Abstract
Even as India achieved statistical elimination of leprosy at the national level in 2005, the target continues to be part of the country’s policy documents. But what is “elimination”, to begin with? The policy documents are unclear of its operational definition, of whether it is at the national level, the state level or the district level. Despite lack of clarity, the political leadership has not failed to indulge in the rhetoric of “leprosy elimination”. In 2018, India was supposed to have achieved national level elimination—yet again. This paper argues that these declarations are devoid of any positive public health significance, and the country is a long way from eliminating leprosy at the state or district levels. As witnessed in 2005, the declaration only served to make officials complacent, shifting resources away from the programme itself. Meanwhile, the data show worrying new trends: Leprosy is becoming highly concentrated amongst the Adivasis (Scheduled Tribes); and the number and proportion of states and districts with elimination-level prevalence is fast decreasing. The paper makes a case for Ayushman Bharat to be the opportunity for streamlining case detection and treatment.
(Author’s note: I would like to acknowledge two anonymous referees for their valuable inputs on an early draft of this paper; Vinia Datinguinoo Mukherjee for making the paper readable; and Vasundhara Singh for her assistance with the referencing.)
Introduction
Current evidence shows that India has managed to improve population health at a considerable rate despite very low per-capita public spending. However, India’s health sector is also known for finding statistical targets that are either already achieved or easily achievable—and later declaring with fanfare that they have been “achieved”. The National Health Policy 2017 (NHP), for example, contained targets that have been described as spectacularly unambitious, including one on increasing life expectancy from 67.5 (2011[i]) to 70 by 2025.[ii] What NHP did not disclose—and the media did not discuss—was the fact that Indian women already achieved it in 2013, and that India has possibly crossed this milestone in 2018, given the rate of progress over the last decades.[iii] India’s recent achievement of the Maternal Mortality Ratio (MMR) target set out in the Millennium Development Goals (MDG) is another case in point. The Ministry of Health, disagreeing with the Ministry of Statistics, opted to cherry-pick the MMR baseline (1990) number from an international estimate and conveniently ignored the endline (2015) number—comparable with the baseline[iv]—from the same source. The choice of a higher number in the baseline made the fall in MMR look steeper than it actually was. The endline estimate based on the Sample Registration Survey (SRS) was selectively used despite the fact that the MMR estimates in the SRS have been regularly upwardly revised by the same international source.[v]
Such selectivity has also been seen with leprosy, with the NHP’s (2017) inclusion of a target of achieving and maintaining “elimination” status by 2018.[vi] Data journalism portal Fact Checker correctly identified this as a re-packaged target from the NHP 2002, and noted: “The 2002 NHP had set the target of eliminating leprosy by 2005, kala azar by 2010 and lymphatic filariasis by 2015–none of which could be achieved yet.”[vii] What Fact Checker failed to note was that the leprosy elimination target was indeed achieved in 2005, as per plans, when the prevalence rate came down to under one per 10,000 population.[viii]
Perhaps because of its inclusion in NHP, and partly due to the confusion between “elimination” (a target defined by the World Health Organization as prevalence level of less than one in 10,000 population) and “eradication” (zero new cases)— “elimination of leprosy” remains a favourite topic of senior ministers. From Prime Minister Narendra Modi,[ix] to Finance Minister Arun Jaitley in his 2017 Budget Speech, officials have repeatedly called for the elimination of leprosy.[x] Indeed, Health Minister Jagat Prakash Nadda declared in June 2018 that India would eliminate leprosy that year.[xi] Not to be outdone, the flagship annual publication of the Ministry of Health and Family Welfare, the Annual Health Profile of India (2018) states that leprosy has been “nearly” eliminated—this, despite the fact that elimination happened more than a decade ago.[xii] Latest reports indicate that the elimination target has been further pushed by the Ministry of Health to 2019.[xiii]
Official data show that the number of new leprosy cases detected during 2016-17 is 135,485 and the prevalence rate per 10,000 population as of March 2017 is 0.66. It is established, however, that these numbers underestimate the real leprosy burden. The Health Minister himself is on record saying that there may be 250,000 new leprosy cases every year, based on a sample survey by the Indian Council of Medical Research (ICMR), a government agency, in 2010-2011.[xiv] Interestingly, the results of this pan-India survey have not yet been released to the public. [xv]
To be sure, the issues surrounding leprosy in India involve not only the contradictory numbers. Equally importantly, India is also known to have passed laws that discriminate against persons with leprosy. One of the oldest, British-era laws (The Lepers Act of 1898)—which sanctioned the arrest and segregation of persons affected by leprosy into asylums—was repealed only as recently as in May 2016 by the current government.[xvi] Before the national-level abrogation, even though 12 states and five union territories had abandoned its application within their jurisdictions, the law continued to be in force in the rest of the country.[xvii] Further, it was only in 2015 when the use of the term “leper” was noted by the Law Commission of India to be derogatory. The Commission said Language was a medium that perpetuates existing stigmas, hampers efforts for the inclusion of Persons affected by leprosy into mainstream society, and affects their sense of dignity. The Commission recommended to replace the term “leper” and other such synonymous terms in national, regional or local languages in all government and private documents, to “persons affected by leprosy” or a similar term to that effect.[xviii]
Despite these orders, however, things have hardly changed. The Rajasthan Panchayati Raj Act, which was passed as late as 1994, states that a person is ineligible to contest local elections if s/he is a “leper or is suffering from any other bodily or mental defect or disease rendering him incapable for work.” Even prominent national newspapers carry headlines such as “Pune hospital admits a family of lepers as number of new cases rises”.[xix] In January 2019, Lok Sabha Passed the Personal Laws (Amendment Bill) 2019 to remove leprosy as valid ground for divorce.[xx]
The Burden of Leprosy in India
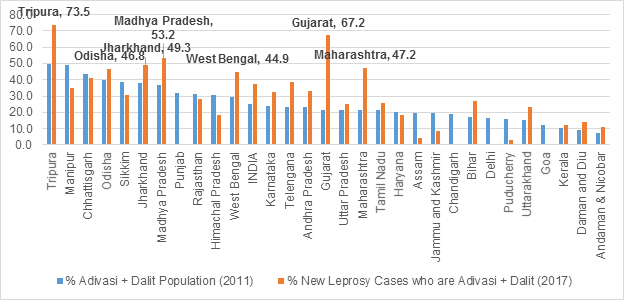
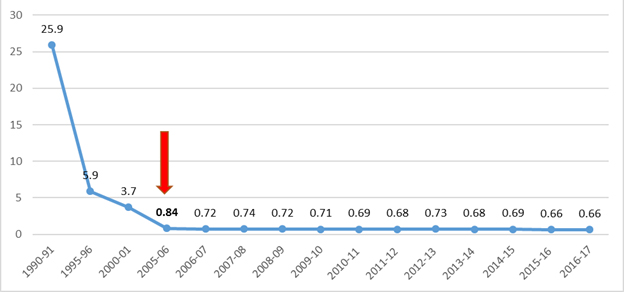
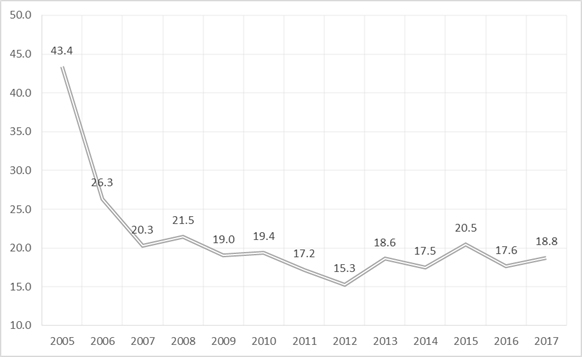
India has had major advances in battling leprosy. Graph 1 shows the country’s success in bringing down prevalence of leprosy over the last three decades. Internationally, the prevalence rate was brought under one per 10,000 population by 2000, and there was pressure on most endemic countries (such as India) to achieve the same at the national level at least by 2005, marking a significant milestone in the elimination of leprosy as a public health problem.[xxi] The current global prevalence is estimated by the World Health Organization (WHO) to be 0.23 per 10,000 population. In 2017, India along with Brazil and Indonesia were the only countries where more than 10,000 new cases were reported per year. For 2017, 135,485 out of the 204,686 new leprosy cases detected globally were in India – a staggering 66 percent. In other words, two out of every three new global leprosy cases are detected in India.[xxii]
Graph 1: Leprosy Prevalence Rate (per 10000) in India
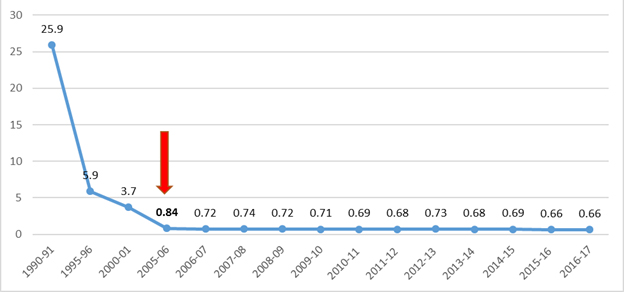
Source: http://nlep.nic.in
WHO reports that the India National Leprosy Eradication Programme (NLEP) carried out an innovative Leprosy Case Detection Campaign (LCDC), which resulted in the detection of 34,000 new cases in 2016-17 from high endemic pockets. These cases accounted for 25 percent of new cases detected by the national programme.[xxiii] While these new detections are remarkable, India needs to bring down the prevalence rate further in order for the world to achieve overall progress, given its extreme case-load when compared to other countries. Unfortunately, as Graph 1 demonstrates, the rapid rates of reduction through the 1990s have slowed down, and the prevalence rates have plateaued. It is noteworthy that the prevalence rate plateaued around the time of the declaration of “Leprosy Elimination” in 2005.
Even though India has not been able to achieve elimination targets at the state and UT levels, the 12th Five-Year Plan set out to achieve elimination of leprosy at the district level by 2017.[xxiv] However, with NHP 2017, the country has regressed to a (re)elimination of leprosy at the national level itself. It is highly unlikely that state-level elimination can be achieved any time soon. In fact, although all States and UTs, barring Chhattisgarh and Dadra & Nagar Haveli, had achieved elimination by 2016, partly due to new case detection campaigns, five more States/UTs (Odisha, Bihar, Chandigarh, Goa and Lakshadweep) have reported a prevalence rate of higher than one per 10,000 population in 2017.[xxv] Given that the government has re-started active surveillance in most parts of the country, the proportion of such states is bound to increase in the short or medium run.
Another major concern is the proportion of children among new leprosy cases. While the proportion of child cases in 2017 was 8.7 percent at the national level, it is more than 10 percent in 10 States/UTs across the country: Arunachal Pradesh (10.71 percent); Bihar (13.70 percent); Jharkhand (10.59 percent); Maharashtra (10.18 percent); Nagaland (11.76 percent); Punjab (17.25 percent); Tamil Nadu (17.64 percent); D&N Haveli (19.79 percent); Daman & Diu (14.29 percent); and Lakshadweep (11.11 percent).[xxvi] As surveillance efforts improve, the number might even increase further.
The numbers are not the only hurdle. Leprosy continues to carry a heavy stigma in popular imagination, even among policymaking circles and medical professionals, in particular the first-liners in managing the disease. It is seen as an illness that affects people only in the “far away corners” of the country. In an editorial for the Journal of Preventive and Social Medicine, Mishra and Gupta (2010) observed that it is quite common amongst doctors to display reluctance in joining government’s leprosy programme. It is considered as a “punishment posting”; those who join are often stigmatised by their own peers.[xxvii]
Bringing up another obstacle is the fact that patients often seek care in alternative systems of medicine. Researchers have found the use of alternative systems of medicine to be a risk factor for delay in diagnosis,[xxviii] and therefore practitioners of modern medicine see homeopaths as a hurdle to the success of NLEP.[xxix] At the same time, studies have highlighted the need to engage with traditional and alternative practitioners to promote early referral to specialist centres where patients can be diagnosed and appropriately treated.[xxx] It is worth mentioning here that NLEP is still exploring, through an expert committee, the use of homeopathic medicine in the treatment of tropic ulcers in leprosy.[xxxi]
Recommendations
With pockets of high endemicity across the country, India needs to pay attention to leprosy which, on paper, is no longer a “public health problem” after the 2005 declaration of elimination. As some 150,000 Health and Wellness Centres are being built across the country under the Ayushman Bharat initiative,[xxxii] which will offer screening for leprosy among other diseases, India has a chance to find patients from areas previously not covered by NLEP, and treat them effectively. Learning the lessons of past and present mistakes, India has three imperatives:
1) Make sure that declarations of Elimination do not take away from the attention needed to eliminate the disease at the state and district levels.
With two out of every three new global leprosy cases being detected in India, the country has remained a key component of WHO’s leprosy goal-setting plans over the decades. Global targets are inarguably dependent on India’s achievements. Knowing this, however, India often tends to overplay its successes and underplay its failures.
It was declared in 2005 with much fanfare that leprosy was officially eliminated as a public health problem in India, but not many seemed to know what the term “elimination” meant. While WHO used elimination as an interim goal to create interest in the neglected disease and raise funds globally, experts maintain that the meaning of this milestone was not clearly communicated to political leaders.[xxxiii] The same remains the case with the media. Even today, both Indian as well as international media often cover the issue while using “leprosy free” as a synonym for “elimination”.[xxxiv]
This has not been without serious implications. The declaration of 2005 halted progress of the national programme for leprosy, allowing the disease to spread again, according to senior bureaucrats of the Ministry of Health themselves. The focus of the programme got diverted as both funding as well as resources fell and frontline health workers stopped making household visits to identify undetected cases. The post-elimination era saw a dependence on “passive detection” whereby patients voluntarily came forward to report disease; this resulted in keeping the true extent of the problem subterranean.[xxxv] Even as part of the new surge in numbers could be a result of active surveillance in far-flung areas which were earlier untouched by the health system, part of the explanation of the persisting burden of leprosy could indeed be the shift away from programmatic focus on the disease post-2005, as suspected.
Research by Chaptini and Marshman (2015) has shown that it was the pressure on the remaining countries to meet the elimination target by 2005, which resulted in India officially meeting the target. However, independent assessments revealed many undiagnosed patients, and even found that active measures were adopted to ensure fewer patients were registered, including not registering single lesion cases and not tracing contacts. Between 2004 and 2007, new case detection dropped by 75 percent, partly the result of a decreased incentive within the system to find new cases.[xxxvi] The fact that India had failed to meet the original year 2000 target of elimination and it needed to be moved to 2005 complicated it further, putting immense pressure on the disease programme to “perform”.
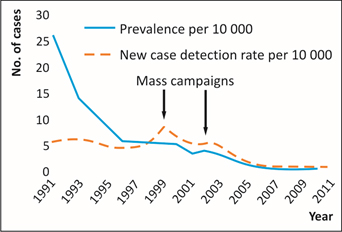
Graph 2 shows the impact of previous mass campaigns on case detections. The 2005 declaration of elimination of leprosy had a dampening effect on new case detections as evident from the graph. As discussed earlier, a rigorous Leprosy Case Detection Campaign (LCDC) campaign is now ongoing, which has the potential of finding cases that have remained hidden so far, due to the voluntary reporting phase. It is necessary to learn lessons from the 2005 experience and avoid creating an environment of complacency by making shallow declarations of India eliminating leprosy in 2018—or 2019 for that matter—and India becoming “leprosy free”.
Graph 2: Incidence and prevalence of leprosy in India, 1991- 2011
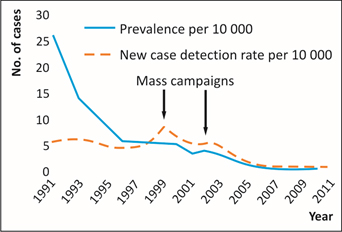
Source: Lockwood, Diana NJ, Vanaja Shetty, and Gerson Oliveira Penna. “Hazards of setting targets to eliminate disease: lessons from the leprosy elimination campaign.” BMJ 348 (2014): g1136.
State-level officials today admit that the 2005 declaration was “a mistake”. Dr Pradip Gaikwad from Maharashtra, for example, calls the declaration of elimination “false relief”, and observes that other diseases took priority in public health circles, resulting in the calling off of door-to-door visits in remote villages and the reassignment of medical personnel. Under-reporting of the disease and shortage of medicines caused by inadequate funding worsened the situation. In the context of under-reporting, the fact that there is vociferous talk of eradication (i.e., no new cases) ensured that there is no incentive to find new cases.[xxxvii]
After achieving statistical elimination of leprosy in 2005 as a public health problem with a national prevalence rate of 0.96, India integrated leprosy services with the primary health care delivery system, from the erstwhile programme-based vertical system.[xxxviii] However, the integration has remained on paper, as India still has hundreds of “Leprosy Colonies”,[xxxix] a practice that was eliminated by countries like Brazil back in the 1970s, along with integrating leprosy services into primary care.[xl]
In an era where political commitment to leprosy is lost, and funding as well as leprosy agencies are on the decline, research (Lockwood et al (2014) ) shows that the rhetoric of elimination has discouraged dermatologists from engaging with leprosy programmes, even though they may be diagnosing cases in the private sector, because they believe leprosy is already eliminated.[xli] In 2007, WHO abandoned the elimination target for leprosy programme and instead set a target based on disability rates with the aim of improving focus on prevention of disability.[xlii] In the same year, Fine (2007) noted in the Bulletin of the World Health Organization that neither funders nor young researchers are attracted to an officially “eliminated” disease — even if it is still ubiquitous. Interestingly, India’s declaration of leprosy elimination also coincided with the main leprosy journal of the previous 70 years (the International Journal of Leprosy) folding up. [xliii]
Thankfully, as part of Ayushman Bharat, India is planning to start a substantial number of (150,000) Health and Wellness Centres across the country to strengthen the primary level care infrastructure. These centres will be instrumental in offering universal screening of leprosy, giving India a historic opportunity to detect all cases and get closer to finally eradicating the disease.[xliv] It is clear that if Ayushman Bharat is to be a game-changer in leprosy, officials must stop engaging in the false rhetoric of India achieving elimination, unless the country achieves district-level elimination.
2) Initiate immediate remedial measures so that leprosy does not remain a stark indicator of India’s social inequities in health.
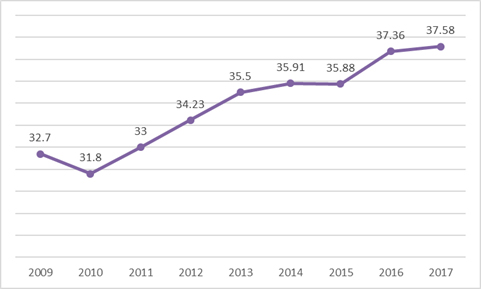
A distinct trend that should worry health policymakers in the country is that leprosy is becoming even more of a disease of the most marginalised and underserved populations in far-flung areas. There is some data on the prevalence of leprosy amongst the Dalits (Scheduled Castes) and Adivasis (Scheduled Tribes) who, according to Census 2011, constitute 16.6 percent and 8.6 percent of the Indian population, respectively. However, as Graph 3 shows, of the percentage of new leprosy cases in India, patients belonging to these two communities constitute 37.6 percent which is much higher than their proportion in the population. The proportion is increasing further.
Graph 3: Proportion of Dalits and Adivasis among new leprosy cases in India
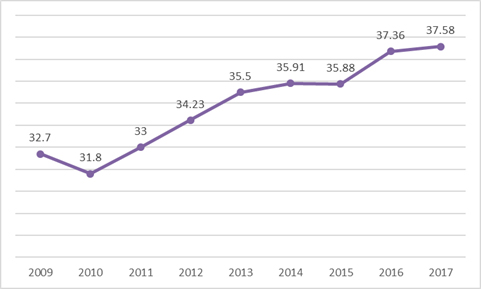
Source: http://www.nlep.nic.in/data.html
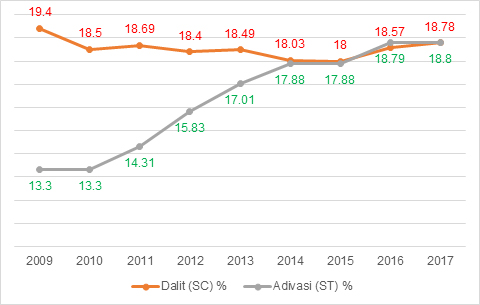
A look at disaggregated data shows that while the proportion of Dalits within new leprosy cases has been constant between 18-19 percent over the last decade, the overall rise is almost exclusively because of the rise in the proportion of Adivasis within new leprosy cases over the last decade. As Graph 4 shows, the increase in the proportion of cases from Adivasis has been considerable and persistent. From 13.3 percent in 2009, it has increased to an alarming 18.8 percent, and given that Adivasis are only 8.6 percent of the Indian population, it is a cause for major concern.
Graph 4: Proportion of Dalits and Adivasis among new leprosy cases in India
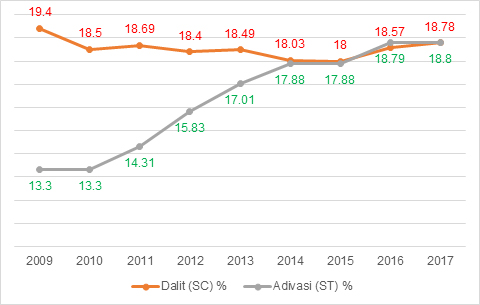
Source: http://www.nlep.nic.in/data.html
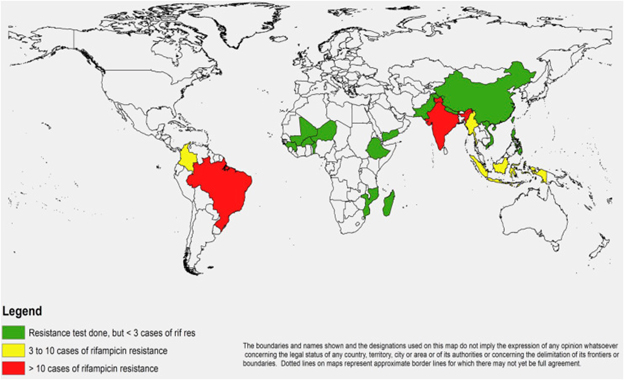
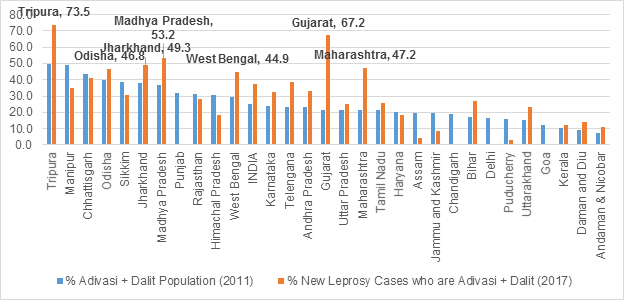
State-level official data paints an even more distressing picture. When states and Union Territories with a proportion of more than 50 percent of Dalit and Adivasi population are excluded from the analysis of new leprosy cases in 2017, a stark picture emerges from across the country. As shown in Graph 5, in Tripura, for instance, three out of every four new leprosy patients in 2017 belonged to either Adivasi or Dalit Communities. In Gujarat, two out of every three new leprosy patients belonged to either Adivasi or Dalit Communities, and in states like Odisha, Madhya Pradesh, Maharashtra, West Bengal and Jharkhand, every second new case of leprosy belonged to these communities.
Indeed, leprosy is at risk of becoming a disease exclusively of the Adivasis in certain states like Gujarat, where despite constituting only 14.8 percent of the state population, Adivasis bear 64.9 percent of the total new leprosy case load. Madhya Pradesh’s Adivasis (who comprise 21 percent of the population) bear 39.4 percent of the new leprosy case load in the state. Maharashtra, which has under 10 percent Adivasis, had 33.7 percent of all new leprosy cases reported from the community.[xlv] West Bengal’s Adivasis report 20.3 percent of all new leprosy cases when their proportion in the state population is only 5.8 percent. Tripura, with 31.8 percent Adivasis and Dadra and Nagar Haveli with 52 percent Adivasis, report 64.7 percent and 98.2 percent of new leprosy cases from among the Adivasi communities, respectively.
The irony may be that as leprosy continues to be a major public health problem for the country, the strategies to contain it are simple enough and the drugs are available in the public sector.[xlvi] This draws into question the priorities of the country’s national and state health policies and their implementation. Government’s own data from districts like Tapi in Gujarat—with more than 80 percent Adivasis—show that the incidence of leprosy has gone up from 9.37 per 10,000 population in 2010 to 17.16 per 10,000 population in 2014.[xlvii] The question, therefore, is whether inadequate attention is being given to this silent emergency hitting the most underserved populations of the country because the emerging spread of the disease is occurring far away from the public gaze in the metros.
The increased number of leprosy patients who are Adivasis may be partly because of the improved surveillance in the far-flung areas, but it is equally possible that part of the increased numbers is due to the policy neglect of leprosy during the post-elimination decade. On the other hand, states like Manipur, Chhattisgarh, Sikkim, Punjab, Rajasthan, Haryana, Assam Jammu & Kashmir, Delhi, Puducherry, Goa and Himachal Pradesh have reported a lesser proportion of leprosy cases from these communities, when compared to their proportion in overall population (See Graph 5).
Graph 5: State-wise proportion of Dalits and Adivasis among new leprosy cases (2017)
http://www.nlep.nic.in/data.html
3) Immediately arrest the decline in the percentage of districts with a prevalence of less than 1 per 10,000 population
After a clear trend of substantial improvement in the past, the percentage of Indian districts with leprosy prevalence more than 1 per 10,000 population has started going up again, after hitting the lowest point of 15.3 percent in 2012 (See Graph 6). As discussed earlier, the national declaration of leprosy elimination, and the policy neglect of the disease that followed may have had a dampening effect on the rate of improvement immediately post-2005, and the inevitable reversal 2012 onwards. While in 2010, there were no district in India with a prevalence level of more than 5/10,000 population, in 2017, there are four such districts.[xlviii]
Graph 6: Percentage of Indian districts with leprosy prevalence more than 1 per 10,000 population
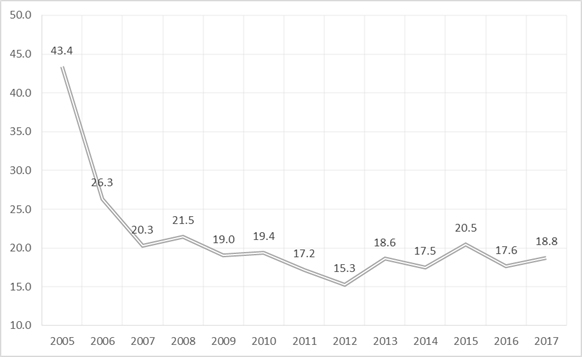
Source: http://www.nlep.nic.in/data.html
A three-pronged strategy was introduced in the National Leprosy Eradication Programme (NLEP) during 2016-17. The components of the strategy were the following: a) A Leprosy Case Detection Campaign; b) A Focused Leprosy Campaign; and c) A Special Plan for Hard to Reach Areas. According to NLEP sources, during 2016-17, LCDC was carried out in 163 districts of 20 states, wherein 34,672 cases were detected and were put on treatment. During 2017-18, the Leprosy Case Detection Campaign was expanded to a total of 305 districts in 23 states and it is likely that some part of the new cases detected can be the result of NLEP reaching erstwhile unreached areas and populations. [xlix] However, these new cases must have only compensated for the reduction in case numbers resulted from better records management, as seen in Bihar in the past when third-party validation caused removal of a large number of cases that had overstayed in the register.[l]
Additionally, ASHAs who are a mainstay of the current strategy have already been involved in the leprosy programme for the last eight years, and it is clear that earlier gains have stagnated and that the country is at risk of a re-emergence of leprosy as a public health problem in substantial areas.[li] According to the latest figures from the government, 128 districts have reported a prevalence rate which is higher than 1/10,000 population. As of March 2017, 53 districts in 11 States/UTs reported a prevalence rate higher than 2/10,000 population. These states are Bihar (four districts); Odisha (eight districts); Chhattisgarh (15); Gujarat (five); Jharkhand (three); Madhya Pradesh (two); Maharashtra (six); West Bengal (six); D&N Haveli (one); Lakshadweep (one); and Delhi (two districts).[lii] It needs to be remembered that in 2010, only 20 districts in seven states had a prevalence rate higher than 2/10,000 population.[liii]
The need of the hour is a clear focus and urgent action, instead of repeating the mistakes of the past and resorting to shallow declarations which only serve to misguide the public health machinery into a false sense of achievement and make sub-national leadership complacent.
Conclusion
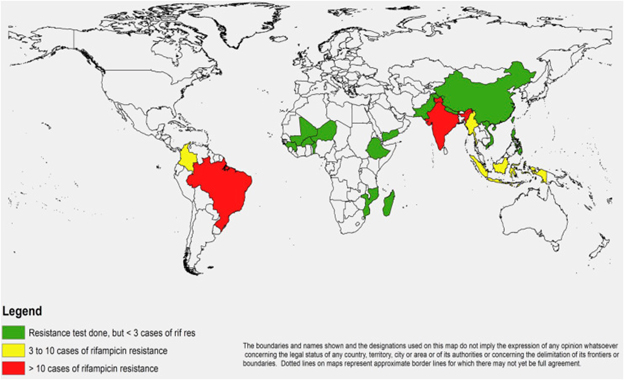
India’s challenges in leprosy include low detection, high level of concentration of the disease in already marginalised population groups, and the patchy implementation of the detection and treatment programme. These problems are compounded by emerging challenges like Antimicrobial Resistance (AMR) which, beginning in the 1980s, had resulted in leprosy mono-therapy being replaced by combined treatment.[liv] Meanwhile, a first-ever comprehensive global study explored the status of AMR in leprosy across countries and found alarming patterns about India (See Map 1). India is one of the three countries—besides Brazil and Indonesia—where cases with resistance to more than one drug were identified.[lv]
Map 1: Map of countries reporting rifampicin resistance in leprosy between 2009 and 2015
Source: Cambau, E., P. Saunderson, M. Matsuoka, S. T. Cole, M. Kai, P. Suffys, P. S. Rosa et al. “Antimicrobial resistance in leprosy: results of the first prospective open survey conducted by a WHO surveillance network for the period 2009–15.” Clinical Microbiology and Infection (2018).
The Government of India has launched post exposure prophylaxis with single dose rifampicin for all contacts of leprosy cases detected across the country with effect from 2 Oct 2018 under NLEP.[lvi] Finding the hidden cases in the community using the recently launched ASHA based Surveillance for Leprosy Suspect (ABSULS) will be an important step forward for treatment as well as prevention.[lvii] However, research has shown that the protective effect of chemoprophylaxis (57 percent overall risk reduction) was seen only in the first two years, with no additional effect after four years.[lviii]
Over the last decade, India has been committing substantial sums to leprosy research, and in 2017, India overtook the US as the largest funder of leprosy research & development, accordingto latest available global data.[lix] However, for these efforts to bring change on the ground, India’s challenges to eliminate leprosy at the state level, followed by elimination at the district level—and indeed, eradication—are contingent on the health system overcoming weaknesses in identification, treatment, management of multiple systems of medicine, removing stigmatisation, and addressing knowledge gaps. Provision of reconstructive surgery for leprosy patients is part of the care package of the Pradhan Mantri Jan Aarogya Yojna (PMJAY), which is the insurance arm of the Ayushman Bharat scheme—this will bring relief to thousands of patients.[lx] India cannot afford to be complacent about leprosy, and the Ayushman Bharat initiative can be a true beginning of the end of this oft-“eliminated” disease in India. This requires that the implementation of the Health and Wellness Centres initiative be made in the true spirit of comprehensive primary healthcare approach, which takes healthcare to the last person.
Endnotes
[i] Census of India (2016), accessed at http://www.censusindia.gov.in/Vital_Statistics/SRS_Life_Table/2.Analysis_2010-14.pdf
[ii] Targets fixed 15 years ago: Fact check on repackaging of National Health Policy, Hindustan Times, March 17, 2017, accessed at https://www.hindustantimes.com/india-news/targets-fixed-15-years-ago-fact-check-on-repackaging-of-national-health-policy-2017/story-1FbjE6PnKSMed1C6mp56II.html
[iii] Census of India (2018), accessed at http://www.censusindia.gov.in/Vital_Statistics/SRS_Life_Table/SRS-12-16/2.Analysis_2012-16.pdf
[iv] Data adjusted for underreporting and misclassification of deaths.
[v] WHO (2015) , Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, accessed at http://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf?sequence=1
[vi] Government of India (2017), Ministry of Health and Family Welfare, National Health Policy 2017, accessed at https://mohfw.gov.in/sites/default/files/9147562941489753121.pdf
[vii] Repackaged: 15-Year-Old National Health Policy Resurrected In 2017 , Fact Checker, accessed at http://factchecker.in/repackaged-15-year-old-national-health-policy-resurrected-in-2017/
[viii] World Health Organization (2016), India’s massive leprosy case detection campaign reaches 320 million people, accessed at: http://www.who.int/neglected_diseases/news/India_massive_leprosy_case_detection_campaign_reaches_320_mill/en/
[ix] Government of India (2017), PM’s Message on the Occasion of Anti Leprosy Day, accessed at http://pib.nic.in/newsite/PrintRelease.aspx?relid=157753
[x] Government of India (2017), Union Budget document, accessed at https://www.indiabudget.gov.in/ub2017-18/bs/bs.pdf
[xi] Economic Times (2018), India will be free of leprosy this year: J P Nadda, June 09, accessed at
https://economictimes.indiatimes.com/news/politics-and-nation/india-will-be-free-of-leprosy-this-year-j-p-nadda/articleshow/64522307.cms
[xii] Government of India (2018), Ministry of Health and Family Welfare, National Health Profile 2018, accessed at http://www.cbhidghs.nic.in/Ebook/National%20Health%20Profile-2018%20(e-Book)/files/assets/common/downloads/files/NHP%202018.pdf
[xiii] The Wire (2016), accessed at https://thewire.in/health/as-leprosy-cases-increase-government-pushes-elimination-target-to-2019
[xiv] The Indian Express (2016), The Fight Against Leprosy, accessed at https://indianexpress.com/article/opinion/columns/the-fight-against-leprosy-symptoms-india-causes-cures-3071272/
[xv] Lockwood, Diana NJ, Vanaja Shetty, and Gerson Oliveira Penna. “Hazards of setting targets to eliminate disease: lessons from the leprosy elimination campaign.” Bmj 348 (2014): g1136.
[xvi] World Health Organisation (2016), Global Leprosy Strategy 2016–2020: Accelerating towards a leprosy-free world, accessed at http://apps.who.int/iris/bitstream/handle/10665/250119/9789290225256-Eng.pdf?sequence=5
[xvii] Ibid.
[xviii] Government of India (2015), accessed at: http://lawcommissionofindia.nic.in/reports/report256.pdf
[xix] Hindustan Times, 30 October, 2018, https://www.hindustantimes.com/pune-news/pune-hospital-admits-a-family-of-lepers/story-OgoaSoIVtmCBVVWodg9UyI.html , accessed on 1 November 2018.
[xx] https://www.livelaw.in/top-stories/lok-sabha-passes-personal-laws-amendment-bill-remove-leprosy-ground-divorce-141925
[xxi] World Health Organisation (2017), Global leprosy update, 2016: accelerating reduction of
disease burden, accessed at http://apps.who.int/iris/bitstream/handle/10665/258841/WER9235.pdf?sequence=1
[xxii] Ibid.
[xxiii] Ibid.
[xxiv] Singal, Archana, and Sidharth Sonthalia. “Leprosy in post-elimination era in India: Difficult journey ahead.” Indian Journal of Dermatology 58, no. 6 (2013): 443.
[xxv] Government of India (2018), National Leprosy Eradication Programme, accessed at http://www.nlep.nic.in/data.html
[xxvi] Ibid.
[xxvii] Mishra, C. P., and M. K. Gupta. “Leprosy and stigma.” Indian J. Prev. Soc. Med 41, no. 1& (2010): 2.
[xxviii] Jacob, Jesse T., and Carlos Franco-Paredes. “The stigmatization of leprosy in India and its impact on future approaches to elimination and control.” PLoS neglected tropical diseases 2, no. 1 (2008): e113.
[xxix] Ibid.
[xxx] Naaz, Farah, Partha Sarathi Mohanty, Avi Kumar Bansal, Dilip Kumar, and Umesh Datta Gupta. “Challenges beyond elimination in leprosy.” International journal of mycobacteriology 6, no. 3 (2017): 222.
[xxxi] National Leprosy Eradication Programme (2018), accessed at http://nlep.nic.in/pdf/NLEP%20Newsletter%20july-sept%209-11-16%20(Dummy).pdf
[xxxii] Ayushman Bharat (meaning ‘an India blessed with a long, healthy life’) has two main pillars: strengthening of universal comprehensive primary health care using a health and wellness centre (HWC) initiative and a health insurance scheme named the Pradhan Mantri Jan Arogya Yojana (PMJAY) to cover 500 million people who belong to the poorer sections of society.
[xxxiii] The Financial Times (2017), Leprosy: India’s hidden plague , accessed at https://www.ft.com/content/b7c8ffb2-ff67-11e6-8d8e-a5e3738f9ae4?saveConsentPreferences=success
[xxxiv] Various newspaper items available at https://indianexpress.com/article/india/india-will-be-free-of-leprosy-this-year-nadda/ , https://www.business-standard.com/article/current-affairs/leprosy-free-for-12-years-india-saw-79-000-new-cases-in-6-months-of-2016-117071700992_1.html , https://timesofindia.indiatimes.com/india/india-will-be-free-of-leprosy-this-year-nadda/articleshow/64522219.cms and http://www.dailymail.co.uk/indiahome/indianews/article-3220286/India-sees-849-leprosy-cases-despite-officially-free-disease-2005.html
[xxxv] The Financial Times (2017), Leprosy: India’s hidden plague , accessed at https://www.ft.com/content/b7c8ffb2-ff67-11e6-8d8e-a5e3738f9ae4?saveConsentPreferences=success
[xxxvi] Chaptini, Casandra, and Gillian Marshman. “Leprosy: a review on elimination, reducing the disease burden, and future research.” Lepr Rev 86, no. 4 (2015): 307-15.
[xxxvii] The Quint (2018), accessed at https://fit.thequint.com/health-news/why-doesnt-leprosy-cripple-the-rest-of-the-world-like-india-2
[xxxviii] Singal, Archana, and Sidharth Sonthalia. “Leprosy in post-elimination era in India: Difficult journey ahead.” Indian Journal of Dermatology 58, no. 6 (2013): 443.
[xxxix] The Quint (2018), accessed at https://fit.thequint.com/health-news/why-doesnt-leprosy-cripple-the-rest-of-the-world-like-india-2
[xl] Lockwood, Diana NJ, Vanaja Shetty, and Gerson Oliveira Penna. “Hazards of setting targets to eliminate disease: lessons from the leprosy elimination campaign.” Bmj 348 (2014): g1136.
[xli] Ibid.
[xlii] Ibid.
[xliii] Fine, Paul EM. “Leprosy: what is being ‘eliminated’?” Bulletin of WHO (2007): 2-2.
[xliv] Government of India (2018), accessed at http://pib.nic.in/newsite/PrintRelease.aspx?relid=179968
[xlv] http://www.nlep.nic.in/data.html
[xlvi] Leprosy requires a course of drugs lasting between six months and two years, freely available in government hospitals.
[xlvii] Government of Gujarat (2015), District Human Development Report, Tapi, accessed at http://www.in.undp.org/content/dam/india/docs/human-development/District%20HDRs/8.%20Tapi_DHDR_May_2016.pdf
[xlviii] Government of India (2018), accessed at http://www.nlep.nic.in/data.html
[xlix] Government of India (2018), accessed at http://www.nlep.nic.in/pdf/Annual%20report_%202016-17_rev.pdf
[l] World Health Organisation (2016), Global Leprosy Strategy 2016–2020: Accelerating towards a leprosy-free world, accessed at http://apps.who.int/iris/bitstream/handle/10665/250119/9789290225256-Eng.pdf?sequence=5
[li] Government of India (2018), accessed at http://www.nlep.nic.in/pdf/Annual%20report_%202016-17_rev.pdf
[lii] Government of India (2018), accessed at http://www.nlep.nic.in/data.html
[liii] Government of India (2012), accessed at http://www.nlep.nic.in/pdf/ProgressReport31March2009-10.pdf
[liv] World Health Organisation (2017), Report on BCG vaccine use for protection against mycobacterial infections including tuberculosis, leprosy, and other nontuberculous mycobacteria (NTM) infections, accessed at http://www.who.int/immunization/sage/meetings/2017/october/1_BCG_report_revised_version_online.pdf
[lv] Cambau, E., P. Saunderson, M. Matsuoka, S. T. Cole, M. Kai, P. Suffys, P. S. Rosa et al. “Antimicrobial resistance in leprosy: results of the first prospective open survey conducted by a WHO surveillance network for the period 2009–15.” Clinical Microbiology and Infection (2018).
[lvi] Government of India (2018), accessed at http://nlep.nic.in/pdf/DO%20NO%2011016.7.1514SEP2018.pdf
[lvii] Government of India (2017), accessed at http://nlep.nic.in/pdf/Guidlines%20ABDULS%20Final.pdf
[lviii] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5885632/ P Narasimha Rao, Sujai Suneetha. “Current Situation Of Leprosy in India and its Future Implications” (2018)
[lix] Chapman, Nick, Anna Doubell, Lisette Oversteegen, Paul Barnsley, Vipul Chowdhary, George Rugarabamu, Ming Ong, and Juliette Borri. “Neglected Disease Research and Development: Reaching new heights”, G-FINDER Report, 2018, accessed at https://www.policycuresresearch.org/g-finder-2018/
[lx] Government of India (2018-19), accessed at http://nlep.nic.in/pdf/SLEC%20booklet%20.pdf
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

 PDF Download
PDF Download


 PREV
PREV


