-
CENTRES
Progammes & Centres
Location
 PDF Download
PDF Download 
Laetitia Warjri and Anushka Shah, “India and Africa: Charting a Post-COVID-19 Future,” ORF Special Report No. 111, June 2020, Observer Research Foundation.
Introduction
COVID-19 has spread to over 200 territories and countries across the globe, exposing the fragility of healthcare systems, the inefficiency of social protections frameworks, and the lack of economic resilience.[1] Governments have taken drastic measures like imposing country-wide lockdowns and closing borders to arrest the further spread of the pandemic. These strategies, however, have caused a slowdown in economic activity and trade, in turn disrupting global supply chains. Indeed, the World Trade Organization (WTO) estimates that the impact of the health crisis on global trade will be more severe than that of the financial crisis of 2008-09.[2] Devastating consequences on developing nations like India and the countries of Africa are being witnessed as they emerge as hotspots, owing to the double burden of large populations and weak healthcare infrastructure. Worryingly for both regions, the pandemic has come at a time when they were making appreciable progress towards meeting their Sustainable Development Goals (SDGs). COVID-19 threatens to undermine those achievements.
In developing a shared Indo-African response to the crisis, it is clear that the impact on the economies and healthcare systems of the countries must attain primary importance. Growth forecasts show that the pandemic will likely push regions of Sub-Saharan Africa towards its first recession in 25 years, while India has also recorded its lowest economic growth rate in the past three decades.[3] The expected damage to the economy is compounded by the ongoing direct costs of measures to treat, detect, and reduce the spread of the virus; indirect costs of domestic lockdowns; global supply chain disruption; and plummeting commodity prices. Taken together with the lack of infrastructure and modest healthcare investment over the past several years, societies and governments in Africa and India are ill-prepared and could be overwhelmed by COVID-19.
The immediate response has been focused on maintaining physical distancing, promoting basic hygiene, expanding testing and contact tracing, and imposing restrictions on movement through lockdowns. Post-COVID-19, there will be a need to rebuild and reconstruct healthcare systems while mitigating the economic damage. A rapid rebound will only be possible if policymakers now begin planning for the aftermath of the pandemic while considering the SDG agenda. After all, COVID-19 has not only tested healthcare systems but has affected development goals related to education, gender equality, and eradicating hunger. There is a need for strong, sustained and socially inclusive recovery through active international cooperation. Decisions taken collectively today will shape the prospects for future recovery.
Figure 1. Confirmed COVID-19 Cases, Deaths and Recoveries in India and Africa

The Role of the Private Sector
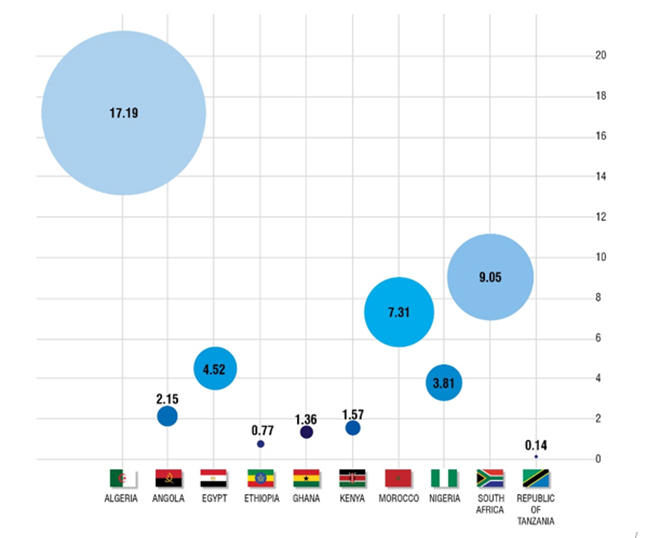
Although the infection rates have been lower than anticipated in India and Africa, the numbers are still growing each day.[4] If the trend continues, the African healthcare system will be ill-prepared to deal with the rise in cases. At present, the continent only has 1.7 ICU beds per 100,000 people and only 20,000 ventilators.[5],[6] There is also a large discrepancy between the healthcare systems in different countries within the continent.[7] For instance, in 2018, Ethiopia had only 0.77 doctors per 10,000 people whereas Nigeria had 3.81 doctors and Zambia had 11.87. The United States, for instance, has better infrastructure with 2.8 beds per 1,000 population and a total of 160,000 ventilators; still, it is overwhelmed in trying to mitigate the outbreak in its territory.[8],[9]
Figure 2. Medical Doctors per 10,000 in Africa
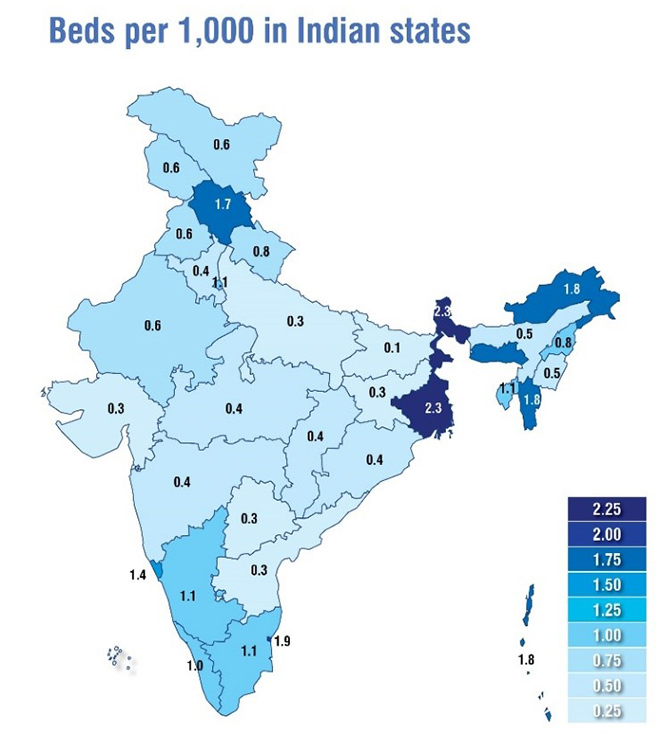
India and its states have a similar story to tell. According to the National Health Profile 2019, India has only one doctor per 10,926 people.[10] The country’s public expenditure towards healthcare has also remained on the lower side—1.28 percent of GDP, which is far below the five percent that WHO recommends. As per 2018 figures from Gujarat, for a population of 64 million, there are only 3.16 hospital beds and 43 physicians, nurses and midwives per 10,000 population; in Bihar, for a population of 114 million, there are only 0.98 hospital beds and 19 physicians, nurses and midwives per 10,000 population.
Figure 3. Government Hospital beds per population 1,000
To achieve higher investment in healthcare, there is a need to integrate the private sector into capacity building of healthcare systems and healthcare delivery. Private manufacturers can also contribute to the supply of hazmat suits, N95 masks, gloves and other medical equipment. In France, for example, luxury conglomerate LVMH has repurporsed its perfume factories to produce hand sanitisers.[11]
In a crisis, the imperative is to develop preventive solutions that require research and development. As this is a long-drawn out process that comes with a high degree of risk of failure as well, public-private partnerships can play a crucial role in sharing the risk. Not only does the private sector often have the capital to do so, but it is also more likely to attract the necessary expertise.
This collaboration can already be seen on the ground. For instance, in South Africa, the government and private sector are collaborating on the National Ventilator Project, which aims to manufacture 10,000 ventilators by the end of June through local sourcing.[12] An apparel factory in Kenya is now making 30,000 masks per day.[13]
In India, the Serum Institute is working towards developing a vaccine in collaboration with researchers at the University of Oxford.[14] In the city of Mumbai, Reliance Industries has built a 100-bed hospital dedicated to COVID-19 patients.[15] In May, an MoU was signed between the Indian Institute of Integrative Medicine (IIIM) which is a national Institute of the Council of Scientific and Industrial Research (CSIR) of India, and Reliance Industries to develop and scale up the manufacture of (RT-LAMP-based)[a] COVID-19 diagnostic kits.[16] Rapid tests like these can cater to larger populations, especially vulnerable sections of society who do not have easy access to health facilities. Industrialist Anand Mahindra has announced measures to manufacture ventilators and to convert Mahindra resorts into COVID-19 care centres.[17] With more than 60 Indian companies certified to produce Personal Protective Equipment (PPE), the country produces more than 0.45 million pieces a day.[18] Indeed, the PPE industry in India has grown 56 times in less than 60 days, making the country the world’s second largest PPE supplier after only China. The Serum Institute of India has partnered with Zipline, a company engaged in healthcare delivery using drones, to make protective kits and medicines available in the most remote regions of India.[19]
Economic Responses to Strengthen SDG Agendas
The COVID-19 pandemic is posing a serious challenge to the attainment of SDGs across the globe. For instance, the International Labour Organization (ILO) estimates that approximately 25 million people could lose their jobs, out of which those in the informal sector would be hardest hit from lack of social protection.[20] In another report, the ILO stated that 400 million of India’s informal workforce could be pushed deeper into poverty due to the pandemic.[21]
Similarly, for Africa, out of the total labour force of 440 million, formal sector employees comprise one-third, or 140 million.[22] An analysis done by McKinsey & Company suggests that nine million to 18 million people in the formal sector could lose their jobs, whereas 30 million to 35 million are at risk of pay cuts and shorter working hours due to the reduced demand resulting from the lockdown.[23]
The service sector, manufacturing industries, tourism, and construction have been severely affected in both Indian and African economies. While India and several African countries have announced fiscal stimulus packages, it is unclear whether the measures will be adequate and if they will reach the targeted populations at all.[24] In the case of India, among other responses, a package valued at approximately 10 percent of GDP was announced for workers in the healthcare sector as well as low-wage workers, which includes tax breaks for MSMEs (Micro, Small and Medium Enterprises), incentives for manufacturing units, and cash transfers.[25]
Similarly, several countries in Africa announced stimulus measures valued between one to 1.5 percent of their GDP. Well-targeted fiscal-stimulus measures can have a multiplier effect on GDP, notwithstanding the comparatively limited financial intervention by India.
In the case of Africa, the economic fallout from the pandemic will be determined more by the impact on its trading partners than the duration of its spread in the continent. Fiscal measures should focus on mitigating adverse effects on the most vulnerable communities by deferred tax payments, wage subsidies, and food programmes.
Technological Responses
Developing nations like India and those in Africa are seeing the important role of technological solutions in the fight against COVID-19.
India, for example, has launched the Aarogya Setu App,[26] which was developed as a public-private partnership.[27] Using the Bluetooth and GPS systems of a smartphone, the app alerts users when they come within six feet of a COVID-19 patient. Alerts are generated by scanning through government-owned, location-specific databases. The user also receives an advisory by the Ministry of Health and Family Welfare on self-isolation practices. It aims to speed up the process of identifying, testing, and isolating people exposed to the virus before they spread it to others. Apart from contact-tracing apps, states like Arunachal Pradesh are using apps to deliver essentials to minimise people’s exposure to the virus.[28] Indian cities like Varanasi and Chandigarh have seen a wide-scale adoption of drones, which are being used to disinfect public spaces.[29] Drones have also been deployed by the police for surveillance in states like Jharkhand, Kerala, Tamil Nadu, and Gujarat.[30]
Another area of technological application is telemedicine, for which the MoHFW along with NITI Aayog and the Board of Governors (BoG) of the Medical Council of India (MCI), have already issued guidelines.[31] As doctors are now able to connect with patients online, this has helped reduce the burden on hospitals. It has also helped limit the exposure of people with non-COVID-related ailments to hospitals that could be sources of infection. Further, to benefit from technological applications such as artificial intelligence (AI), on 18 May 2020, the Apollo Hospitals Group partnered with a UK-based Artificial Intelligence radiology company to develop a pilot on AI-based chest X-ray technology.[32] The Wadhwani Group is also doing research on the use of AI to analyse cough sounds to detect COVID-19 in its early stages.[33]
To be sure, technological solutions also aid in the most elementary tasks during public health crises such as the ongoing pandemic. These include not only the management of misinformation but the education of citizens by communicating facts, such as those around best practices in hygiene. The Government of India, through its COVID-19 portal keeps citizens informed on the prevailing situation and on the safety measures that need to be taken to prevent the further spread of the disease.[34] Government agencies in this regard are making use of different social media platforms, such as Facebook, Instagram, Twitter, YouTube, LinkedIn, Telegram, TikTok, Helo, VMate, and Likee.[35]
Similarly, in South Africa, the country’s biggest telecommunications company Telkom, in partnership with Samsung, is assisting the government to contain the spread through contact tracing.[36] South Africa is also addressing misinformation by sending messages to millions with the help of the non-profit Praekelt, which leverages mobile technology for pro-poor programmes.[37] In Kenya, meanwhile, Safe Hands Kenya is using existing technology-enabled supply chains to supply sanitisers, masks, soap, and surface disinfectant to the poor.[38]
Biometric digital identification is another tool that could gain traction, especially when the implementation of large stimulus packages will be a challenge for many. Digital identification registers will be useful to both India and African countries as their stimulus packages involve the provision of direct cash transfers to people below the poverty line.
Technology has also become imperative for the education sector, as schools turn to online learning during the pandemic. Considering half of India’s population is under the age of 25, there is massive potential for the growth of online education in India. A KPMG and Google study done in 2017, before COVID-19, estimated that the online education market in India was set to grow to US$1.96 billion, with 9.6 million users by 2021.[39] This is a considerable jump from its worth in 2016, which was US$247 million with 1.6 million users. While these numbers are impressive, ongoing studies suggest that more than 90 million in India have signed up for online courses during the lockdown, with still more potential for exponential growth. Investment in technology is key towards meeting this potential. India’s learnings in the EduTech sector can prove to be an invaluable resource for nations in Africa, who also have similarly young demographics and potential for growth.
Country-Level Response in Africa
As countries in Africa differ in terms of economic development, urbanisation, employment, and social welfare, each one has had to face their own battle against COVID-19. Governments, therefore, have responded differently to the pandemic.
Figure 4: COVID19 Status in the 10 most affected African Countries

South Africa enforced a nationwide lockdown on March 27 and also closed its borders to limit the movement of people.[40] However, the border remained open for the transfer of goods. Nigeria, for its part, imposed a partial lockdown with full border closure;[41] and Ethiopia ordered the closure of schools, colleges, and public spaces, and banned public gatherings. Air traffic in Ethiopia remained open, however, while land borders were closed.[42]
In Ghana, the situation has not been as controlled as it was during the spread of Ebola between 2014-2016. In that epidemic, community leaders played a critical role in conducting surveillance as well as communicating to the people the importance of social distancing.[43] This time, analysts are observing low compliance with social-distancing measures.[44]
For the government of Kenya, COVID-19 has posed multiple challenges owing to the limited awareness to the risks associated with the virus, and the fragile nature of the healthcare system.[45] The government has faced difficulty in convincing the population to adhere to basic preventive measures. These factors are further compounded by limited testing capacity, and officials are unable to capture the full extent of the pandemic. Another challenge comes from cross-border travel of people from Tanzania to Kenya. While a nationwide lockdown was imposed in Kenya, the same was not the case for Tanzania. There were people who travelled to Kenya from Tanzania, then tested positive, and were deported.[46] This underlines the need for improved cross-border cooperation among African countries.[47]
Figure 5: Tests per one million v/s infection detected across states in India

The first priority of African governments has often been communicating the seriousness of the threat.[48] Considering a large proportion of Africa’s population lives in densely populated areas with little prospect for social distancing, communicating to the people the importance of basic hygiene becomes even more crucial as this affects the pace with which compliance can be achieved for various other public health measures.
Conclusion and Recommendations
The fight against COVID-19 has put emphasis on preventing the further spread of infection. It is time for governments to look to the future, towards creating regimes that will allow for greater cooperation between nations to ensure that even the most vulnerable have access to healthcare, especially to medicines and vaccines. For long-term resilience, the preparedness of India and Africa’s healthcare systems for future pandemics must be reviewed.
This report makes the following recommendations.

Laetitia Warjri is Associate Fellow, and Anushka Shah is a Research Assistant at ORF.
[a] RT-LAMP means ‘Reverse Transcriptase-Loop Mediated Isothermal Amplification’. These test kits use throat/nasal samples to detect if a person is COVID positive or not. They are cost-effective, they provide accurate results in less than 60 minutes, and they require basic setups that can be done in areas like airports.
[1] John Hopkins University and Medicine – Coronavirus Research Centre, May 2020.
[2] World Trade Organization, Press Release, April 2020.
[3] The World Bank, Press Release, “COVID-19 (Coronavirus) Drives Sub-Saharan Africa Toward First Recession in 25 Years”, April 2020.
[4] Observer Research Foundation, “Tracking COVID 19 in South Asia and Beyond”, May 2020.
[5] Niall McCarthy, “The Countries With The Most Critical Care Beds Per Capita [Infographic]”, March 2020.
[6] Aryn Baker, “Few Doctors, Fewer Ventilators: African Countries Fear They Are Defenseless Against Inevitable Spread of Coronavirus”, April 2020.
[7] World Health Organization, Medical Doctors (per 10,000),
[8] John Hopkins Centre for Health Security, “Ventilator Stockpiling and Availability in the US”, April 2020,
[9] “OECD.Stat”, “Health Care Resouces”, May 2020.
[10] National Health Profile 2019.
[11] Richard Kestenbaum, ”LVMH Converting Its Perfume Factories To Make Hand Sanitizer”, March 2020.
[12] Helena Wasserman and Phillip de Wet, “The design of SA’s first ventilator for mass production is expected within days”, April 2020.
[13] Max Bearak, “The Kenyan factory that transformed into a surgical mask assembly line overnight”, April 2020.
[14] “Serum Institute eyes COVID-19 vaccine by October”, April 2020.
[15] “Reliance Industries sets up 100-bed centre for coronavirus patients; to make 1 lakh masks daily”, March 2020.
[16] Press Information Bureau, “CSIR-IIIM, Jammu signs MoU with RI”, May 2020.
[17] “Coronavirus crisis: Mahindra factories to make ventilators; Anand Mahindra to give away salary to COVID-19 fund”, March 2020,
[18] M Ramesh, “India becomes second largest supplier of PPE in the world”, May 2020.
[19] Sohini Das, “Maharashtra govt plans to deliver emergency medicines through drones”.
[20] International Labor Organization, COVID-19: Protecting workers in the workplace, March 2020.
[21] “ILO Monitor: COVID-19 and the world of work. Second edition”, April 2020.
[22] Kartik Jayaram, Amandla Ooko-Ombaka, Ying Sunny Sun, and Acha Leke, “Finding Africa’s path: Shaping bold solutions to save lives and livelihoods in the COVID-19 crisis”, April 2020.
[23] Ibid.
[24] International Monetary Fund, Policy Tracker.
[25] PTI, “India’s Rs 20 lakh crore Covid relief package one among the largest in the world, May 2020”.
[26] My Gov.in, Aarogya Setu App,
[27] PIB, “AarogyaSetu: A multi-dimensional bridge”, April 2020.
[28] Oommen Kurian and Sangeet Jain, “State of the States: Two months of the pandemic”, May 2020,
[29] Ibid.
[30] Ibid.
[31] Ministry of Health and Family Welfare, “Telemedicine Practice Guidelines” March 2020.
[32] GlobalNews Wire, Press Release, “Behold.ai partners with Apollo Hospitals Group, India for rapid COVID-19 diagnosis using AI-based chest X-ray technology”, May 2020.
[34] My Gov.in, COVID-19 Dashboard.
[35] Shubhangi Agarwal, “Communications on COVID-19”, May 2020.
[36] Aditya Chaturvedi, “How South Africa uses tech to fight Covid-19”, April 2020,
[37] Health Connect for COVID-19.
[39] Times of India, “India’s online edu industry set to reach $1.96 bn in 2021: Report“, June 2020.
[40] Elliot Smith, “South Africa deploys police and army to enforce 3-week coronavirus lockdown”, March 2020.
[41] Thomas Herman, Nila Wilde, Eva Maarek, Sharif Abousaada and François Adao “COVID-19: Initial responses of certain African countries”.
[42] Ibid.
[43] Amy S. Patterson, “The coronavirus is about to hit Africa. Here are the big challenges”, February 2020.
[44] Gameli Aheto, “I’m an Emergency Doctor Tackling COVID-19 in Ghana. Here’s What’s Giving Me Hope”.
[45] ““Diseases will not wait” for COVID-19 in Kenya”, May 2020.
[46] “Kenya deports 182 virus carriers back to Tanzania”, May 2020.
[47] “Kenya, Tanzania agree on Covid-19 testing and cross-border movement”, May 2020.
[48] Shannon Smith, “Managing Health and Economic Priorities as the COVID-19 Pandemic Spreads in Africa”, March 2020.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

Laetitia Bruce Warjri was a Head of Communications and Outreach at ORF. Before joining ORF, Laetitia worked as a journalist with the India Today Group and ...
Read More +
Anushka Shah was Sub-Editor at ORF. Anushkas research interests include: climate finance urban environmental policy use of technology for socioeconomic development.
Read More +