-
CENTRES
Progammes & Centres
Location
 PDF Download
PDF Download 
Sujay Santra, Tirumala Santra Mandal and Parswati Das, “Leveraging Disruptive Technology Innovations for Healthcare Delivery in Sub-Saharan Africa”, ORF Issue Brief No. 298, June 2019, Observer Research Foundation.
Introduction
The Alma Ata Declaration of 1978 recognised primary healthcare as the foundation of health systems in most of Sub-Saharan Africa (SSA). Following the Declaration, SSA restructured the entire health system within the framework of primary healthcare, instead of focusing solely on the first level of care.[3] However, primary-healthcare implementation has suffered obstacles due to political instability, structural changes, natural calamities and HIV/AIDS pandemics, impacting access to equitable and sustainable care and the health outcomes of the people.[4]
1. Insufficient access to primary care: Primary healthcare systems are governed by a set of policies regarding universal health coverage and primary care.[5] In SSA, only one-third of the region has access to affordable basic healthcare, and the workforce is a fraction of the total size required, causing multiple health challenges.[6] The subregion’s public agenda does not sufficiently include prevention and treatments. The region has experienced drastic changes in health and disease patterns, and has a high predominance of communicable diseases, non-communicable diseases, and infectious and parasite diseases.[7],[8],[9] While the public health system is crucial in addressing the healthcare gap, there has been little progress over the years, due to the continuation of colonial-era healthcare models that lack focus on disease prevention, promotion components, workforce training, strong supervision and managerial leadership.[10]
2. Shortage of health workforce: Community health workers form important linkages to essential life-saving healthcare intervention. SSA consists of 11 percent of the world’s population and bears 24 percent of the global disease burden, but it is home to only three percent of the global health workforce.[11] The World Health Organization (WHO) estimates that 57 countries worldwide face a critical shortage of health workers, out of which 36 countries are in SSA.[12],[13] The lack of health resources has negative implications on public health with respect to increased mortality rates, maternal and child health and the treatment of AIDS, which further limits the capacity of various interventions and the implementation of government health policies, given the scale of health workforce disparity.[14],[15]
Figure 1: Current Density of Physicians, Nurses and Midwives, and the Required Rate of Workforce Growth According to Population Growth Rates, in 12 African Countries[16]
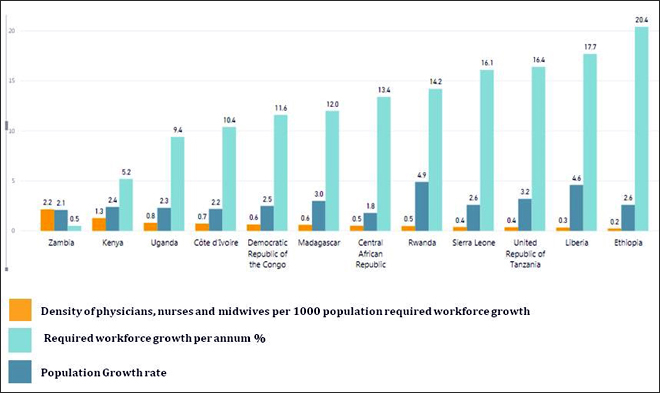
Source: WHO, 2009.
3. Information technology for clinical use: Harnessing the power of information technology can significantly improve the health system’s capacity to streamline patient database and provide better clinical care and drug management.[17] However, due to the disproportionate burden of diseases, SSA lags behind in the adoption of innovative technology. A study reported that the use of Electronic Health Records in SSA was recommended for the AIDS Relief HIV programme, but limited computer skills and human resources hindered proper implementation.[18],[19] So far, technology has remained confined to administrative and non-clinical usage.
The growth of private healthcare in Africa
The weak national health systems in Africa paved the way for private players to gain new footholds in the continent. In countries with limited public resources, 60 percent of the healthcare financing is dependent on private health services and 50 percent of the total expenditure goes to private health providers.[20] Most citizens—especially in rural communities— have been underserved by the public sector, creating opportunities for private players to fill the gap with high-quality, frequent services and advanced resources.
Renewed political stability, economic reforms and increasing average incomes have expanded the healthcare gap, creating greater demand for quality care. In 2001, Africa’s annual GDP growth was at five percent, faster than the global average of 4.2 percent, with SSA’s per capita growth exceeding five percent in the last five years.[21] This allowed for improved per-capita expenditure on healthcare goods and services. The highest share of investment has come from private healthcare sectors, such as medical product manufacturer, pharmaceutical, retail, insurance, medical education and technology-enabled healthcare initiatives.
India–Africa healthcare relations
India is SSA’s second-largest pharmaceutical trading partner, followed by China, which is growing at a rate of 6.4 percent of the total global trade.[22] Southern and Western Africa, in particular, are the largest importers of Indian pharmaceutical products. Indian manufacturers gain market share primarily through cost-effective pricing and by targeting different markets. For example, Ranbaxy, Cipla and Dr. Reddy have a strong presence in East Africa[23] and have gained competitive advantage over other global players in the region by integrating local talent in business operations and offering quality medicines certified by WHO.[24]
Before 2001, only one in a thousand had access to life-saving antiretroviral (ARV) medicines, critical for preventing the transmission of HIV/AIDS. During that time, the biggest pharmaceutical companies offered the medicine at a price point of US$10,000–15,000 per patient per year. Recognising the need for affordable medicines in the region, Indian pharmaceutical companies, such as Cipla, disrupted the market price to offer the drug at US$350 per person per year, and later, Mylan and Aurobindo reduced the cost to US$75 per person per year.[25]
Table 1: Key Pharmaceutical Companies in Sub-Saharan Africa
| Pharmaceutical Firms | Areas of Operation | Initiatives |
| Cipla Ltd. | Cameroon, Kenya, Lesotho, Zambia | Cipla’s “Dollar a Day” Treatment Programme offers triple-combination of “antiretroviral” AIDS drugs at US$350 per person per year, which is less than $1 a day per patient to provide critical medicines to poor nations at an affordable price. It has revolutionised the way AIDS drugs are offered in Africa. |
| Dr. Reddy’s Laboratories | South Africa | The pharma company is a wholly owned subsidiary and a leading generic player in South Africa and focuses on key therapeutic areas such as Central Nervous System (CNS) and Primary Care. The company commenced operations in the continent through Triomed. |
| Ranbaxy Laboratories | Operates in 52 countries in the African continent and the Middle East and is strengthening its manufacturing capacities in Nigeria | Ranbaxy Laboratories boosted its presence in the emerging market of Africa by introducing a new malaria-fighting drug, “Synriam,” and setting up manufacturing facilities in Morocco, Nigeria and South Africa. |
| IPCA Laboratories | Uganda, Ghana, Ivory Coast, Burkina Faso, Zimbabwe, Sudan, Tanzania, Kenya, Ethiopia and Nigeria | IPCA exports branded and generic formulations, as well as Active Pharmaceutical Ingredients (APIs). |
| Cadila Healthcare | South Africa | The company is amongst the top ten Indian private pharmaceutical companies operating in the African generic drugs market. Subsidiary companies of Cadila working in Africa include Simayla Pharmaceuticals (Pty) Ltd. (South Africa), Zydus Healthcare S.A. (Pty) Ltd. (South Africa), and Script Management Services (Pty) Ltd. (South Africa). |
| J.B. Chemicals and Pharmaceuticals Ltd. (JBCPL) | South Africa | Manufactures and markets a diverse range of pharmaceutical formulations, herbal remedies and APIs. |
| Lupin Ltd. | South Africa | The single-largest company in the cardiovascular segment. It is a major generic pharmaceutical player in South Africa. |
Source: RIS New Delhi, 2015.[26]
After 2001, several Indian pharmaceutical companies entered SSA’s healthcare market to ride its growth wave. It was evident that they would only be able to develop and expand in the continent through healthcare provider partnerships. For instance, in 2009, a CAD50-million equity fund made an investment in Nairobi, acquiring a stake in a women’s hospital,[27] and worked with local organisations to reach more patients to provide healthcare services and medicine supplements. An initiative in India implemented by Novartis, in partnership with local NGOs, earned increased demand for medicines by encouraging rural families to seek health advice.[28]
The expansion of SSA’s pharmaceutical market and the region’s improved average incomes enabled Indian healthcare partners to put down roots and offer cheaper healthcare compared to private African healthcare providers. Prior to this, Africa’s own health systems catered primarily to the affluent populations and restricted care to acute and short-term treatment.[29] A majority of African citizens—especially the poor and those in the middle-income bracket—relied on under-funded public health facilities, with only a small minority having access to well-funded, private health systems. Consequently, there was an urgent demand for improved access to primary healthcare. Indian health providers managed to fill this gap by providing treatments at lower costs and catering to a larger patient base, while also improving their profit margins.
Table 2 shows key Indian secondary and tertiary healthcare providers in SSA.
Table 2: Indian Private Healthcare Service Providers in SSA[30],[31]
| Company | Areas of Intervention | Domain |
| Aga Khan University Hospital | Nairobi | Due to increasingly frequent non-communicable illnesses, including cancer, they are looking to provide specialist care. |
| Medanta Africare | Kenya, Nairobi | Tertiary care |
| Fortis Healthcare | Uganda and Nigeria | Tertiary care |
| Agarwal’s Eye Hospitals | Mauritius , Ghana and Mozambique | Advanced diagnostics and eye-care treatment with optical facility |
| Apollo Healthcare | Nigeria, South Africa, Mauritius, Ethiopia, Tanzania and Zimbabwe | Tertiary care |
| Moolchand Healthcare | Nigeria, South Africa, Mauritius, Ethiopia, Tanzania and Zimbabwe | Tertiary care |
| IPE Africa | Kenya, Ethiopia, Tanzania, Rwanda, Somalia, Democratic Republic of Congo, Ghana and Zimbabwe | Focused on building local capacities, strengthening health systems |
Indian healthcare providers soon realised that specialised services are domain-specific and fail to cater to vulnerable populations. The private players were observed to work in silos and lacked integrated technology solutions, limiting their impact, scale and reach of service delivery to certain geographic regions. Further, the expansion and replication of Indian models for affordable delivery proved difficult in Africa for several reasons:
In light of these challenges, a model that combines the health workforce, technology innovations and health-reform integration can help the Indian health systems scale up more effectively in African countries.[35]
Healthcare delivery in SSA is uncoordinated, and hospitals and specialist care are accessible only to the affluent population due to high costs. There is a dearth of integrated primary healthcare delivery systems, which can act as the first point of access to medical care and, later, to secondary and tertiary care across the region. For instance, common illnesses can be managed at the primary level and complex disorders referred to specialists by the primary medical team, ensuring that patients receive the most appropriate care in a systematic manner. This coordinated continuum of care can help reduce the costs of secondary treatments and alleviate inequality and vulnerability.[36] Sub-Saharan African countries have now committed themselves to reviewing and updating their health policies to keep up with the regional goal of accomplishing health for all through the primary-healthcare model.[37]
Table 3: Health-Tech Companies Operating in Africa’s Primary Healthcare Domain
| Name of Organisation | Domain | Area | For Profit Model | Last Mile | Front line Health Workers | End-to-End Technology Integration | Innovative POC | Continuum of Care Backed by AI | Occasioning with Govt. |
| Living Goods[38] | Living Goods operates networks of independent entrepreneurs who make a living by selling medicines and products to poor people that can help improve their health, wealth and productivity. Plan to deploy thousands of digitally empowered CHWs to deliver quality care, door-to-door, at a fraction of the cost of training doctors or nurses. | Uganda and Kenya | Non-Profit Organisation | ☑ | ☑ | ☒ | ☒ | ☒ | ☑ |
| Last-Mile Health[39] | Supports the government to implement a nationwide community health-worker programme that will bring life-saving care to the doorsteps of people living in remote communities | Liberia | Non-Profit Organisation | ☑ | ☑ | ☒ | ☒ | ☒ | ☑ |
| BRAC[40] | Community-based Healthcare | Liberia, Uganda | Non-Profit | ☑ | ☑ | ☒ | ☒ | ☒ | ☑ |
| Medic Mobile[41] | Integrated community health systems that improve the quality, accessibility, speed, and equity of primary healthcare | Liberia, Uganda, Kenya, Ethiopia, Malawi | Non-Profit | ☑ | ☑ | ☑ | ☒ | ☒ | ☒ |
| Commcare-Dimagi[42] | A unique feature of ICT-enabled data collection is that data can be viewed and analysed in real time, so that care providers and policymakers can make life-saving decisions based on evidence | South Africa, Maputo, Mozambique, and Dakar, Senegal, Tanzania | For profit | ☑ | ☑ | ☑ | ☑ | ☒ | ☒ |
Indian healthcare start-ups in Africa
Extending the reach of primary care and renewing its framework requires a systemic approach on several fronts, including new delivery models; a greater role of private initiatives; and the introduction of digital technology to improve access to care and knowledge, and create collaborations between key stakeholders.[43]
Mobile phones have become increasingly common and can be used as important tools in delivering better health outcomes. Entrepreneurial ventures with technology solutions are emerging to connect the healthcare gaps in the continent.[44] While many of these ventures are in their nascent stages, they are already creating a significant impact in African communities. For example, a longitudinal study conducted by a start-up venture called “Healthy Entrepreneur” in Kenya, in association with Erasmus University Rotterdam, observed significant improvement in knowledge and access to basic care delivered through entrepreneurial initiatives, compared to non-entrepreneurs. The study demonstrated a 52-percent increase in knowledge, 80-percent increase in access to essential health products and generic drugs, and 17–25-percent reduction in overall market price. The study also showed that entrepreneurial initiatives provide more reliable services to the community while still generating profit. They spend more time in community work and increasing the population’s self-esteem.
While technology penetration has picked up rapidly, the continent is yet to establish e-health programmes.[45] However, the study finds that SSA is open to mainstreaming e-health as a major component of its health strategy. Recently, multiple m-health interventions have been pilot tested in the continent across various fields, such as maternal and child health intervention, telemedicine, remote consultations, referrals, supply-chain management, and technology-enabled health workforce.
Despite the immense opportunity that SSA presents for health-tech companies, however, prominent Indian health-tech players are still few and far between.
Bharti Airtel Limited is an Indian global telecommunications services company, and it is Africa’s largest mobile carrier. The Malawi Ministry of Health has discovered an innovative way to provide important healthcare services to rural people through the use of text messages called “health centres by phone.” A mobile handset becomes a clinic that transmits information to patients without them having to visit a clinic. The text message service also provides medical tips, recommendations and reminders about medications, allowing patients to connect with doctors anytime, anywhere. The toll-free service line has provided prenatal and postnatal information to five million pregnant women, new mothers and children, as well as encouraged the use of mosquito repellents to prevent malaria. The service is based on the public–private partnership between the Ministry and Airtel, providing critical support, accessibility, sustainability and successful integration and diversification of content and services at the community level.[46],[47]
Figure 2: Mobile-phone Subscriber Penetration in SSA[48]
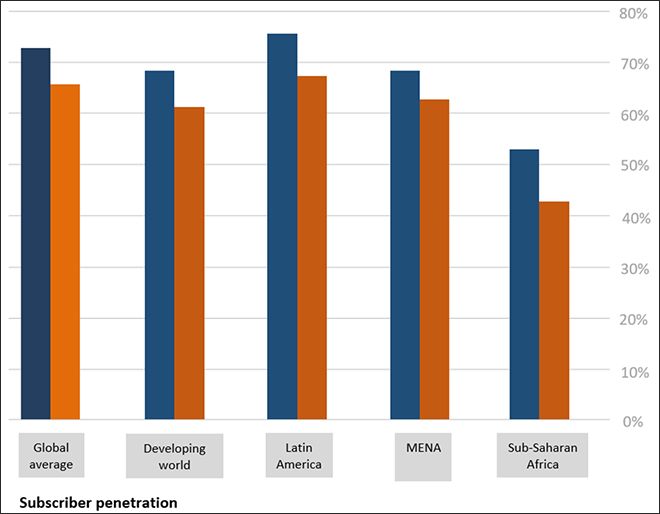
Source: GSMA Mobile Economy 2018, Sub-Saharan Africa, 2018.
Challenges: The mobile market in SSA has expanded considerably in urban areas, but coverage and adoption are still low in rural regions. The operators experience high-cost pressure in entering the market, since the economics of rollout in low-income regions is challenging. It is important to formulate investment-friendly policies that allow operators to connect the unconnected and bring about sustained improvement in health and economic outcomes in the region.[49]
Dure Technology, in collaboration with community organisations, has developed the first community app for tuberculosis (TB). The app empowers communities to collect, analyse, understand and communicate key information about the responses at the local level with respect to the availability and quality of services, barriers to accessing these services and other inequalities. Community actors report the information generated to the local- and national-level programme management units which, in turn, work on improving services and access to quality care. With offices in both Switzerland and India, the venture offers innovative technology products and solutions for public health and the social-development sector. Dure Technology is a dynamic venture that explores practical solutions to improve people’s lives by closely working with the UN organisations, international organisations and government bodies across several countries in Asia, Africa and Europe.
Challenges: The current investment in TB research is inadequate to sustain the pipeline of discovery in the region.[50]
The dearth of doctors and skilled manpower, coupled with the high burden of diseases, fuels the need for teleradiology services in Africa. A venture named ‘Teleradiology Solutions’ tapped this growing opportunity using its proprietary technology “RadSpa.” The technology allows doctors to receive radiology images and revert with diagnostic options from hospitals in areas with low internet bandwidth. The extensive experience garnered in the far-flung areas of Asia helped the venture implement the model in Africa. It also provides Continuing Medical Education Programmes for radiologists and doctors, to improve their knowledge of the latest advances in the medical field in Africa. The Bengaluru-based company has served 1.90 lakh cases and has expanded its presence in nine African countries, namely Ethiopia, Uganda, Zimbabwe, Djibouti, Botswana, Nigeria, Cameroon, Tanzania and Zambia.[51]
Challenges: One of the biggest challenges to the implementation of teleradiology in Africa is low internet bandwidth and high costs. However, the market is expected to improve in a couple of years as Africa gets better bandwidth.[52]
Metropolis is a Mumbai-based company with more than 85 diagnostic centres and 600 sample collection centres across South Asia, West Asia and Africa. It is based on a hub-and-spoke model, where each of the labs connects with 10 collection centres within a specified area. Its healthcare providers conduct trainings for medical professionals to address the skills and training gaps in Africa.
Challenges: The cost of healthcare professionals in Africa is higher than in India. According to the Kenya Nurses Union statistics, the average salary of Kenyan nurses is about US$400 a month, while the average salary of Indian nurses is in the range of US$36–88 per month. The shortage of medical practitioners and the lack of government focus on healthcare is a major challenge in the region.[53]
iKure is an India-based public healthcare start-up, delivering technology-enabled integrated primary care across 840 million rural populations. Backed by disruptive technology innovations, an empowered health workforce and a collaborative partnership ecosystem, the venture has treated eight million beneficiaries, trained 550 community health workers, and reached 3,200 villages in India. iKure’s cloud-based technology platform, called WHIMS, enables access to affordable and quality care, health information and seamless communication between patients and healthcare providers. With newer technological capability, the venture is working towards automating business operations, streamlining workflow and upskilling the health workforce to meet the needs of the beneficiaries more holistically.[54]
In Kenya’s Homa Bay area and Uganda’s Mityana and Mukono, 70–80 percent of the populations live in rural villages. These areas have high maternal and infant mortality rates, foetal deaths caused by preventable diseases, and lifelong disabilities due to poor access to healthcare, sanitation, nutrition and hygiene information. Given the similar nature of challenges in Indian and African rural communities, iKure ventured in the region to offer technology-integrated solutions in association with the local partner. Some key approaches are listed below:
The following are some of iKure’s key impacts in SSA:
Challenges: The healthcare market catering to vulnerable populations in rural areas is inundated with traditional healers, individual medicine sellers and different sources of care, especially for the poor and marginalised communities. Lack of education and awareness about high-quality providers is a challenge for iKure, making it heavily dependent on unregulated medicines and services. Poor infrastructure for cybersecurity regulators and privacy regulators to govern the sharing of health data is also a challenge for digital start-ups in the region.
While the Indian government is supportive of start-up ecosystems, African countries rank low on the World Bank’s “Ease of Doing Business Index.” Start-ups face the challenges of complex regulations, as well as ever-changing political and trading laws in the region.[55] Further, monetary transaction across the continent is difficult due to high bank charges, and availing services through Western Union hikes costs by 15 percent. Financial companies such as FinTech money transfer can be set up to help the situation.
Conclusion
While issues about expansion and acceptance from private healthcare organisations will continue to exist, the sheer size of SSA’s health challenges makes it necessary to involve the government in improving the population’s health and quality of life. Enterprises that focus on technology solutions are working to fill the gaps in healthcare delivery in the region. Start-ups such as iKure, for example, are able to offer a more holistic, multisectoral approach to serving the underserved population. For this reason, these ventures are finding considerable measures of success in the SSA region.
At this crucial juncture, it is important for start-ups to identify the ground challenges—e.g. varying consumers’ insights, regulations and market forces—that can affect returns as well as sustainable results. Being open to working across the diversified spectrum of health determinants will help technology start-ups deliver effective healthcare solutions in Sub-Saharan Africa.
Endnotes
[1] “The Business of Health in Africa: Partnering with the Private Sector to Improve People’s Lives (English)” International Finance Corporation, World Bank, Washington, D.C., 2008, accessed 2 April 2019.
[2] “Why the Workforce is Important”, World Health Organisation, 2006.
[3] Olujide O. Arije, “Quality in Primary Health Care Services in Sub-Sahara Africa: Right or Privilege?” Journal of Community Medicine and Primary Health Care 28, no. 1 (2016): 25–30, accessed 2 April 2019.
[4] Rufaro R. Chatora and P. Tumusiime, “Primary Healthcare: A Review of Its Implementation in Sub-Saharan Africa,” Primary Health Care Research and Development 5 (2004): 296–306, accessed 2 April 2019.
[5] “A VISION FOR PRIMARY HEALTH CARE IN THE 21ST CENTURY: Towards Universal Health Coverage and the Sustainable Development Goals” World Health Organisation and the United Nations Children’s Fund, 2018, accessed 2 April 2019.
[6] L. Chen, T. Evans, S. Anand, Jo I. Boufford, H. Brown, M. Chowdhury, et al., “Human Resources for Health: Overcoming the Crisis,” Lancet 364, no. 9449 (2004): 1984–990, doi: 10.1016/S0140-6736(04)17482-5pmid: 15567015.
[7] A. Boutayeb, “The Double Burden of Communicable and Non-communicable Diseases in Developing Countries”, Transactions of the Royal Society of Tropical Medicine and Hygiene 100, no.3 (2006): 191–99, accessed 2 April 2019, doi:.
[8] “The Global Burden of Disease: Main Findings for Sub-Saharan Africa”, World Health Report, 2013.
[9] G.A. Mensah, “A Heart-healthy and "Stroke-free” World through Policy Development, Systems Change, and Environmental Supports: A 2020 Vision for Sub-Saharan Africa,” Ethnicity and Disease 13 (2003): S4–12.
[10] R.O. Chimezie, “Failure of Primary Healthcare Delivery in Africa,” International Journal of Interdisciplinary and Multidisciplinary Studies 2, no. 4 (2015): 208–15, accessed 2 April 2019, doi: 10.2471/BLT.07.049239.
[11] “The Business of Health in Africa,” World Bank, 2008.
[12] Ibid., 98.
[13] “Working Together for Health”, The World Health Report, 2006.
[14] R. Mash, A. Howe, O. Olayemi, et al., “Reflections on Family Medicine and Primary Healthcare in Sub-Saharan Africa,” BMJ Global Health 3 (2018), doi:10.1136/ bmjgh-2017-000662.
[15] Oathokwa Nkomazana, Robert Mash, Silvia Wojczewski, Ruth Kutalek, Nthabiseng Phaladze, “How to Create More Supportive Supervision for Primary Healthcare: Lessons from Ngamiland District of Botswana: Co-operative Inquiry Group”, Global Health Action 9, no. 1 (2016).
[16] “The Health Worker Shortage in Africa: Are Enough Physicians and Nurses being Trained?” World Health Organisation, 2009, accessed 29 March 2019.
[17] Meera Shekar and Kate Otto, “ICTs for Health in Africa”, World Bank, 2014.
[18] Paula Braitstein, Robert M. Einterz, et al., “‘Talkin' About a Revolution’: How Electronic Health Records Can Facilitate the Scale-Up of HIV Care and Treatment and Catalyze Primary Care in Resource-Constrained Settings,” Journal of Acquired Immune Deficiency Syndromes 52, no. 1 (2009): S54–7, doi:0.1097/QAI.0b013e3181bbcb67.
[19] F. Odekunle, R. Odekunle, S. Srinivasan, “Why Sub-Saharan Africa Lags in Electronic Health Record (EHR) Adoption and Possible Strategies to Increase EHR Adoption in This Region,” International Journal of Health Sciences and Research 7 (2017): 282–90.
[20] “The Business of Health in Africa,” op. cit.
[21] Ibid., 13.
[22] Natalie Emery, Siddharth Dixit and Chinmoy Kumar, “Is Trade with India Changing Africa’s Healthcare Landscape?” Brookings, 1 March 2019, accessed 28 March 2019.
[23] T.C. James, P. Shaw, P. Chatterjee, D. Bhatia, “India–Africa Partnership in Healthcare: Accomplishments and Prospects,” RIS New Delhi, 2015.
[24] “Africa: A Ripe Opportunity”, White Paper Africa, IMS Health, 2014, accessed 28 March 2019.
[25] Natalie Emery, Siddharth Dixit and Chinmoy Kumar, op. cit.
[26] T.C. James, P. Shaw, P. Chatterjee, D. Bhatia, op. cit.
[27] “Africa: A Ripe Opportunity,” op. cit.
[28] “Africa Rise Focusing on Patients, Fueling Growth”, Novartis in Africa.
[29] "The Future of Healthcare in Africa", The Economist Intelligence Unit Limited, The Economist, 2012, accessed 2 April 2019.
[30] S. Gebre and H. Nyambura-Mwaura, “India Health-Care Providers Look to Tap Africa ‘Growth Wave’”, Bloomberg Quint, 28 November 2016, accessed 2 April 2019.
[31] "Why IPE Africa", IPE Africa, accessed 2 April 2019.
[32] S. Gebre and H. Nyambura-Mwaura, op. cit.
[33] Ibid.
[34] Ibid.
[35] T. Knapp, B. Richardson and S. Viranna, “Three Practical Steps to Better Health for Africans” McKinsey Quaterly, June 2010, accessed 2 April 2019.
[36] Jan De Maeseneer and Maaike Flinkenflögel, “Primary Health Care in Africa: Do Family Physicians Fit In?” The British Journal of General Practice: The Journal of the Royal College of General Practitioners 60, no. 573 (2010): 286–92, doi:10.3399/bjgp10X483977.
[37] Rufaro R. Chatora and P. Tumusiime, op. cit.
[38] “LIVING GOODS + LAST MILE HEALTH”, LivingGoods, accessed 4 June 2019.
[39] "We Save Lives in the World's Most Remote Communities", Last Mile Health, accessed 4 June 2019.
[40] "Raising Awareness for Healthier Life", Brac, accessed 4 June 2019.
[41] “ABOUT US”, Medic Mobile, accessed 4 June 2019.
[42] “Build A Smarter Data Collection App”, Dimagi, accessed 4 June 2019.
[43] T. Knapp, B. Richardson and S. Viranna, op. cit.
[44] J. Jimenez, “Three Ways to Improve Healthcare in Africa”, World Economic Forum, 21 January 2015, accessed 28 March 2019.
[45] “Global Diffusion of eHealth: Making Universal Health Coverage Achievable”, World Health Organisation, 2016.
[46] K. OYARO, “Taking Health Services to Remote Areas: Mobile Camel Clinics, Motorbike Ambulances and Other Innovations for Reaching Rural Folk,” Africa Renewal, December 2016–March 2017.
[47] “Chipatala Cha Pa Foni: Health Center by Phone”, Village Reach Blog, 17 November 2014, accessed 29 March 2019.
[48] “GSMA Mobile Economy 2018: Sub-Saharan Africa 2018”, The Mobile Economy, accessed 29 March 2019.
[49] Ibid.
[50] "Dure Technologies Pvt Ltd: Delivering Accurate Real-time Data Applications for Healthcare Programs”, CIO Review India, accessed 29 March 2019.
[51] Nandita Vijay, “Doctor Shortfall in Africa Propels Demand for Teleradiology Expertise: Dr. Arjun Kalyanpur”, Pharmabiz, 30 November 2016, accessed 29 March 2019.
[52] “TELERADIOLOGY IN AFRICA - HOW IT BENEFITS PATIENTS”, Teleradiology Blog, 28 August 2017, accessed 4 June 2019.
[53] “Metropolis Healthcare Plans Buyouts in African Markets”, Business Standard, 8 May 2013, accessed 4 June 2019.
[54] Abram Wagner Abram, Lu Xia, Priyamvada Pandey, Sandip Datta, et al., “Risk Factors During Pregnancy and Early Childhood in Rural West Bengal, India: A Feasibility Study Implemented via Trained Community Health Workers Using Mobile Data Collection Devices,” Maternal and Child Health Journal 22, no. 9 (2018): 1286–296, doi: 10.1007/s10995-018-2509-y.
[55] “EASE OF DOING BUSINESS IN Malawi”, World Bank, accessed 29 March 2019.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Sujay Santra is Founder &: CEO of iKure Techsoft Pvt. Ltd. He was among the 100 most impactful healthcare leaders recognised by the World Health ...
Read More +
TirumalaSantra Mandal PhD is a Senior Research and Communication Analyst at iKure. She has authored and edited publications for various peer-reviewed journals. ...
Read More +
Parswati Das is Programme Manager at iKure. She has workedin Technology Business Incubation NSTEDB DST Government of India as well as various state government projects.
Read More +