15-19 years) is also a cause for alarm: it increased from 54.1 percent in 2015-16 to 59.1 percent in 2019-21.
Table 1: Consumption of Recommended Dietary Allowance (RDA) of various nutrients
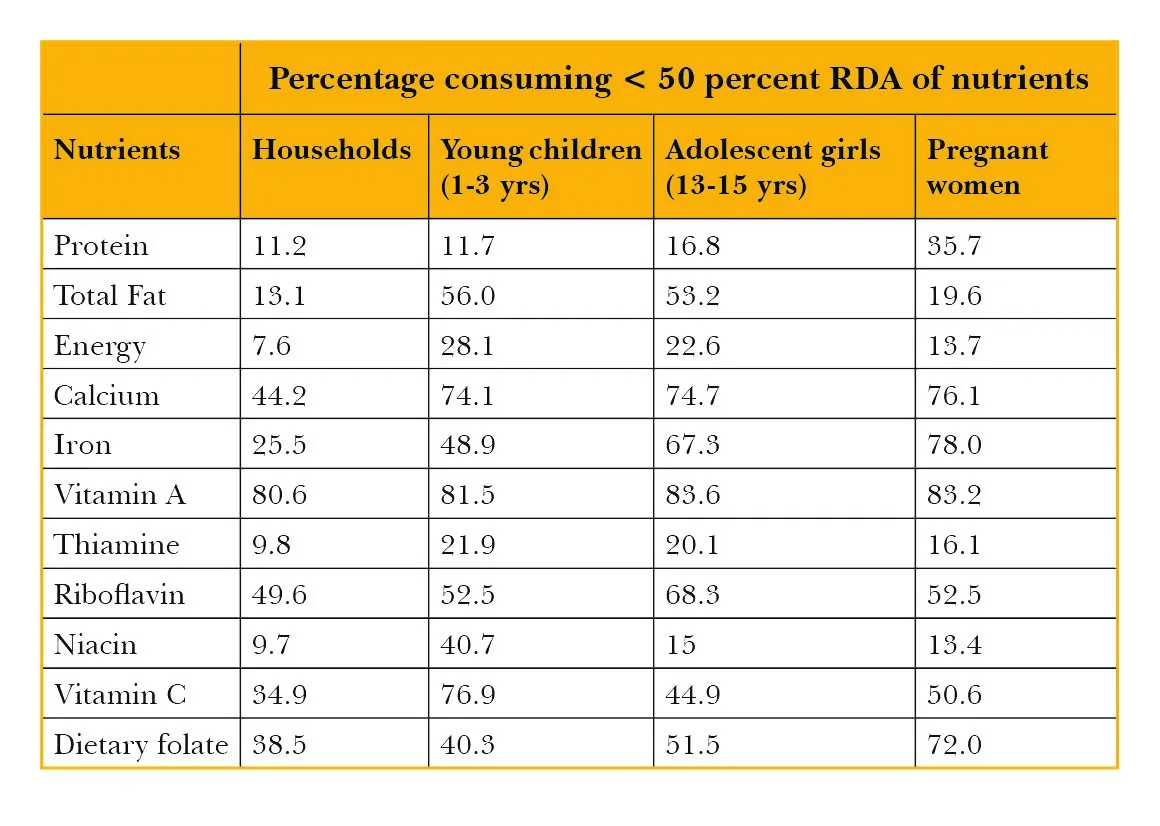
Source: NNMB Survey report, 2012[21]
Improving Maternal Nutrition: Nutrition-Specific and Nutrition-Sensitive Interventions
Health experts agree that malnutrition in women has roots in many factors, at the individual, household, community, and societal levels.[22] Figure 7 illustrates the implications of women’s resource constraints on child undernutrition. The resource constraints include both, nutrition-specific drivers of mother’s nutrition and physical well-being, as well as nutrition-sensitive factors such as women’s empowerment that impact decision-making power and control over household resources, education and knowledge, employment, and time availability.[23]
Figure 5: Women’s resources, Nutrition-specific and Nutrition-sensitive factors, and Childhood stunting
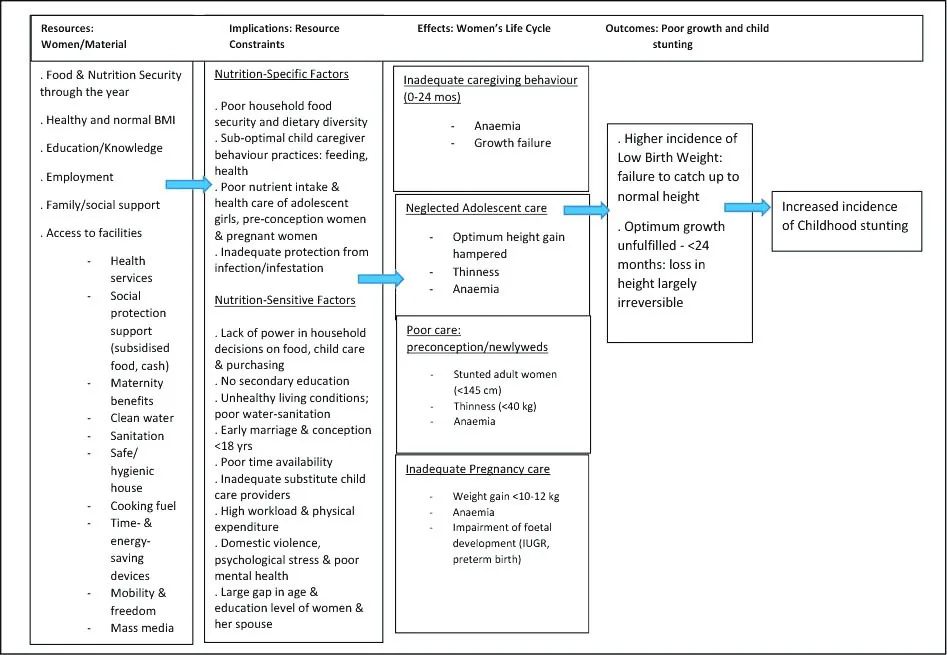
Source: Sheila C. Vir, 2016[24]
A review study indicates that the three domains of women’s empowerment—i.e., control of resources and autonomy, workload and time, and social support environment—influence child anthropometry. However, the strength and direction of association differs according to various factors such as child’s age and household income.[25]
As shown in Figure 5, the immediate and direct causative factors of poor maternal nutrition are poor dietary intake during pregnancy, and inadequate health services. Women must maintain a healthy weight prior to the onset of pregnancy, as both excess and low weight gain during pregnancy could lead to adverse pregnancy outcomes.[26] To meet the observed nutrient intake gap and the rapid increase in nutrient requirements during pregnancy, the ICDS sector provides pregnant women supplementary nutrition (SN),[c] and the health sector administers micronutrient supplements (IFA and calcium), all as part of national policy. In most states, SN is supplied as dry food mixture in the form of Take Home Ration (THR); in others, SN is given as a hot cooked meal instead of THR. According to latest available data (2013-14), only four of every 10 pregnant women (40.7 percent) availed the SN service of ICDS, while an even lower 27.8 percent of all ICDS-enrolled pregnant women received SN for the minimum prescribed 21 days in a month.[27] Meanwhile, the proportion of pregnant women who daily consumed IFA tablets for 180 days was reported to be as low as 26 percent.[28]
Besides poor SN intake and consumption of IFA supplements, many pregnant women’s daily food intake lacks diversity. Analysts attribute this to inadequate purchasing power; at the same time, many women are unable to buy appropriately nutritious food with the meagre resources that they have, largely because of lack of awareness. Indeed, the imperative for behaviour change in food habits is widely recognised, and it was for this reason that nutrition education was made a component of ICDS. However, national surveys show that many women do not receive quality nutrition counselling services: for example, less than 18 percent of mothers of under-five children are aware that nutrition counselling is part of ICDS services.[29]
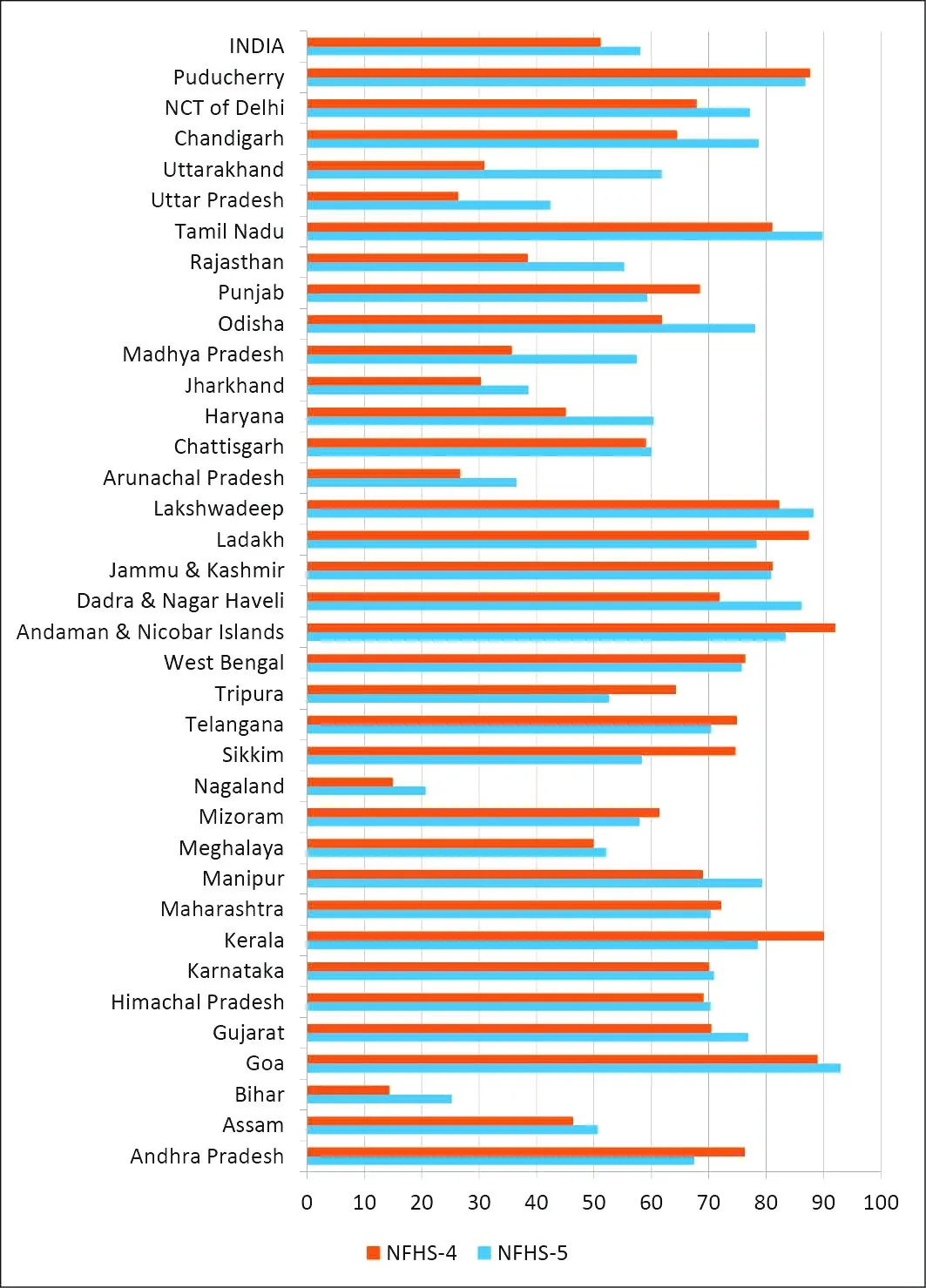
The other immediate factor that impacts maternal nutrition is timely access to health services. Appropriate antenatal care (ANC) services help reduce adverse health outcomes during pregnancy and childbirth.[30] According to NFHS-5, there has been a steady increase in the coverage of ANC services at the national level—from 51.2 percent in 2015-16 to 58 percent in 2019-21 (see Figure 6). Most states and UTs show an increase in the percentage of women availing the minimum recommended four ANC services, with Goa having the highest coverage at 93 percent; the states of Bihar, Manipur, Haryana, Madhya Pradesh, Odisha, Uttar Pradesh, and Uttarakhand are recording substantial improvement.[31]
Figure 6: Percentage of women attending 4 Antenatal Care (ANC) services: NFHS 4 (2015-16) and NFHS 5 (2019-21)
Data from the NFHS 5 (2019-21) shows notable improvement in many of the nutrition-sensitive factors illustrated in Figure 5, including proxy indicators of women empowerment (see Table 2 and Figure 7). The latter includes years of education, age of marriage, experience of domestic violence, and ownership of mobile phones and bank accounts.
Table 2. Coverage of nutrition-sensitive interventions in women 15-49 years: Comparison of percentage points (NFHS 4 and NFHS 5)
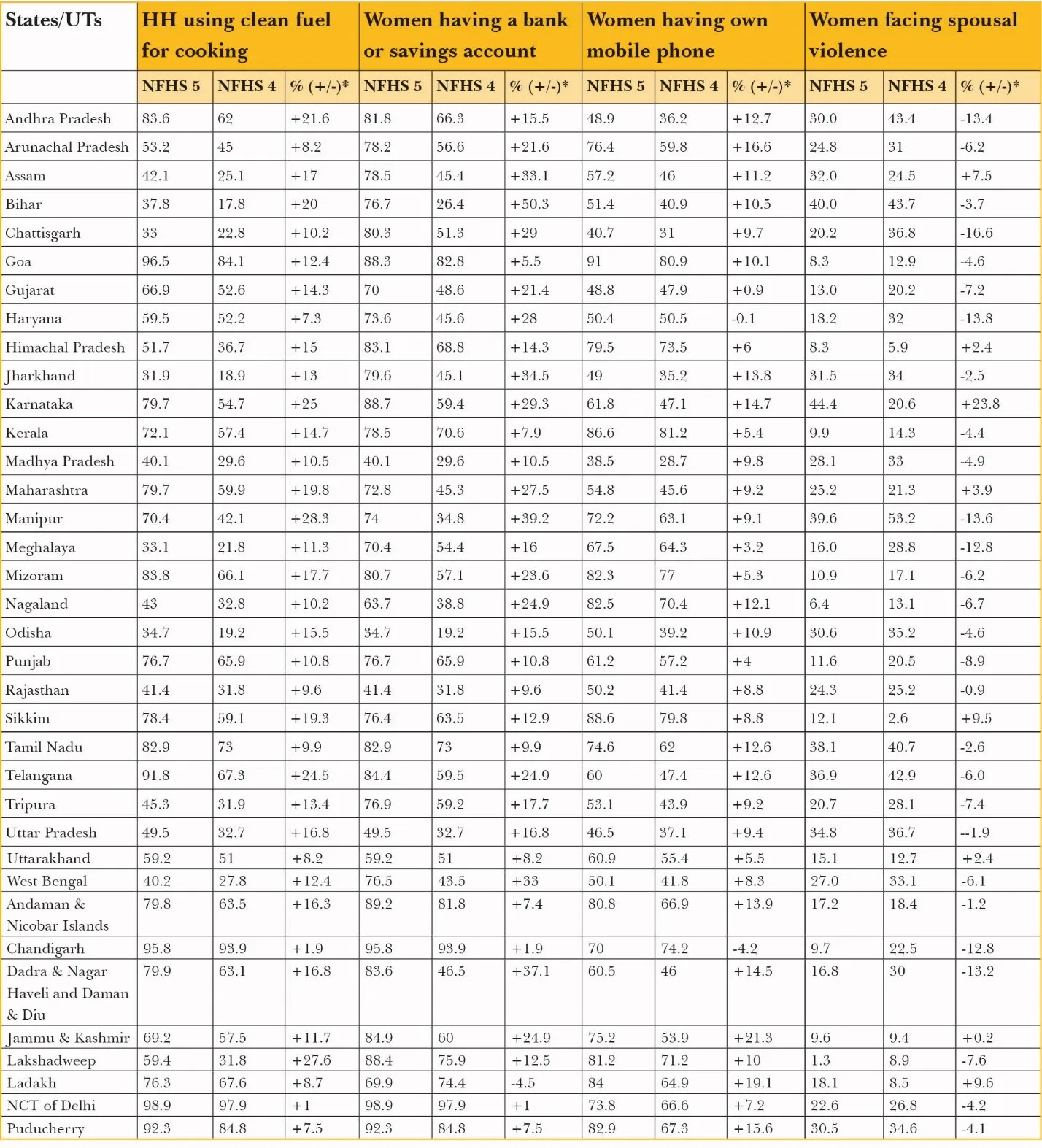
*represents the percentage point change
Latest data on the percentage of women completing 10 years of education is reported to be at 41 percent, up from 35.7 percent five years earlier in 2015-16, and 22.3 percent in 2005-06. Such attainment of education is found to have a positive impact on the nutrition status of these women’s children.[32] It is an experience that is not unique to India. Studies across different countries in South and Central Asia show similar patterns of reduction in childhood stunting, wasting, and underweight through the empowerment of mothers by enhancing their independence and giving them a voice in decision-making.[33] Greater agency, in turn, allows the woman to mobilise family support for food and care; it also addresses harmful cultural beliefs and practices about pregnancy (e.g., restrictive or excessive food intake) and gendered practices such as women being the last in the family to partake of a meal.
Women completing 10 years of education also has a positive impact on the age of marriage and conception (see Figure 7). In this regard, India has seen gains in the past decades in reducing the incidence of early marriage, especially among those under-18. This is expected to contribute in improving the state of child nutrition in the country; after all, early marriage and childbearing are among the most crucial causes of maternal undernutrition and have adverse consequences on health, education, and employment.[34]
Figure 7: Status of women in India: Percentage with secondary education, low age of marriage, and conception < 18 years
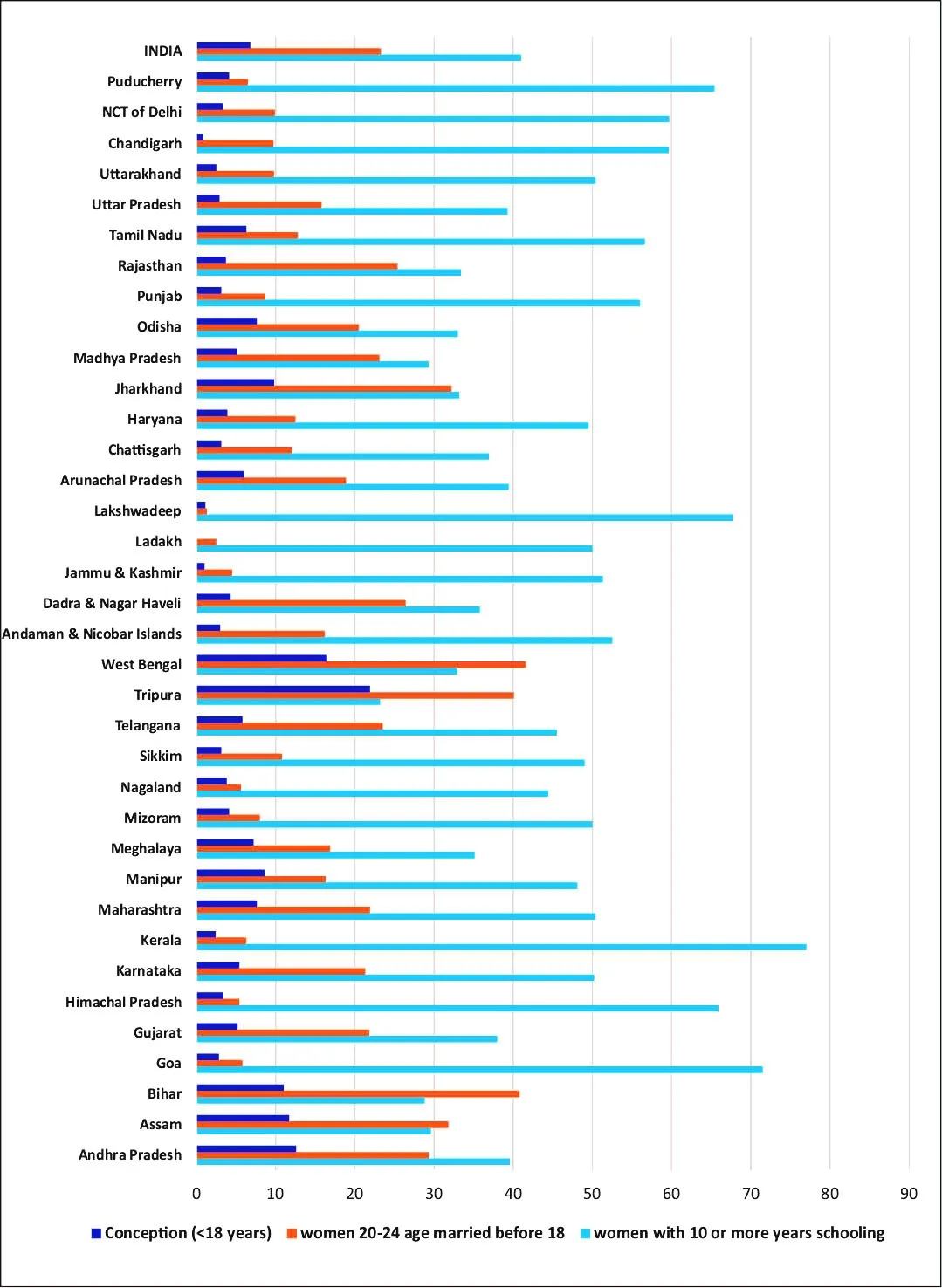
A 2016 analysis of social and biological factors of undernutrition in India found that children born to adolescent mothers have a 10-percent higher chance of being stunted.[35] Other countries share the same experience. Data gathered in 2015 from five low- and middle-income countries (LMICs), including India, showed a strong association between younger maternal age and lower birth weight, preterm birth, and stunting by 2 years of age.[36] Early pregnancy and conception prevents a woman from gaining optimum height. This then traps the woman in a likely cycle: Short stature (below 145 cm) is closely associated with poor pregnancy outcomes, such as SGA (small for gestational age) and preterm births, and stunting in children.[37]
Another important nutrition-sensitive determinant of maternal health is domestic violence. According to NFHS 5 data, 29.3 percent of adult women have experienced domestic violence at the time of the survey—this is lower than the 31.1 percent recorded by NFHS 4, and the 37.2 percent found by NFHS 3 (see Table 2). In India, such observed reduction in the incidence of domestic violence is partly correlated with completing higher levels of education.[38] This is remarkable progress. As indicated in Figure 5, domestic violence has immediate impacts on all aspects of women’s health—physical, sexual and reproductive, and mental. Domestic violence increases the risk of maternal mortality and pregnancy-related consequences such as stillbirths.[39]
Indeed, studies in different countries—i.e., Nicaragua, Bangladesh, India, and the United States—similarly report high incidence of low-birth-weight babies and deaths amongst pregnant women who experience domestic violence.[40] A 2020 study that focused on India also found an increased probability of stunting, underweight and wasting in children of mothers who experience violence from their intimate partner.[41]
The interrelated concerns of water, sanitation, and hygiene (WASH) are among the fundamental nutrition-sensitive factors that can influence maternal nutrition and, in turn, the likelihood of childhood stunting. Poor WASH practices can cause gastrointestinal conditions such as tropical enteropathy, which have adverse effects on growth. They also increase the occurrence of water-borne illnesses such as hookworm, and the risks of anaemia and low birth-weight. Findings of the NFHS 5 (2019-21) indicate a marked improvement in the country’s WASH situation: all states and UTs reported increased coverage of sanitation facilities, except in Sikkim, which had achieved 89.7-percent coverage in 2015-16 but declined to 87.3 percent in 2019-21. Water facilities were also recorded to have increased in all except four states and UTs (Sikkim, Punjab, Chandigarh and Delhi).[42] While these improvements in nutrition-sensitive measures are important, they have not been accompanied by parallel progress in the provision of more direct nutrition services for pregnant women. Programme interventions during pregnancy for promoting appropriate weight gain, consumption of diversified diet, and consumption of micronutrient supplements remain weak.
These gaps need to be bridged, given adequate evidence that paying attention to high coverage of evidence-based, nutrition-specific maternal nutrition interventions through integration with antenatal care services can have a significant impact on pregnancy outcomes. A 2019 study that gathered data from 81 LMICs reported that when evidence-based nutrition intervention packages were made available to mothers seeking antenatal healthcare, maternal and neonatal deaths declined by nearly one-third (28 percent), and stillbirths, by 25 percent.[43]
Some of India’s states have shown remarkable achievements in various nutrition-sensitive interventions. Odisha’s Mamata Scheme, for example, has led to a reduction in the percentage of stunting in children following programme interventions that focused on pregnant women improving attendance to ANC services, ensuring higher consumption of IFA tablets, and addressing the problem of household food insecurity.[44] In Maharashtra, meanwhile, childhood stunting has dropped from 39 percent in 2006 to 24 percent in 2012, owing to, among others, renewed focus on maternal, neonatal, and adolescent girls’ health. The state has also worked on creating an enabling environment for the reduction of childhood stunting.[45] This involves improving outcomes in mother’s literacy, delaying first pregnancy, number of antenatal visits, and promoting institutional delivery. There are also initiatives related to providing women with opportunities for income-generation, along with appropriate infant and young child feeding practices and improved sanitation.[46],[47]
These are only a few of the examples from specific states which prove that maternal nutrition is crucial to achieving rapid and significant progress in reducing childhood stunting. Attention needs to be directed at scaling up these evidence-based nutrition interventions for pregnant women. These include nutrition counselling, as well as monitoring for appropriate weight gain, improving supply and compliance of micronutrient supplements that are delivered as a part of ANC services, and consumption of supplementary nutrition from the ICDS system. These interventions need to be continued and supplemented by efforts to address the underlying socioeconomic causes that adversely influence nutrition in women and children.[48],[49]
Policymakers are giving more attention to the imperative of improving maternal nutrition, and the goals of improving women’s health before, during, and after pregnancy are today part of two of the country’s primary national programmes—the ICDS, and the National Health Mission. However, it must be ensured that the opportunity platforms offered by these two schemes are used to the optimum, and explicit guidelines on maternal nutrition care are issued by the government. This paper makes the following recommendations.
Conclusion
Malnutrition in women is a result of many interrelated factors, including poor diets, limited knowledge, poor access and use of health and hygiene services, and a weak enabling environment due to harmful social and cultural practices. These gaps need to be filled, as malnutrition before and during pregnancy is a fundamental contributory factor to low birth-weight, which in turn has long-term, adverse consequences on a child’s growth.
Both direct and indirect determinants of undernutrition or overweight, and micronutrient deficiencies in pregnant women need to be addressed through a life-cycle approach. Particular attention needs to be paid to the first 1,000 days of life, as well as in the accelerated growth period of adolescence, through to the pre-conception period. Optimum use of contact opportunities with mothers during health and ICDS services, and reaching out to the unreached women through NRLM contacts, deserve special attention.
It is also critical to reach pregnant women who are outside the government health system and who opt for private health facilities. They should be informed of their entitlements in government feeding schemes, counselling on nutrition care including diet diversity, and for consumption of weekly iron-folic acid tablets for improved health and productivity.
The formulation of an evidence-based national maternal nutrition policy that addresses both immediate and underlying determinants of undernutrition is imperative. This policy should clearly outline the roles and accountability assigned for scaling up maternal nutrition interventions to the two primary sectors—health and ICDS, and other critical existing platforms (water-sanitation, education, maternity protection benefits, and social protection).[65] Implementing a comprehensive maternal nutrition policy would help the country achieve the Sustainable Development Goal (SDG) of eliminating all forms of malnutrition.
Endnotes
[a] The countries are Brazil, Guatemala, India, the Philippines, and South Africa.
[c] SN provides one-third of daily requirements of energy, protein, and micronutrients.
[1] World Health Organization, Global nutrition targets 2025: Stunting policy brief. No. WHO/NMH/NHD/14.3. World Health Organization, 2014, https://www.who.int/nutrition/topics/globaltargets_stunting_policybrief.pdf
[2] Robert E. Black et al., “Maternal and child undernutrition and overweight in low-income and middle-income countries,” The Lancet 382, no. 9890 (2013): 427-451.
[4] UNICEF, Stop Stunting, https://www.unicef.org/india/what-we-do/stop-stunting
[5] Sheila C Vir and Shoba Suri, “The 5th National Family Health Survey of India: A Sub-National Analysis of Child Nutrition,” ORF Occasional Paper No. 315, May 2021, Observer Research Foundation
[6] Black et al., “Maternal and child undernutrition and overweight in low-income and middle-income countries.”
[7] Addo O. Yaw et al., “Maternal height and child growth patterns.” The Journal of Pediatrics 163, no. 2 (2013): 549-554.
[8] Subramanian S. V., et al., “Association of maternal height with child mortality, anthropometric failure, and anemia in India,” Jama 301, no. 16 (2009): 1691-1701.
[9] Mason John B. et al., “Opportunities for improving maternal nutrition and birth outcomes: synthesis of country experiences,” Food and Nutrition Bulletin 33, no. 2_suppl1 (2012): S104-S137.
[10] Christian Parul et al., “Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low-and middle-income countries,” International Journal of Epidemiology 42, no. 5 (2013): 1340-1355.
[11] Sachdev H.P.S., “Overcoming challenges to accelerate linear growth in Indian children,” India Health Beat vol 5, Number 2, June 2011 (Public Health Foundation of India (PHFI) and World Bank).
[12] Georgiadis Andreas et al., “Child undernutrition: opportunities beyond the first 1000 days,” The Lancet Public Health 2, no. 9 (2017): e399.
[13] Sheila C. Vir, “Improving women’s nutrition imperative for rapid reduction of childhood stunting in South Asia: coupling of nutrition specific interventions with nutrition sensitive measures essential,” Maternal & Child Nutrition 12 (2016): 72-90.
[14] FAO, IFAD, UNICEF, WFP and WHO (2021), The State of Food Security and Nutrition in the World 2021, Transforming food systems for food security, improved nutrition and affordable healthy diets for all. Rome, FAO.
[15] Sarah D. McDonald et al., “Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: systematic review and meta-analyses.” Bmj 341 (2010).
[17] National Family Health Survey. International Institute of Population Sciences. Ministry of Health & Family Welfare. Government of India. http://rchiips.org/nfhs/index.shtml
[18] United Nations Children’s Fund 2021.
[19] Ana C.M.G. Figueiredo et al., “Maternal anemia and low birth weight: a systematic review and meta-analysis,” Nutrients 10, no. 5 (2018): 601.
[20] Shweta Kumari et al.,”Maternal and severe anaemia in delivering women is associated with risk of preterm and low birth weight: A cross sectional study from Jharkhand, India,” One Health 8 (2019): 100098.
[21] National Nutrition Monitoring Bureau. “Diet and Nutritional Status of Rural Population, Prevalence of Hypertension & Diabetes among Adults and Infant & Young Child feeding Practices—Report of third Repeat Survey.” Report of Third Repeat Survey) (2012).https://www.nin.res.in/downloads/NNMB_Third_Repeat_Rural_Survey%20%20%20Technicl_Report_26%20(1).pdf
[22] United Nations Children’s Fund 2021.
[23] Patrice L. Engle et al., “Care and nutrition: concepts and measurement.” World Development 27, no. 8 (1999): 1309-1337.
[24] Sheila C. Vir, “Improving women’s nutrition imperative for rapid reduction of childhood stunting in South Asia: coupling of nutrition specific interventions with nutrition sensitive measures essential.”
[25] Kenda Cunningham et al., “Women’s empowerment and child nutritional status in S outh Asia: a synthesis of the literature,” Maternal & Child nutrition 11, no. 1 (2015): 1-19.
[26] Bhavadharini Balaji et al.,”Gestational weight gain and pregnancy outcomes in relation to body mass index in Asian Indian women,” Indian Journal of Endocrinology and Metabolism 21, no. 4 (2017): 588.
[28] National Family Health Survey-5, 2019-21. International Institute of Population Sciences. Ministry of Health & Family Welfare. Government of India. http://rchiips.org/nfhs/factsheet_NFHS-5.shtml
[29] Rapid survey on Children (RSOC) 2013-14.
[30] Felix A. Ogbo et al., “Enablers and barriers to the utilization of antenatal care services in India,” International Journal of Environmental Research and Public Health 16, no. 17 (2019): 3152.
[31] National Family Health Survey-5, 2019-21.
[32] Katsushi Imai et al., “Women’s empowerment and prevalence of stunted and underweight children in rural India,” World Development 62 (2014): 88-105.
[33] Katsushi Imai et al., “Women’s empowerment and prevalence of stunted and underweight children in rural India.”
[34] Phuong Hong Nguyen et al., “Social, biological, and programmatic factors linking adolescent pregnancy and early childhood undernutrition: a path analysis of India’s 2016 National Family and Health Survey,” The Lancet Child & Adolescent Health 3, no. 7 (2019): 463-473.
[35] Phuong Hong Nguyen et al., “Social, biological, and programmatic factors linking adolescent pregnancy and early childhood undernutrition: a path analysis of India’s 2016 National Family and Health Survey.”
[36] Caroline H.D. Fall et al., “Association between maternal age at childbirth and child and adult outcomes in the off spring: a prospective study in five low-income and middleincome countries (COHORTS collaboration),” The Lancet Global Health 3, no. 7 (2015), e366–e377.
[37] Naoko Kozuki et al., “Short maternal stature increases risk of small-for-gestational-age and preterm births in low-and middle-income countries: individual participant data meta-analysis and population attributable fraction.” The Journal of Nutrition 145, no. 11 (2015): 2542-2550.
[38] Abigail Weitzman, “Does increasing women’s education reduce their risk of intimate partner violence? Evidence from an education policy reform.” Criminology 56, no. 3 (2018): 574-607.
[39] Abigail Weitzman, “Does increasing women’s education reduce their risk of intimate partner violence? Evidence from an education policy reform.”
[40] Shoba Suri, “Case study on India-Impact of domestic violence on the nutritional status of children,” July 15 2021, https://www.orfonline.org/expert-speak/case-study-on-india-impact-of-domestic-violence-on-the-nutritional-status-of-children/
[41] Dinabandhu Mondal and Pintu Paul, “Association between intimate partner violence and child nutrition in India: Findings from recent National Family Health Survey,” Children and Youth Services Review 119 (2020): 105493.
[42] National Family Health Survey-5, 2019-21.
[44] Kalyani Raghunathan et al., “Can conditional cash transfers improve the uptake of nutrition interventions and household food security? Evidence from Odisha’s Mamata scheme.” PLoS One 12, no. 12 (2017): e0188952.
[45] Nicholas Nisbett et al., “Explaining the reduction in child undernutrition in the Indian state of Maharashtra between 2006 and 2012: An analysis of the policy processes,” Food Policy 70 (2017, 27-39.
[46] Haddad L, Nisbett, N.; Barnett, I. and Valli, E., Maharashtra’s Child Stunting Declines: What Is Driving Them? Findings of a Multidisciplinary Analysis, Brighton: IDS, 2014, https://www.growgreat.co.za/wp-content/uploads/2019/02/Maharashtras-Child-Stunting-Declines-Report.pdf
[47] Victor M. Aguayo et al., “Determinants of stunting and poor linear growth in children under 2 years of age in India: An in‐depth analysis of Maharashtra’s comprehensive nutrition survey,” Maternal & Child Nutrition 12 (2016): 121-140.
[48] Vir Sheila C., “Improving women’s nutrition imperative for rapid reduction of childhood stunting in South Asia: coupling of nutrition specific interventions with nutrition sensitive measures essential.”
[51] Melissa F. Young et al., “Understanding Implementation and Improving Nutrition Interventions: Barriers and Facilitators of Using Data Strategically to Inform the Implementation of Maternal Nutrition in Uttar Pradesh, India.” Current developments in nutrition 5, no. 6 (2021): nzab081.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8242137/
[52] World Health Organization 2016. WHO recommendations on antenatal care for a positive pregnancy experience, https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf
[54] Rebecca A. Heidkamp et al., “Mobilising evidence, data, and resources to achieve global maternal and child undernutrition targets and the Sustainable Development Goals: an agenda for action,” Lancet 397, no. 10282 (2021).
[55] Kushwaha KP., Jhuma Sankar, M. Jeeva Sankar, Arun Gupta, J. P. Dadhich, Y. P. Gupta, Girish C. Bhatt, Dilshad A. Ansari, and B. Sharma. “Effect of peer counselling by mother support groups on infant and young child feeding practices: the Lalitpur experience.”
[56] International Food Policy Research Institute, Strengthening Governance for Agriculture and Rural Development in South Asia, Development strategy and governance Division (DSGD), 2008.
[58] Nguyen PH et al., “Strengthening nutrition interventions in antenatal care services affects dietary intake, micronutrient intake, gestational weight gain, and breastfeeding in Uttar Pradesh, India: results of a cluster-randomized program evaluation.” J Nutr 2021;151(8):2282–95
[59] United Nations Children’s Fund. UNICEF Programming Guidance. Prevention of malnutrition in women before and during pregnancy and while breastfeeding. New York: UNICEF, 2021
[60] Rapid survey on Children (RSOC) 2013-14.
[64] A. Dulloo, The Ministry of Rural Development’s Contribution to NNM, Deen Dayal Antodaya Yojana. Ministry of Rural Development, Government of India 2018, http://icds-wcd.nic.in/nnm/Events/NationalWorkshop/MoRD_NW_20-03-2018.pdf
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Dr. Sheila C. Vir is Director Public Health Nutrition and Development Centre.
Read More +
Dr. Shoba Suri is a Senior Fellow with ORFs Health Initiative. Shoba is a nutritionist with experience in community and clinical research. She has worked on nutrition, ...
Read More +