-
CENTRES
Progammes & Centres
Location

Jessie Huang and Deepesh Vendoti, “The Fight Against Infectious Diseases: Considerations for Public Health Systems and International Cooperation”, ORF Occasional Paper No. 206, August 2019, Observer Research Foundation.
I. Introduction
The severe acute respiratory syndrome (SARS)[1] outbreak in 2003 provoked fear in the global community.[1] The outbreak quickly spread, causing some 8,098 people to fall ill; of them, 774 died. The disease crossed borders, reaching to more than two dozen countries in North America, South America, Europe, and Asia before it was contained.[2] Across the world, news of the outbreak[2] triggered extreme precautions to contain the spread of the disease. In many airports across Asia, nurses wore protective gear as they assessed arriving passengers for signs of disease. In Hong Kong, hospitals were overrun, apartments quarantined, and public places were deserted.[3] The symptoms of SARS closely resembled the common cold or flu, allowing it to easily escape diagnosis and no treatment or drug could contain the outbreak.[4]
The SARS epidemic is only one example of the potential magnitude and severity that infectious diseases can have, even at a time of medical advances. For one, ease of travel comes with the concomitant challenge of securing people against the transmission of disease. The SARS outbreak demonstrated how quickly an infectious disease can spread across borders, worsen within people who have contracted the disease, and pose serious risks to healthcare workers.
Indeed, close to 200 outbreaks of infectious diseases are recorded across the world every year.[5] According to the World Health Organization (WHO), new infectious diseases like SARS are emerging and familiar ones like Ebola are reappearing in new territories.[6] Infectious diseases pose serious burdens to the global community, particularly in low-income countries whose healthcare systems are already strained, to begin with. Over half of all deaths in low-income countries in 2016 were caused by infectious diseases; these diseases also caused ill-health conditions during pregnancy and childbirth, and nutritional deficiencies.[7]
Studies have shown that the number of outbreaks and the kinds of diseases have increased since 1980. However, the number of outbreak cases per capita has declined over time.[8] This suggests that despite an overall increase in outbreaks, there have been global improvements in prevention, early detection, and control that have brought down the number of people affected in each outbreak. These improvements are the result of medical advances in detecting such diseases through diagnostics, treating them with medicines, and preventing them using vaccines.
The response to infectious diseases must be analysed through the lens of public health: nations should follow the multisectoral approaches of coordination and cooperation to prevent disease and protect human health. This framework includes strengthening disease surveillance systems, training public health officials to quickly coordinate action, and investing in research to develop countermeasures like medicine, vaccines, and accurate diagnostics.
This paper examines the history of recent infectious disease outbreaks and outlines the global responses. It raises important questions about the shortcomings of both governments and the international community. Using the cases of recent outbreaks such as the Ebola virus in the Democratic Republic of the Congo, and the Nipah virus in India, the paper makes the case for the improvement of domestic public health infrastructure and the ecosystem of international cooperation.
The emergence of a disease is dependent on factors ranging from the tiny microbial agents to the human host, to the wider environment. Understanding these factors helps identify the necessary measures in scientific research and policy development.
Table 1: Major factors that underlie disease emergence and re-emergence
| Microbial Agents | Human Host | Human Environment |
| Genetic adaptation and change | Human susceptibility to infection | Climate and weather |
| Polymicrobial diseases | Human demographics and behaviour | Changing ecosystems |
| International trade and travel | Economic development and land use | |
| Intent to harm (bioterrorism) | Technology and industry | |
| Occupational exposures | Poverty and social inequality | |
| Inappropriate use of antibiotics | Lack of public health services | |
| Animal populations | ||
| War and famine | ||
| Lack of political will |
Source: Morens DM, Fauci AS. “Emerging Infectious Diseases: Threats to Human Health and Global Stability.” PLoS Pathogen (2013), 9 no. 7.
Despite medical advances that include the development of vaccines, antivirals and antibiotics, there are wider-scale trends that determine the spread of an infectious disease. These include rising human mobility, population growth, and rapid urbanisation.[12] The spread of an infectious disease is primarily driven by human mobility. Global trade, travel, and connectivity have grown exponentially.[3] When a new pathogen is introduced to a new location, local people are biologically more susceptible because of their lack of immunity.[13] Additionally, urbanisation has given rise to breeding environments for epidemics. Unhygienic city spaces and agricultural spaces with greater contact with animals pose serious risks. Deadly zoonotic diseases are caused by pathogens from animals that can survive outside their host to infect humans.[14]
II. Contemporary Contagions: Impact and Response
The number of outbreaks, and the number of kinds of disease, have increased significantly since 1980. The proportion of diseases transmitted by animals and other vectors has also risen relative to those that are human-specific.[15]
Figure 1: The global number of human infectious disease outbreaks and richness of causal diseases from 1980 to 2010. Outbreak records are plotted with respect to (a) total global outbreaks (left axis, bars) and total number of diseases causing outbreaks in each year (right axis, dots), (b) host type, (c) pathogen taxonomy, and (d) transmission mode.
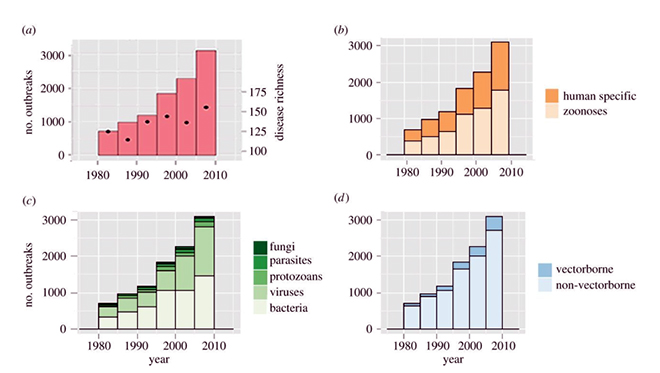
This section analyses the more recent episodes of infectious disease outbreaks, and the successes and failures of the response.
In November 2002, a form of atypical pneumonia began to spread from the Guangdong province in China. Eventually, the same symptoms showed in more than 5,000 people, killing 349 of them across the country. The epidemic spread to other countries, which would finally number nothing less than 26.[4] Epidemiologists would name the illness, Severe Acute Respiratory Syndrome (SARS).
Investigators found that Hong Kong was ground-zero for the illness. Its officials were widely acknowledged for their willingness to share information. In contrast, China proved to be a stumbling block to gathering as much data about the disease, and as early as possible. Its officials failed to communicate properly and efficiently with medical practitioners and the general public; this allowed the disease to spread quicker than it would have, if initial response mechanisms had been put in place as the epidemic erupted.[16] The initial document submitted to the provincial health bureau of China was classified. It also did not mention any signs of contagion, nor did it call for measures to protect the health workers who would soon contract the illness.[17]
China’s response to the SARS epidemic raised crucial questions about the capacity and functioning of its political structure and its ability to address future outbreaks. There is evidence that the Chinese government decided to be opaque about the spread of the disease because of concerns over how SARS could impact its economic development.[18] Overall, the epidemic revealed major weaknesses in the healthcare systems of not only China but the other affected countries as well; these failures compromised patient care and the safety of health workers. China has since apologised.[19] It has also made greater investments in public health initiatives, strengthened its national and local surveillance systems, and expanded laboratory capacity.[20]
Equally importantly, China needed to increase its dedication to international cooperative efforts.[21] The SARS outbreak showed how isolated actions by China in favour of its national interests can be counterproductive and squander any chances of containing the threat of an epidemic. After initial hesitation to share information, China did launch an active campaign against SARS and eventually successfully eliminated the disease.[22]
The SARS epidemic laid the foundations for the framework of international cooperation to contain such similar outbreaks. In particular, there needs to be prompt and public reporting of diseases, travel recommendations and screenings across borders, and international collaboration in the scientific community. The epidemic contributed to the building of stronger collaborations with national and international agencies, while stepping up financial investments for collective preparedness.
In terms of forming a coordinated international response, the World Health Organization (WHO) had established the International Health Regulations (IHR) in 1969 to help monitor and control four serious diseases that had significant potential to spread between countries. These original IHR were designed to monitor and control four serious infectious diseases: cholera, plague, yellow fever and smallpox. In the wake of an unabated increase in the scale and diversity of infectious diseases, the WHO decided to revise the IHR in 1995. It also became clear that these outdated regulations needed to address the increasing travel and trade.[23] However, by the time of the SARS outbreak in 2003, the IHR of 1969 had become inadequate in managing newer infectious diseases.
Because of the scale and impact of the SARS outbreak, amendments to the IHR were finalised in 2005, and the regulations, in a much-strengthened form, came into force in 2007.[24] These new regulations created a global legal framework that enabled nations to facilitate coordinated responses to public health risks and emergencies. The revisions placed emphasis on mitigating the effects of biological threats on human lives and economies, while avoiding restrictions on international trade and travel. These amendments to the IHR in 2005 paved the path for nations to notify to WHO all events with potential for public health emergency of international concern. The WHO took on the responsibility to coordinate the fight against any infectious diseases that threaten international health. This open communication is coupled with WHO’s ability to issue a Public Health Emergency of International Concern (PHEIC) declaration.[25] This combination proves to be an effective solution to flag potential threats that require a well-coordinated international response.
In addition to coordinating an effective response, the international community also worked to strengthen surveillance mechanisms to detect disease. The following year, the World Bank set up the European Union-led Avian and Human Influence Facility (AHIF) which is supported by Australia, China, Estonia, Iceland, India, Korea, Russia, Slovenia and the United Kingdom. In the final years of its existence, over US$1.3 billion was available to over 60 countries to strengthen early identification and response mechanisms against outbreaks of imminent threat.[26] There was significant progress made in these participating countries as global cooperation facilitated greater preparedness. The success of AHIF also underscored the need for continual efforts to build platforms that are regionally connected, internationally networked and financially sustained.
The Middle East Consortium on Infectious Disease Surveillance (MECIDS) is another example on how regional cooperation stems from shared concerns and the collective strengths of a region. The organisation was active during the same period with the support of the AHIF and Nuclear Threat Initiative. MECIDS is a cooperative arrangement between the health ministries in Jordan, Palestine and Israel along with their respective scientific institutions. These institutions all worked together across the food safety, veterinary and human health sectors.[27] Despite bitter political differences, their collective effort improved surveillance, monitoring and analyses of the entire region.
These efforts at strengthening systems for outbreak alert and response became the clear method to defend public health security against an outbreak like SARS, in addition to future infectious disease threats. These collective improvements in international coordination, especially in the Middle East through MECIDS, became especially relevant in 2012 when the Middle East Respiratory Syndrome (MERS), a viral outbreak similar to SARS, was identified in Saudi Arabia. The disease is similar to SARS since they are both zoonotic, meaning humans become infected from animals, particularly camels common in the region, and the disease is caused by a coronavirus that can result in death. Though transmission from camels is endemic to the region, countries neighbouring Saudi Arabia as well as distant ones started reporting infections. The disease eventually spread to 27 countries.[28] The new outbreak suggests that growing threat of zoonotic infectious diseases in recent decades also requires strengthening information flow and coordinating decisions across veterinary and human health systems.
The 2014 Ebola outbreak in West Africa not only exposed critical weaknesses in the health systems of those poor countries in the continent, but also highlighted the lack of preparedness globally. The outbreak prompted multiple institutional and collaborative global efforts, including aiding and cooperating internationally, investing in vaccine development, and providing financial support to developing nations.
Due to the weak surveillance systems and poor public health infrastructure of the developing nations of West Africa, the Ebola outbreak caused deaths in half of those who acquired the syndrome. To be sure, the Ebola virus had been discovered as early as 1976; the world had seen 29 epidemics, affecting more than 2,000 people, by the time the West Africa episode happened.[29] In those times, however, the spread of the virus was limited to specific regions within the African continent, unlike in 2014, when the rash of infections reached farther territories.[30]
By the time the world recognised the magnitude of the outbreak and began to respond, the entirety of West Africa was in the grip of panic. Though the virus and form of transmission was the same, the Ebola virus for the first time, spread across many more countries including to developed nations. This fast movement of the disease was due to the increased mobility across borders, more crowded urban areas, and gaps in the countries’ infection control mechanisms. The transmission to developed nations was facilitated by human travel, including health personnel returning from the affected regions (See Table 2). Consequently, cross-border restrictions on the movement of people and goods were enforced. In addition to human health effects, this epidemic also had a snowballing socioeconomic impact as it affected tourism and infrastructure projects.[31]
Table 2: The Transnational Impact of the 2014 Ebola Outbreak
| Country | Total Cases (Suspected, Probable, Confirmed) | Laboratory Confirmed Cases | Total Deaths |
| Countries with Widespread Transmission | |||
| Guinea | 3,814 | 3,358 | 2,544 |
| Liberia | 10,678 | 3,163 | 4,810 |
| Sierra Leone | 14,124 | 8,706 | 3,956 |
| Affected Countries | |||
| Italy | 1 | 1 | 0 |
| Mali | 8 | 7 | 6 |
| Nigeria | 20 | 19 | 8 |
| Senegal | 1 | 1 | 0 |
| Spain | 1 | 1 | 0 |
| UK | 1 | 1 | 0 |
| US | 4 | 4 | 1 |
| Total | 28,652 | 15,261 | 11,325 |
Source: CDC, USA
The Ebola epidemic of 2014 showed that the world was unprepared to meet a threat of such scale and speed. Countries under attack in the West African region hardly had the human and financial resources for even their existing health problems, let alone a spate of deadly viral infections.
WHO failed to red-flag the disease early enough, in turn causing the delay in response from the international community.[32] The organisation initially believed that sufficient funds would be mobilised without much difficulty in the hour of crisis. In reality, WHO had to spend the most crucial early days advocating and pooling the required resources to overcome the Ebola attack. It started with a modest financial appeal for US$4.8 million in April 2014, which was raised to US$71 million by July 2014. In August that year, it gave a revised call for US$490 million and within the next few weeks, the United Nations (UN), too, had to make an appeal to raise another billion dollars.[33] These repeated appeals and delays revealed glaring deficiencies in financial estimation, mobilisation and emergency preparedness on the part of international agencies.
While WHO and the international community were falling short in securing a matching response, the United States (US) government stepped up its contribution significantly on multiple fronts. Beyond financial resources, the US also mobilised more than 3,700 public health personnel from its Centres for Disease Control (CDC) and around 3,000 from its military and deployed them to the affected countries.[34] Then President Barack Obama obtained Congressional approval for US$5.3 billion for the emergency, including US$3.7 billion exclusively for international activities for the West African Ebola outbreak.[35] The US did not only provide funds for the immediate needs in the affected territories, but also helped strengthen international efforts of preparedness over the next five years. The federal government designated the United States Agency for International Development (USAID) as a nodal agency to coordinate the work of various departments, with the CDC being the medical lead.
WHO eventually admitted to its shortcomings and promised reforms in its efforts for global coordination.[36] The aftermath of the Ebola outbreak also highlighted issues of underfunding and inadequate financial reserves to tackle such biological threats. Both WHO and the UN acknowledged the need to increase investments in research and development for clinical tools such as vaccines.
WHO established a new dedicated Health Emergencies Programme (HEP) to focus on outbreaks of public health concern.[37] It also set up the Contingency Fund for Emergencies (CFE) to bridge funding gaps in nations with weak economies that are unable to allocate adequate resources in response to outbreaks.[38] These mechanisms to manage funds helped reduce delays in pooling funds in times of crisis.
Critical shortages in health personnel were common among the countries heavily affected by the outbreak. Countries like Guinea, Liberia and Sierra Leone were in various stages of recovery after years of internal conflict and lacked prior experience in witnessing and handling Ebola outbreaks. Despite the increasing global attention and incremental improvements after repeated outbreaks, a number of crucial missing links surfaced during the Ebola episode. There were glaring concerns in weak leadership, financial deficiencies, inadequate preparedness among the health personnel, and gaps in risk communication.
By the time WHO issued the Public Health Emergency of International Concern (PHEIC) status alert, finally unlocking contributions from the international community, Ebola had spread across 10 nations and the death toll had spiked up to over 11,000.[39] West African countries whose health systems were already suffering even before the epidemic registered maximum losses.[40] A World Bank report estimated Ebola’s economic impact in 2014-15 to be around US$32.6 billion. This sum was largely due to indirect economic losses, which could have been avoided if there was improved preparedness.
Table 3: Collective contributions to WHO Contingency Fund for Emergencies (CFE); Allocations for affected countries.
| Collective Contributions of Nations to WHO’s CFE | Allocations to various nations from WHO’s CFE | |||
| Total in 2015-2018 US $ | Total in 2018 US $ | |||
| Germany | 22 641 591 | DR Congo | 5 250 000 | |
| UK | 16 178 585 | Bangladesh | 3 500 000 | |
| Japan | 10 833 800 | Regional Africa | 1 550 000 | |
| Australia | 3 017 985 | Nigeria | 2 050 406 | |
| Netherlands | 2 309 508 | Somalia | 489 500 | |
| Canada | 2 252 932 | South Africa | 373 220 | |
| Korea | 2 015 192 | Uganda | 225 000 | |
| China | 2 000 000 | Papua New Guinea | 135 000 | |
| Denmark | 1 621 534 | Regional Pacific | 108 385 | |
| France | 1 418 218 | Mozambique | 100 000 | |
| Norway | 1 275 348 | Venezuela | 50 000 | |
| Sweden | 1 159 555 | Republic of Congo | 50 000 | |
| India | 1 000 000 | Angola | 40 000 | |
| Luxembourg | 613 497 | Total | 13 921 511 | |
| Kuwait | 500 000 | |||
| Estonia | 145 287 | |||
| Malta | 20 000 | |||
| Total | 69 003 030 | Updated June 1, 2018 | ||
Source: WHO, Contingency Fund for Emergencies (CFE).
In 2015, WHO evolved a global strategy in this regard though its Research & Development Blueprint for Action to Prevent Epidemics. From 2016 to 2018, WHO has been periodically reviewing the list of priority diseases for research, development, and preparedness in preparation for potential public health emergencies.[41]
Figure 2: Research and Development (R&D) Funding from 2007 to 2015 for rare and neglected diseases including emerging threats.
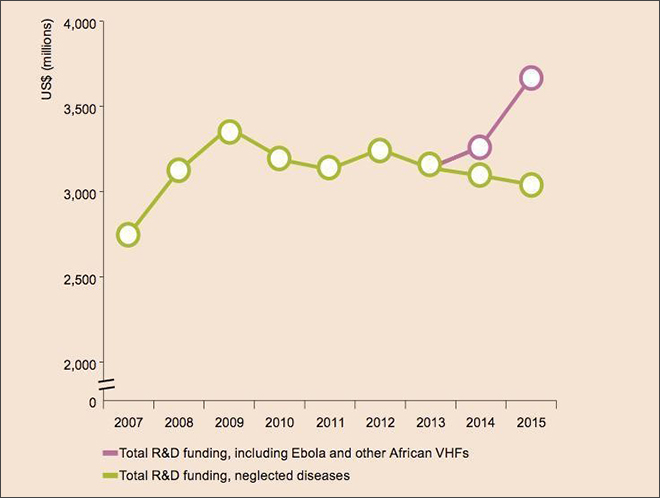
There has been significant ongoing R&D for the production and supply of vaccines. Vaccines operate by providing an acquired immunity to a particular disease, preventing the spread of epidemics among the unaffected populations. However, even for well understood causative viruses, this process could take at least six to eight months.[42] Development for newly emerging diseases, particularly of zoonotic origin, could take much longer. Together with the time expense of mass production and delivery, vaccines cannot serve as a timely solution during epidemics.[43]
In terms of the 2014 Ebola outbreak, there were extensive efforts in vaccines that resulted in the final phase of research for Ebola Vaccine, ‘rVSV-ZEBOV’.[44] There was excitement within the international scientific community over the possibility of developing vaccines in reasonably short time frames, even for an extremely challenging virus like Ebola. The vaccine was used on a trial basis and was only made available towards the end of outbreak in 2016. As a result, the vaccine missed the opportunity to save lives and reduce the socioeconomic consequences.
During this same period, German Chancellor Angela Merkel hosted the G7 meeting in June 2015 in Bavaria, Germany—with Canada, France, Italy, Japan, the United Kingdom, and the United States. She made a strong appeal for global health reforms against the backdrop of Ebola.[45] This was followed up during the World Economic Forum’s (WEF) annual meeting in Davos in 2016 when the economic and political leaders agreed to launch a focused initiative to strengthen outbreak response mechanisms. At the following World Economic Forum (WEF) in January 2017, the Coalition for Epidemic Preparedness Innovations (CEPI) was launched, in recognition of the failure of the free market to catalyse the vaccine industry. CEPI’s primary objective is to accelerate the development of vaccines for emerging infectious diseases.[46]
CEPI has been a transformative step supported by innovative partnerships between public, private, philanthropic and civil organisations. These organisations have worked together to ensure all components like vaccine discovery and delivery are in place in times of crisis. CEPI has members from all spheres of influence including public, private and civil society organisations. The first phase of CEPI funding pushed for candidate vaccines including the emerging and newer pathogens of MERS-CoV, Nipah and Lassa viruses, which are all among WHO’s current list of priority diseases.[47]
There were significant difficulties and delays in securing funds during the 2014 Ebola outbreak, prompting the World Bank to make changes. The Ebola outbreak, in particular, proved that regardless of the preparedness of nations involved, funds need to be mobilised immediately during emergencies. The Ebola outbreak affected a number of nations with weaker economies and infrastructure which posed an insurmountable challenge by exceeding budgeted amounts.
To address this challenge, the World Bank launched the ‘Pandemic Emergency Financing’ (PEF) Facility in coordination with WHO. This was the first-ever initiative that has raised funding through bonds in preparation against infectious diseases.[48] The PEF facility began operating in 2017. The facility set aside US$425 million to be readily available for poor nations as an insurance option. The money set aside is used to stop or prevent the spread of outbreaks within an appropriate time frame.[49]
This fund can become available for all the outbreaks mentioned in WHO’s priority list and by default to all the countries eligible for funding from the World Bank’s International Development Association (IDA). Germany has invested an additional amount of US$61 million to the PEF to be used as flexible cash bailouts within 48 hours to enable poor nations to meet the urgent requirements. The PEF facility was initially intended to be operational for only three years until 2020. However, its success before then could offer valuable insights for further changes or an extension.[50]
Another Ebola epidemic hit the Democratic Republic of the Congo in May 2018. This time, the international response relied on the improvements adopted three years earlier, resulting in a more timely response. In addition, since the Democratic Republic of the Congo already had experience with Ebola outbreaks on eight occasions in the past, the country had significant understanding of the disease. This timely international intervention, coupled with greater understanding within the country, prevented the disease from rapidly spreading outside the DRC.[51]
Figure 3: International Donor Pledges of Financial Support for the Democratic Republic of the Congo Ebola Response (as of May 24, 2018; in USD millions)
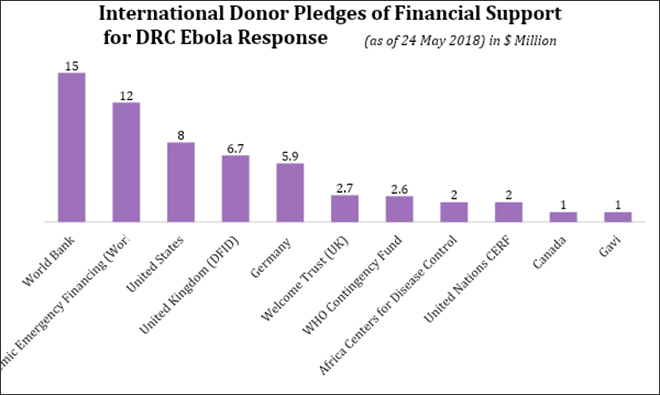
Note: Based on 23 May 2018 exchange rates. World Bank’s $15 million is a reallocation of funds previously planned as a three-year investment in disease surveillance in the country.
The first appeal of WHO was for US$26 million and was met within a few days. Various other international agencies and member states were prompt in sharing resources so collective financial cooperation provided early relief in May 2018.[52] In the previous major Ebola outbreak in 2014, the US, specifically the Obama administration, was the largest contributor in aid for the epidemic. However, in a turn of events in 2018, US President Donald Trump announced the revocation of the US$252-million aid pledged by the Obama administration. This revocation dampened global efforts to counter outbreaks.[53]
For the first time in history, the vaccine was developed in a timely fashion and successfully protected people against Ebola during the middle of the outbreak. The vaccine was supported financially by international organisations including the Global Alliance for Vaccine and Immunisation (GAVI).[54] The “ring vaccination” method was used, which means the spread of the disease was inhibited by only vaccinating those who are mostly likely infected. The vaccine was given to over 3,000 on site, including healthcare personnel and others who came in contact with the infected.[55]
By the end of July 2018, the outbreak was reported to be have tapered off. On July 24, WHO even declared the end of DRC Ebola outbreak.[56] However, soon after in August, there were more cases found in the Kivu province of the DRC. This new outbreak soon escalated to the second largest ever Ebola outbreak in 2019.[57] Despite significant progress, global efforts need to continue to contain and eradicate this disease.
At the moment, the 2019 Ebola outbreak has continued to persist in the Democratic Republic of the Congo due to the lack of adequate funding and strained human resources. The Ebola virus even crossed borders from the DRC to Uganda, constituting an international spread of disease.[58] As of 10 July 2019, a total of 2,418 cases and 1,630 deaths have been reported.[59] However, as of 14 June 2019 at the third review of the situation, a PHEIC declaration has not been made because the outbreak does not meet all criteria and only affects this region. The PHEIC declaration was not made because it poses serious risks to the local economy by enacting travel and trade restrictions.[60]
This time around, there are vaccines and experimental treatments available including Merck’s VSV-EBOV, the unlicensed Ebola vaccine. However, it has been difficult to control the outbreak because of the distrust and violent attacks on healthcare workers.[61] Many people at risk have refused the vaccine, which has hindered efforts to contain the spread. These management efforts require much more funding and resources from the international community. WHO needed US$98 million in funding but only received US$44 million. The US$54-million gap in funding was crucial for sustaining the response without reducing or halting operations in areas in need.[62] WHO’s recommendations for managing the outbreak also included optimal vaccine strategies, community engagement, and improved detection and screening.[63] The continued fight against Ebola raises serious concerns about the control of infectious diseases in developing nations. Even when biomedical solutions like a successful vaccine are made available, there are still barriers to protecting people at risk and containing the disease.
III. The Emerging Threats in India
India carries a disproportionate burden of global infectious diseases, ranking 64th out of 462 countries in burden of communicable diseases, particularly ones of zoonotic origin.[64] The rapid urbanisation, for instance, that has increased mobility and led to greater density has raised new challenges to sanitation and healthcare.[65] There are other environmental, demographic, and socio-economic factors that put India at strong risk for communicable diseases, including its large population that facilitates transmission of disease and changes in agricultural practices that introduce zoonotic pathogens.[66]
The Nipah virus outbreak of 2018 in the state of Kerala is a prime example of the recent severe challenges to India’s infectious disease management infrastructure. The virus was first discovered in 1999 in a village in Malaysia. In May 2018 it emerged as a serious public health threat when the virus appeared in Kerala and claimed 17 lives. The lack of a vaccine or specific drug treatment further inhibited efforts to mitigate the impact of the epidemic.[67]
Soon after Kerala health authorities reported the first set of cases to the National Centre for Disease Control (NCDC), the Ministry of Health coordinated a response between local, state, and national agencies. The local Government of Kerala’s Department of Health and Family Welfare rapidly called for infection prevention and control, patient isolation, and protective equipment use for healthcare personnel on the frontlines of the response. A multidisciplinary team was mobilised at the national level, consisting of the National Centre for Disease Control; the All India Institute of Medical Sciences; the Department of Animal Husbandry, Dairying & Fisheries; the Division of Emergency Medical Relief; and Ram Manohar Lohia Hospital in New Delhi. The coordination and information-exchange from multiple sectors helped to quickly detect cases, treat patients, contain the spread, and protect the health workers.
For their part, the local governments launched a communication and education campaign for the public. In response to the sense of panic and fear, district governments worked to informing the public on best practices for protection against the illness, including the safe cremation of those who die of the infection. By June 2018, health officials declared that the outbreak had been successfully contained, meaning there were no new infections and there were no new people who were contracting the disease.[68] The public health response in Kerala succeeded in coordinating between all levels of leadership which prevented the situation from worsening.[69]
Yet, there continue to be gaps in India’s local government and public health systems. In 2019, the re-emergence of Nipah in Kerala and the continued outbreaks of acute encephalitis syndrome, recently in the state of Bihar, have called attention to the weak surveillance systems, lack of public awareness, poor nutrition and sanitation, and ill-equipped health facilities.[70] [71] These recent outbreaks in India highlight the successes and shortcomings in local responses at a crucial stage in infectious disease management. Adequate public health systems and multi-sectoral coordination at this early, local stage play an important role in containing diseases that could lead to national and global spread like SARS and Ebola.
IV Recommendations
National governments and international health agencies should work together to adopt urgent measures towards building the resilience of public health ecosystems in preventing and combating infectious diseases. The following are some of the most crucial and immediate tasks.
The first step to improving defence against outbreaks is strengthening surveillance mechanisms. WHO’s global leadership should require transparency from amongst the member nations, for them to be willing to share and seek mutually beneficial resources across national boundaries. This early detection must seamlessly feed into global networks of surveillance and monitoring.
All nations should be equally respectful and uniformly compliant with the International Health Regulations of 2005, which mandated nations to notify the WHO on all events that have the potential to escalate to a public health emergency of international concern. Moreover, nations should follow the joint external evaluation (JEE) framework, which is a voluntary, collaborative process to assess country capacities to prevent, detect and rapidly respond to public health risks. The JEE helps countries identify the critical gaps within their human and animal health systems. Since it is voluntary, nations that are yet to adopt the JEE processes must be encouraged and incentivised. This framework also serves as a strategic means for countries to protect their own environments, livestock, livelihoods and most importantly, human lives.
The outbreaks of Ebola, SARS, and Nipah in recent years have emphasised the importance of communications across multiple key sectors, not only in health. The emergency response to containing disease is dependent on a multitude of domains including agriculture, animal health, financial markets, the travel industry, sanitation, and defence. Therefore, protection and prevention ecosystems need to be holistic. In the midst of an outbreak, it is not enough to focus on medical solutions. For zoonotic infectious diseases like SARS, MERS, and Nipah viruses, in particular, coordination should be improved between the various departments mandated in agriculture, animal health, and human health. This approach aligns with the “One Health” goal[5] which involves designing programmes, policies, legislation and research in which multiple sectors work together to achieve better public health outcomes.[72]
The “One Health” concept must be institutionalised across ministries, departments, and decision-makers at all levels. There must be surveillance across veterinary branches, environmental sciences, agricultural crops and human populations. This surveillance must seamlessly feed into the planning and preparation of medical, health, paramedical, veterinary and environmental personnel. One Health’s resulting evaluation and corrective practices should not be viewed as a threat to the global trade and local business ecosystems. Animal health monitoring, biosecurity, quarantining and culling are costly measures that need to be undertaken in support of human health. Investments towards early detection and management at the animal population level are more cost-effective and less catastrophic than primarily focusing on human contexts. However, nations need to move beyond optimising financial gains, and towards recognising the need for sharing resources, protecting animal-linked livelihoods, and securing the border movements of food products.
The management of an infectious disease outbreak is greatly dependent on vaccine development. As witnessed in response to the Ebola outbreak, effective vaccine development and distribution of those vaccines can help contain the epidemic. Furthermore, widespread access to genomic information and collaborative research in the international level can help quickly develop clinical tools. All nations, regardless of their own perceived threats, should have maximal overlap with the priorities identified on WHO’s Research and Development Blueprint and 2018 priority lists[6] in the development of new vaccines.
The response to the Ebola outbreak of 2014 was greatly dependent on emergency funding through CEPI and aid from the United States. The rapid pooling of resources and financial assistance for economically weaker nations is crucial. Therefore, in the future, increased endorsement for these funds is instrumental, especially for lower- and middle-income developing nations that are susceptible to epidemics.
Conclusion
The rise in infectious outbreaks in recent years has revealed limitations in public health systems, international collaboration, and prophylactic solutions. Over the last 20 years, the international community has learned from various major epidemics, including SARS, Zika, and the constantly re-emerging Ebola virus. Likewise, local and national governments such as in India have effectively managed localised outbreaks to prevent rapid and widespread movement across borders. The government of India has learned from and improved response for the Nipah outbreak. The aftermath and response to these epidemics are strong indicators of what to expect, which can be used to make changes for inevitable future infectious disease outbreaks.
The solution to combating infectious disease outbreaks lies in sustained, collaborative and institutionalised global efforts. The global rise in infectious disease outbreaks warrants preparedness through an internationally networked approach. As these global outbreaks like Ebola and local outbreaks of Nipah inevitably continue, future changes must follow these multisectoral principles of coordination and cooperation between and within nations in addition to the public health values of early preparedness and response. Nations have a clear opportunity and obligation to define their responsibilities and enhance their contributions to make this world safer.
About the Authors
Jessie Huang is an intern with the Observer Research Foundation office in Mumbai. She is a junior at Wellesley College near Boston, MA, studying chemistry and women’s and gender studies. Her research interests include social determinants of health, women’s reproductive health, and computational sciences.
Deepesh Vendoti is a former consultant at ORF-Mumbai’s Health Initiative. He is a medical doctor by training and a public health management graduate from Yale University.
Endnotes
[1] SARS is a viral respiratory disease of zoonotic origin. Symptoms resemble a flu and include fever, muscle pain, lethargy, cough, and sore throat. In early 2003, this single disease quickly spread to 29 countries, killing ten percent of the people infected, including many healthcare workers.
[2] An outbreak is defined as the occurrence of cases of disease in excess of what would normally be expected in a defined community, geographical area or season. An outbreak may occur in a restricted geographical area, or may extend over several countries. It may last for a few days or weeks, or for several years. The term, “outbreak” refers to either an epidemic or pandemic restricted to a small geographical area or population.
[3] Air travel, in particular, has grown eight-fold in the last four decades and is further expected to double by 2035[3].
[4] Of these 26 countries, the East Asian countries were predominantly affected. Besides China, where the outbreak originated, Hong Kong, Taiwan, Singapore, and Vietnam reported cases of SARS.
[5] The ‘One Health’ concept is an approach employed by programmes, legislation, research, and multiple sectors to better communicate and achieve improved health outcomes. In particular, coordination across multiple sectors through food safety and control of zoonoses that can be contracted from animals. The approach is employed by many organisation and sectors to better public health. For example, the World Health Organisation works with the Food and Agricultural Organisation of the United Nations and the World Organisation for Animal Health.
[6] The World Health Organisation Research and Development Blueprint List of Priority Diseases is a special tool developed by WHO to determine which diseases and pathogens to prioritise for research and development for public health purposes. It is not an exhaustive list nor does is it indicative of the next epidemics.
[1] “SARS spread leads to fears, questions,” ABC News, April 4, 2013.
[2] “SARS Basics Fact Sheet,” About SARS, Centres for Disease Control and Prevention, last modified December 6, 2017.
[3] “In Pictures: Hong Kong during the 2003 SARS epidemic,” Hong Kong Free Press, February 19, 2017.
[4] Jong-Wha Lee and Warwick J. McKibbin, Learning from SARS: Preparing for the Next Disease Outbreak (Washington (DC): The National Academies Press, 2004)
[5] “Emergencies preparedness, response,” The World Health Organisation, last modified December 22, 2017.
[6] “A Safer Future: Global Public Health Security in the 21st Century,” The World Health Report 2007, The World Health Organisation, last modified May 7, 2007.
[7] “The top 10 causes of death,” The World Health Organisation, last modified May 24, 2018.
[8] Katherine F. Smith et al, “Global rise in human infectious disease outbreaks,” Journal of the Royal Society Interface 11 (2014).
[9] Mauricio L Barreto, “Infectious diseases epidemiology,” Journal of epidemiology and community health 60, no. 3 (2006).
[10] Ibid (11)
[11] Ibid (11)
[12] Ibid (11)
[13] Johanna F Lindahl and Delia Grace, “The consequences of human actions on risks for infectious diseases: a review,” Infection ecology & epidemiology 5 (2015).
[14] Carl-Johan Neiderud, “How urbanization affects the epidemiology of emerging infectious diseases,” Infection ecology & epidemiology, 5 (2015).
[15] Ibid (13)
[16] Yanzhong Huang, “Implications of SARS Epidemic for China’s Public Health Infrastructure and Political System, Testimony before the Congressional-Executive Commission on China Roundtable on SARS,” Congressional-Executive Commission of China, May 12, 2003.
[17] Ibid (11)
[18] Ibid (4)
[19]“China Apologises for Slow Response to SARS Outbreak,” Voa News, October 30, 2009, https://www.voanews.com/archive/china-apologizes-slow-response-sars-outbreak
[20]Yanzhong Huang, “The SARS Epidemic and its aftermath in China : A political Perspective,” Learning from SARS: Preparing for the Next Disease Outbreak, (DC: National Academies Press US, 2004),
[21] “China Apologises for Covering Up SARS Cases,” Fox News, April 4, 2003, http://www.foxnews.com/story/2003/04/04/china-apologizes-for-covering-up-sars-cases.html
[22] Amena Ahmad, Ralf Krumkamp, and Ralf Reintjes, “Controlling SARS: a review on China’s response compared with other SARS-affected countries,” Tropical Medicine and International Health, 1, 36-45 (2009) https://doi.org/10.1111/j.1365-3156.2008.02146.x
[23] “World Health Assembly adopts new International Health Regulations,” The World Health Organization, May 23, 2005, https://www.who.int/mediacentre/news/releases/2005/pr_wha03/en/
[24] Singh Sujeet Kumar and Sudhir Kumar, “International Health Regulations: a major paradigm shift from 1969 to 2005,” Journal of Communicable Diseases 41, no. 2 (2009): 113-116.
[25] “International Health Regulations,” The World Health Organisation last modified 2005, https://www.who.int/ihr/publications/9789241580496/en/
[26] “Avian and Human Influenza Facility,” The World Bank, last modified October 31, 2013, http://www.worldbank.org/en/topic/pandemics/brief/avian-human-influenza-facility
[27] Louise S Gresham et al. “Creating a Global Dialogue on Infectious Disease Surveillance: Connecting Organizations for Regional Disease Surveillance (CORDS),” Emerging Health Threats Journal 6, no. 1 (2013), https://doi/full/10.3402/ehtj.v6i0.19955
[28] “Middle East respiratory syndrome coronavirus (MERS-CoV),”, The World Health Organisation, last modified February 19, 2018, http://www.who.int/news-room/fact-sheets/detail/middle-east-respiratory-syndrome-coronavirus-(mers-cov)
[29] Coltart CE et al., “The Ebola outbreak, 2013-2016: old lessons for new epidemics,” Philosophical Transactions of the Royal Society B 372, no. 1721 (2017) http://doi.org/10.1098/rstb.2016.0297
[30] Ibid (37)
[31] Cordelia E. M. Coltart, Benjamin Lindsey, Isaac Ghinai, Anne M. Johnson, and David L. Heyman. “Public health impact of the 2014–2015 Ebola outbreak in West Africa: seizing opportunities for the future,” BMJ Global Health 372, no. 1721 (2017), http://doi.org/ 10.1098/rstb.2016.0297.
[32] “Pushed to the limit and beyond: a year into the largest ever Ebola outbreak,” Medecins Sans Frontières (MSF), last modified March 23, 2015, https://www.msf.org/ebola-pushed-limit-and-beyond
[33] Ibid (40)
[34] “The Latest Ebola Outbreaks: What Has Changed in the International and U.S. Response Since 2014?” Henry J Kaiser Family Foundation, last modified May 25, 2018, https://www.kff.org/global-health-policy/issue-brief/the-latest-ebola-outbreak-what-has-changed-in-the-international-and-u-s-response-since-2014/
[35] Jennifer Kates et al., “The U.S. Response to Ebola: Status of the FY2015 Emergency Ebola Appropriation,” Henry J Kaiser Family Foundation, last modified December 11, 2015, https://www.kff.org/global-health-policy/issue-brief/the-u-s-response-to-ebola-status-of-the-fy2015-emergency-ebola-appropriation/
[36] Tom Miles, “WHO leadership admits failings over Ebola, promises reform,” The Reuters, April 20, 2015,
https://www.reuters.com/article/us-health-ebola-who-idUSKBN0NA12J20150419
[37] “WHO’s new Health Emergencies Programme,” The World Health Organization, last modified October 31, 2016, https://www.who.int/features/qa/health-emergencies-programme/en/
[38] “Contingency Fund for Emergencies (CFE),” The World Health Organization, last modified July 23, 2019, https://www.who.int/emergencies/funding/contingency-fund/en/
[39] “2014-2016 Ebola Outbreak in West Africa,” The Centres for Disease Control and Prevention (CDC), last modified March 8, 2019, https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html
[40] “Ebola: Mapping the outbreak,” BBC, January 14, 2016, https://www.bbc.com/news/world-africa-28755033
[41] “A research and development Blueprint for action to prevent epidemics,” The World Health Organization, https://www.who.int/blueprint/en/
[42] Stanley Plotkin et al. “The complexity and cost of vaccine manufacturing – An overview,” Vaccine 35, no. 33 (2017): 4064-4071, https://doi.org/10.1016/j.vaccine.2017.06.003
[43] Christopher K Brown. “Ebola vaccine: What took so long?” Bulletin of the Atomic Scientists, May 31, 2018, https://thebulletin.org/2018/05/ebola-vaccine-what-took-so-long/
[44] “Final trial results confirm Ebola vaccine provides high protection against disease,” The World Health Organisation, December 23, 2016, http://www.who.int/news-room/detail/23-12-2016-final-trial-results-confirm-ebola-vaccine-provides-high-protection-against-disease
[45] “G7 welcomes Gavi’s aim to reach 300 million more children with vaccines,” Gavi Vaccine Alliance, June 8, 2015, https://www.gavi.org/library/news/statements/2015/g7-welcomes-gavi-s-aim-to-reach-300-million-more-children-with-vaccines/
[46] Alexandra Sifferlin, “This New Group Wants to Stop Pandemics Before They Start,” Time Magazine, January 19, 2017, https://time.com/4639245/cepi-ebola-zika-epidemic/
[47] “List of Blueprint priority diseases,” The World Health Organization, 2018, https://www.who.int/blueprint/priority-diseases/en/
[48] “World Bank Launches First-Ever Pandemic Bonds to Support $500 Million Pandemic Emergency Financing Facility,” The World Bank, June 28, 2017, https://www.worldbank.org/en/news/press-release/2017/06/28/world-bank-launches-first-ever-pandemic-bonds-to-support-500-million-pandemic-emergency-financing-facility
[49] “Pandemic Emergency Financing Facility,” The World Bank, last modified July 27, 2017, http://www.worldbank.org/en/topic/pandemics/brief/pandemic-emergency-financing-facility
[50] “Pandemic Emergency Financing Facility (PEF) Operational Brief for Eligible Countries,” The World Bank, last modified December, 2017, http://pubdocs.worldbank.org/en/119961516647620597/PEF-Operational-Brief-Dec-2017.pdf
[51] “Ebola virus disease – Democratic Republic of the Congo,” The World Health Organization, last modified August 17, 2018, http://www.who.int/csr/don/17-august-2018-ebola-drc/en/
[52] “WHO supports Ebola vaccination of high risk populations in the Democratic Republic of the Congo,” The World Health Organization, May 21, 2018, https://www.who.int/news-room/detail/21-05-2018-who-supports-ebola-vaccination-of-high-risk-populations-in-the-democratic-republic-of-the-congo
[53] Laurie Garrett, “Ebola Is Back. And Trump Is Trying to Kill Funding for It,” Foreign Policy, May 9, 2018, https://foreignpolicy.com/2018/05/09/ebola-is-back-and-trump-is-trying-to-kill-funding-for-it/
[54] “Ebola vaccination begins in North Kivu,” The World Health Organization, August 8, 2018, https://www.who.int/news-room/detail/08-08-2018-ebola-vaccination-begins-in-north-kivu
[55] Jacqui Wise, “WHO is “cautiously optimistic” about Ebola ring vaccination programme in DRC,” British Medical Journal 361, (2018) https://doi.org/10.1136/bmj.k2388
[56] “Ebola outbreak in DRC ends: WHO calls for international efforts to stop other deadly outbreaks in the country,” The World Health Organization, July 24, 2018, https://www.who.int/news-room/detail/24-07-2018-ebola-outbreak-in-drc-ends–who-calls-for-international-efforts-to-stop-other-deadly-outbreaks-in-the-country
[57] Nadia Drake, “The world’s second-biggest Ebola outbreak is still raging. Here’s why,” The National Geographic, May 24, 2019, https://www.nationalgeographic.com/science/2019/04/worlds-second-biggest-ebola-outbreak-still-raging-heres-why-hot-zone/
[58] “Ebola virus disease – Republic of Uganda,” The World Health Organization, last modified June 13, 2019, https://www.who.int/csr/don/13-june-2019-ebola-uganda/en/
[59] “Ebola situation reports: Democratic Republic of the Congo,” The World Health Organization, last modified 2018, https://www.who.int/ebola/situation-reports/drc-2018/en/
[60] “Statement on the meeting of the International Health Regulations (2005) Emergency Committee for Ebola virus disease in the Democratic Republic of the Congo,” The World Health Organization, June 14, 2019.
[61] Nurith Aizenman. “Threats By Text, A Mob Outside The Door: What Health Workers Face In The Ebola Zone,” National Public Radio, May 10, 2019.
[62] “WHO flags critical funding gap, calls for political parties to join the fight against Ebola,” The World Health Organization, June 19, 2019.
[63] Ibid (68)
[64] “Global Health Data Exchange,” Institute of Health Metrics and Evaluation, last modified 2017.
[65] Olivier Telle, “Emerging infectious diseases in India: the scourge that could boost urban development,” The Conversation, April 18, 2018.
[66] Tanzin Dikid et al., “Emerging & re-emerging infections in India: an overview,” The Indian journal of medical research 138, no. 1, (2013).
[67] Rajeev Sadanadan et al., “Towards global health security: response to the May 2018 Nipah virus outbreak linked to Pteropus bats in Kerala, India,” BMJ Global Health 3, (2018).
[68] Ibid (75)
[69] “Could have been much worse: India stops deadly Nipah outbreak,” Healio, September 2018.
[70] “Nipah virus case confirmed by Kerala govt, 86 people under observation”, India Today, June 4, 2019.
[71] “Bihar encephalitis deaths reveal cracks in India healthcare”, BBC, June 25, 2019.
[72] “One Health”, The World Health Organization. Last modified September 2017.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Jessie Huang is an intern with the Observer Research Foundationoffice in Mumbai. She is a junior at Wellesley College near Boston MA
Read More +
Deepesh Vendoti is a former consultant at ORF-Mumbai's HealthInitiative. He is a medical doctor by training and a public healthmanagement graduate from Yale University.
Read More +