In the next decade, India is bound to become the most populous nation in the world, overtaking China. However, compared globally, India remains a country with among the lowest levels of public health spending, despite the government’s commitment to expand funding. Ayushman Bharat was launched on April 4, 2018, to challenge the status quo in the healthcare delivery system, where for most Indian citizens quality healthcare has remained a luxury good.
Ayushman Bharat involves a two-pronged approach of improving the comprehensive primary healthcare infrastructure on the ground with the rollout of 1.5 lakh Ayushman Bharat - Health and Wellness Centres (AB-HWC) across the country by 2022, and offering substantial financial protection to the poorest 50 crore Indians with secondary and tertiary healthcare insurance.
The health and wellness centres have been off to a slow start, over the last year.
Reportedly, of the 52,744 health and wellness centres for which approvals have been accorded, just over 21,000 have been operational across the country as on Sept. 17, 2019.
Most of the limelight has been on the Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY), the insurance arm of this ambitious and innovative strategy. AB-PMJAY was launched on Sept. 23, 2018, and just completed a year of operation.
Coverage Over The Last Year
As per the latest data available on the scheme’s website, 44 lakh hospitalisations have happened across the country under AB-PMJAY as of today. Given that many intended beneficiaries are still not aware of the scheme, as initial studies suggest, the hospitalisation rates are bound to go up in the future.
West Bengal, Telangana, Odisha, and Delhi are not part of AB-PMJAY yet, mostly for political reasons. Across other states and Union Territories of India, 8,583 public hospitals, 683 private not-for-profit hospitals, and 8,921 private for-profit hospitals are already part of the scheme as of today. These numbers, in particular of the private hospitals, are bound to grow substantially as the scheme matures and a steady flow of patients is ensured.
With a significantly larger risk-cover than what was offered as part of the earlier Rashtriya Swasthya Bima Yojana (RSBY), a consolidation at the level of health insurance schemes is already happening across Indian states. Reportedly, using the AB-PMJAY opportunity, Karnataka has merged seven existing health insurance schemes into one, while Kerala has dovetailed three different healthcare schemes.
Although the Centre has initially identified 50 crore beneficiaries, with many states going further and choosing to widen the population coverage, it is clear that the scheme will also be instrumental in building a larger risk pool, taking India closer to the target of universal health coverage.
Reportedly, eleven states/UTs have expanded AB-PMJAY or the state variant to the point of universal or almost universal coverage.
In addition, 23 states/UTs have expanded the beneficiary base considerably.
Curbing Foul Play
Unlike the RSBY era, plagued by lax monitoring of insurance fraud, AB-PMJAY involves a robust information technology infrastructure overseeing transactions and locating suspicious surges across the country. Many hospitals have been blacklisted and the constantly evolving fraud-control system will play a major role in streamlining the scheme as it matures. However, initial analysis of high-value claims under PMJAY has revealed that a relatively small number of districts and hospitals account for a high number of these, and some hint of an anti-women bias, with male patients getting more coverage.
Initial research shows that over 75 percent of all hysterectomy claims—the surgical removal of the uterus—under AB-PMJAY have been generated in 6 states: Chhattisgarh (21.2 percent); Uttar Pradesh (18.9 percent); Jharkhand (12.2 percent); Gujarat (10.8 percent); Maharashtra (9.0 percent); and Karnataka (6.6 percent).
Shockingly, between September 2018 and April 2019, almost 9 percent of the 1,146 hysterectomies conducted in Karnataka under AB-PMJAY were on girls aged under 15 years.
Despite all efforts to curb foul-play, the risk of unscrupulous private entities profiteering from gaming the system is clearly present in AB-PMJAY.
Uneven Performance
With India looking at achieving universal health coverage by 2030, getting the AB-PMJAY package available in the market for non-poor households to purchase, is the logical next step. Perhaps, there can be pilots in urban areas, which will also nudge the private sector towards a sustainable low-margin, high-volume business model in health care.
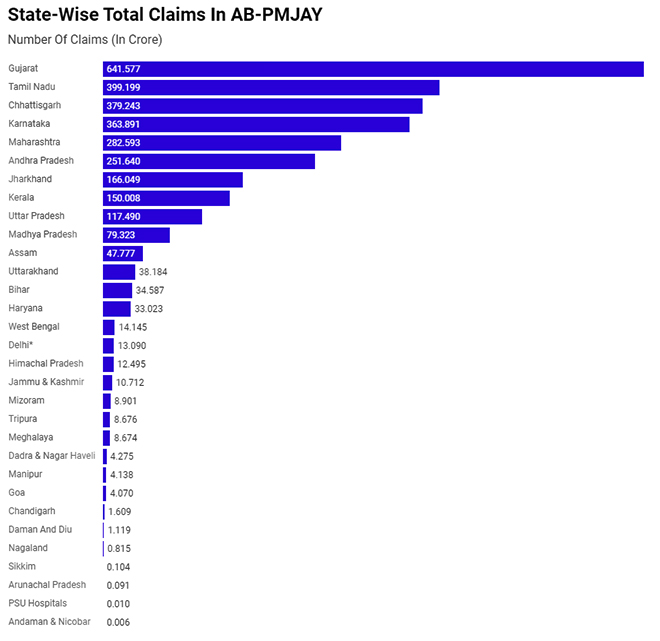
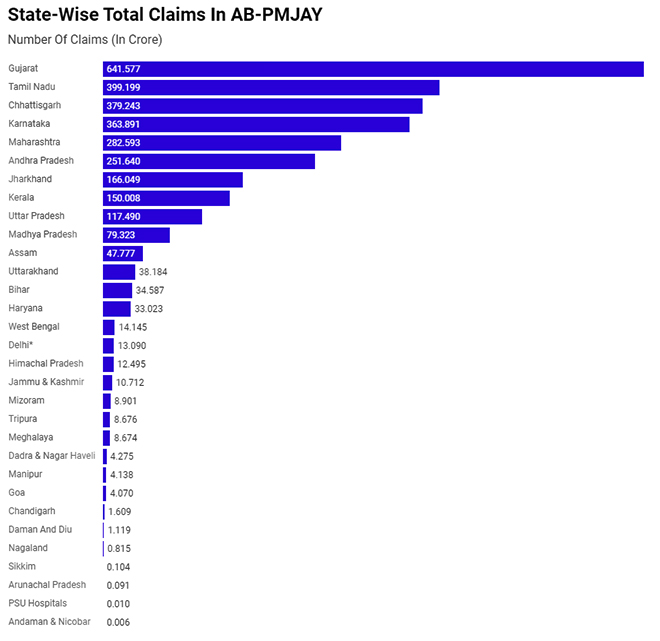 Data on Rajasthan, Telangana, Punjab, Odisha, Delhi, Puduchery not available. (* Delhi under NHCP)
Data on Rajasthan, Telangana, Punjab, Odisha, Delhi, Puduchery not available. (* Delhi under NHCP)
Source: Government of India, In Lok Sabha
Analysis of available disaggregated data in the public domain (from June 18, 2019) indicates that, barring a few states like Chhattisgarh in the case of AB-PMJAY, most top performers are the richer states. In the case of health and wellness centres (19,282 operational as on June 17, 2019), barring Uttar Pradesh that has 2,071 operational centres, all other top-five performers are richer states.
The government needs to ensure that benefits of Ayushman Bharat are distributed equitably between well-off and poorer states who may need it the most.
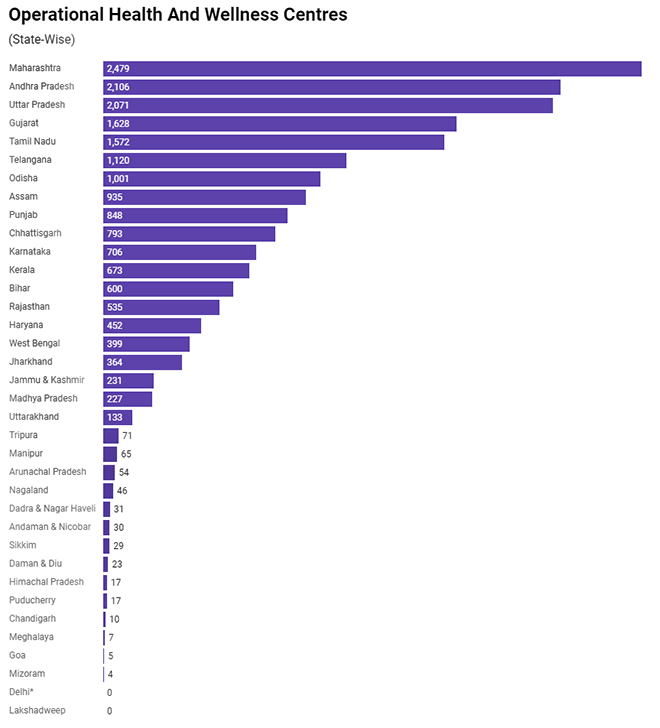 (* Centres in Delhi operate under National Health Mission)
(* Centres in Delhi operate under National Health Mission)
Source: Government of India, In Lok Sabha
The Next Steps
That National Health Authority, the apex body implementing AB-PMJAY is proactively conducting analysis and putting it in the public domain is indeed laudable. Soon, one would expect disaggregated real-time data to be available in the public domain for researchers to analyse, and make recommendations to plug gaps in the scheme. Similarly, state-level data on the status of health and wellness centres needs to be in the public domain too.
Recommendations made by the Finance Commission panel earlier this month of declaring healthcare a right and shifting health to the Concurrent List are inherently linked and are favourable to the success of Ayushman Bharat. The recommendations are also natural progress from the National Health Policy 2017, which made a logical case for regulation, recommended public sector strengthening, and explicitly supported the need for moving in the direction of a rights-based approach to healthcare.
Right now, the central government spends under one-third of the total government expenditure on health. If the current laggard states are to improve, the centre has to step up, both financially and programmatically. An enhanced role of the centre is impossible when health is still a state subject. As AB-PMJAY expands, the Finance Commission’s recommendation to shift health to the Concurrent List should be implemented so that along with more funds to be efficiently disbursed to the private sector, the centre has some regulatory teeth as well.
This commentary originally appeared in Bloomberg.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.




 Data on Rajasthan, Telangana, Punjab, Odisha, Delhi, Puduchery not available. (* Delhi under NHCP)
Data on Rajasthan, Telangana, Punjab, Odisha, Delhi, Puduchery not available. (* Delhi under NHCP)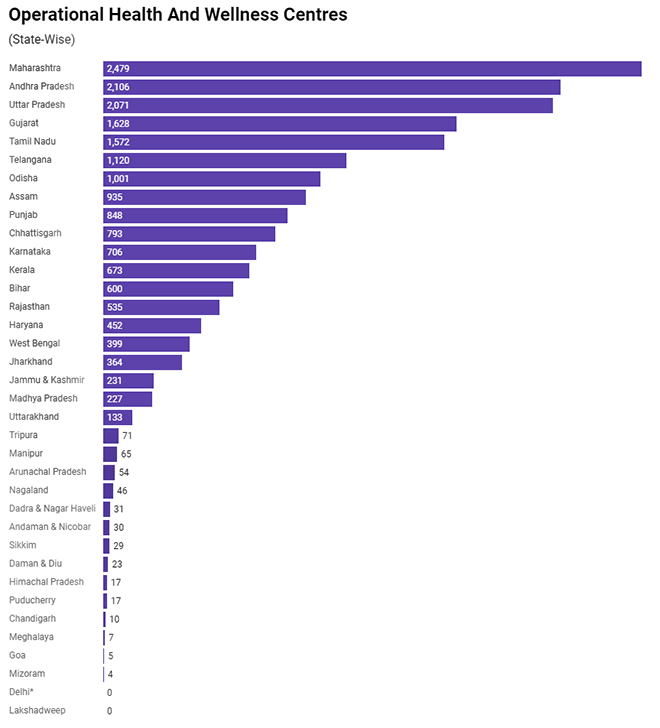 (* Centres in Delhi operate under National Health Mission)
(* Centres in Delhi operate under National Health Mission) PREV
PREV


