Immunisation is key to child survival and is cost effective in protecting their lives. But with the looming threat of Covid-19 pandemic, 23 million children globally missed out routine immunisation last year. The pandemic has further worsened the worrying trends on immunisation against preventable child illness. A recent review on impact of Covid-19 on immunisation campaigns and programmes suggests a reduction in both coverage and number of vaccines administered due to lockdown restrictions, shortage of health workers and resource diversion to address the andemic. Each $1 invested in child immunisation brings a return of $44 for low and middle-income countries.
Immunisation coverage data shows a plateau over decades, with global coverage of 83% and increase in unvaccinated by 3.4 million in 2020. The recent modelling study by Lancet finds a significant gap in vaccine coverage by end of 2020, extending throughout 2021. Findings estimate a dip in coverage for diphtheria-tetanus-pertussis (DTP) 3 at 76·7% and measles vaccine at 78·9% in 2020. India experienced a large drop in DTP3 vaccine coverage from 91% to 85%. According to recent data released by WHO-UNICEF, over 3 million children in India have missed out on their first dose of DTP in 2020, more than double the numbers of children in 2019.
Even though India has seen tremendous progress in immunisation coverage through its Mission Indradhanush programme (now Intensified Mission Indradhanush-IMI) targeting 27 million newborns and 29 million pregnant women annually. Regardless of this, infectious diseases continue to contribute to a significant proportion of child mortality and morbidity in India. According to the Pneumonia and Diarrhea Progress report 2020, nearly half million pneumonia and diarrhoea deaths occur in India followed by Nigeria. India can markedly reduce those deaths through an integrated package of interventions-exclusive breastfeeding, immunisation and improving water and sanitation and reducing exposure to air pollution.
Even though India has seen tremendous progress in immunisation coverage through its Mission Indradhanush programme (now Intensified Mission Indradhanush-IMI) targeting 27 million newborns and 29 million pregnant women annually. Regardless of this, infectious diseases continue to contribute to a significant proportion of child mortality and morbidity in India
The recent NFHS-5 data (2019-20) from 22 states/UTs indicates an improvement on the full immunisation coverage in children (12-23 months) as indicated in figure 1. Going by the national figures from NFHS-4 (2015-16) the full immunization rate was 62%.
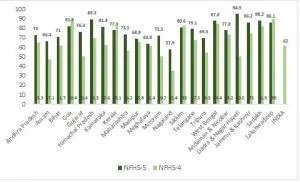 Figure 1: Children 12-23 months fully immunized in 22 states/UTs
Figure 1: Children 12-23 months fully immunized in 22 states/UTs
A major problem in India and other similarly high-burden countries is the inequality in vaccine administration amongst vulnerable children. Evidence suggest socioeconomic status based vaccine disparity with the disadvantaged and undeserved groups being left out. Recent review shows a slight improvement in wealth related inequality in few states in India, however, a more targeted approach is needed to overcome it. Vaccine coverage for India has gone up by only 19% from 2006 to 2016, largely attributable to lack of awareness, migrant population, and access to vaccination.
Vaccine hesitancy is a challenge for India for reasons of parents’ literacy, their income, their knowledge on the vaccination schedule and false beliefs. Pandemic has seen the rise of vaccine hesitancy among the educated and privileged for reasons of misinformation. An analysis of the IMI has found that the lack of skills and inadequate time are the key limiting factors on the capabilities of community health workers in providing effective counselling. It suggests for providing clear, accurate information to counter misinformation and myths around vaccination.
Vaccine hesitancy is a challenge for India for reasons of parents’ literacy, their income, their knowledge on the vaccination schedule and false beliefs. Pandemic has seen the rise of vaccine hesitancy among the educated and privileged for reasons of misinformation. An analysis of the IMI has found that the lack of skills and inadequate time are the key limiting factors on the capabilities of community health workers in providing effective counselling
In order to address the disruption of routine immunisation by the pandemic, the Indian Academy of Pediatrics have issued recommendations for routine immunisation of Covid-19 suspect and positive children. Immunisation is beneficial and far outweigh the risk of infections as observed during Ebola outbreak, where the number of deaths due to measles, malaria, and tuberculosis due to disruption of health services far exceeded that from Ebola. According to benefit–risk analysis of health benefits versus excess risk of SARS-CoV-2 infection in Africa, ‘for every one excess COVID-19 death attributable to SARS-CoV-2 infections acquired during routine vaccination clinic visits, 84 deaths in children could be prevented by sustaining routine childhood immunisation’.
As early as March-April 2020, an alarming 5 million children from across 600,000 villages in India may have lost the chance to routine immunisation. A survey of peadiatricians to understand Covid-19 related disruptions to routine vaccination services in India, reported a 50% decline in vaccination services with slow recovery. More than 75% expressed concern on the gap in vaccination coverage leading to non-Covid morbidity and mortality. Essential health services have been affected across the board, according to the WHO’s Pulse survey on continuity of essential health services during the COVID-19 pandemic (figure 2). The most frequently disrupted services include routine immunization services — outreach services (70%) and facility-based services (61%).
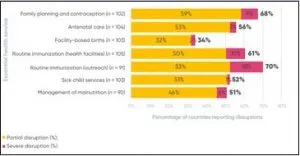 Figure 2: Percentage of countries reporting disruption in essential health and nutrition services
Figure 2: Percentage of countries reporting disruption in essential health and nutrition services
A narrative review in line with WHO’s guidance document recommends sustaining immunisation programmes specially focusing on the vulnerable who missed out during the pandemic. India rolled out the IMI 3.0 in February 2021, targeting children and pregnant women who missed out routine immunisation during the pandemic. A review indicates a systematic approach to close the immunisation gap with a prepared health system for equitable rollout of vaccines.
Improving access to immunisation is critical to achieving sustainable development goals. There is an urgent need to take efforts to restore the routine immunisation programmes with all precautionary measures, according to WHO guidelines. According to medical journal Lancet, there is an urgent need to strengthen routine immunisation and outreach to prevent the risk of vaccine-preventable disease in children and accelerate progress for a more equitable vaccination coverage. Greater efforts to communicate the benefits of vaccines through health education and counselling, along with immunisation delivery approaches under safe conditions for health worker, caregiver and the community needs to be adopted.
It is time to invest in immunisation programmes to secure life of the future generations.
This commentary originally appeared in News18
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

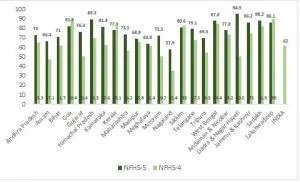 Figure 1: Children 12-23 months fully immunized in 22 states/UTs
Figure 1: Children 12-23 months fully immunized in 22 states/UTs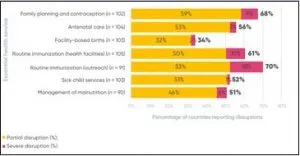 Figure 2: Percentage of countries reporting disruption in essential health and nutrition services
Figure 2: Percentage of countries reporting disruption in essential health and nutrition services