
The deaths of mothers and newborns caused by non-communicable and nutrition-related diseases pose a significant public health challenge in India, leading to numerous fatalities each year. These diseases, which can affect either the mother or baby, can be contracted during pregnancy, delivery, postpartum, or even during childhood, and may be difficult to detect early on, putting patients at risk of severe complications later on. To address this, early screening, detection, and diagnosis are crucial in reducing maternal and neonatal mortality. With the emergence of Artificial Intelligence (AI) and other digital technologies, there is potential for these tools to support maternal and neonatal healthcare in low-resource settings, although their development in this field is still in its early stages. AI has the capability of transforming maternal and child health in low and middle-income countries by supplementing conventional practices with advanced technology, thus improving the accuracy of diagnoses, increasing access to care, and ultimately saving lives.
< style="color: #0069a6">With the emergence of Artificial Intelligence (AI) and other digital technologies, there is potential for these tools to support maternal and neonatal healthcare in low-resource settings
< style="color: #163449">The current state of maternal and child health in India
The current state of maternal and child health in India is a complex issue with both challenges and progress. One of the main challenges is the high maternal and infant mortality rates. According to the latest SRS Bulletin, India's maternal mortality rate (MMR) was 97 deaths per 100,000 live births in 2018-2020, and the infant mortality rate (IMR) was 35.2 deaths per 1,000 live births in 2019-21. The Sustainable Development Goals (SDGs) have set a target to eliminate preventable deaths of newborns and children under five years of age by 2030, with a specific aim to lower neonatal mortality (NMR) to a minimum of 12 deaths per 1,000 live births and under-five mortality (U5MR) to a minimum of 25 deaths per 1,000 live births across all nations.
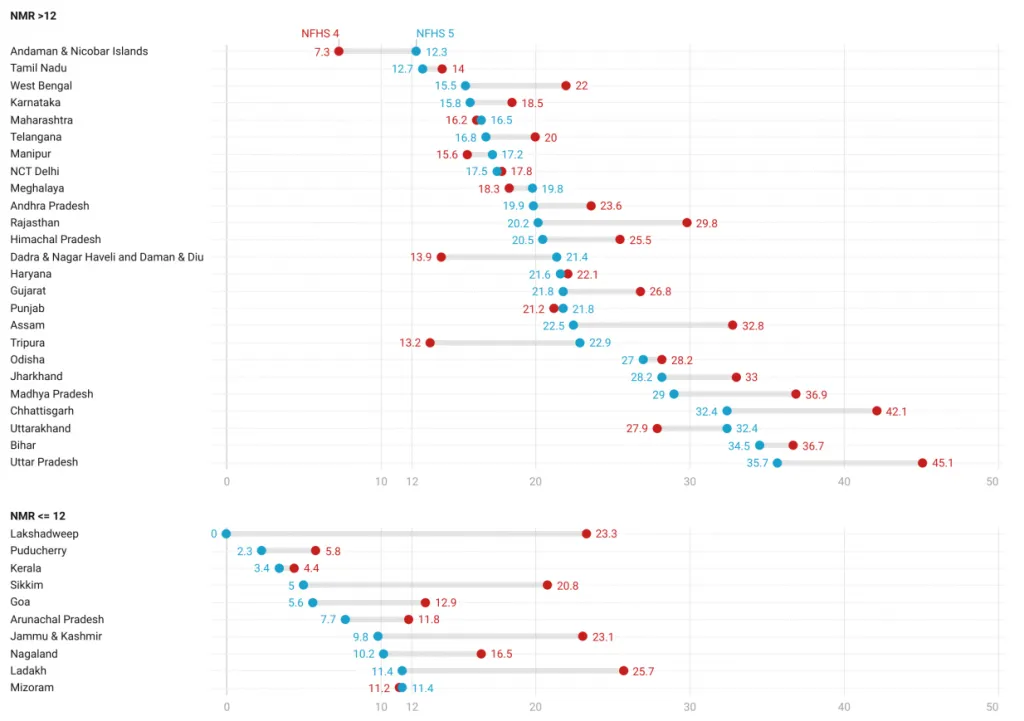
Fig 1. Neonatal mortality rate (NMR) across the states of India
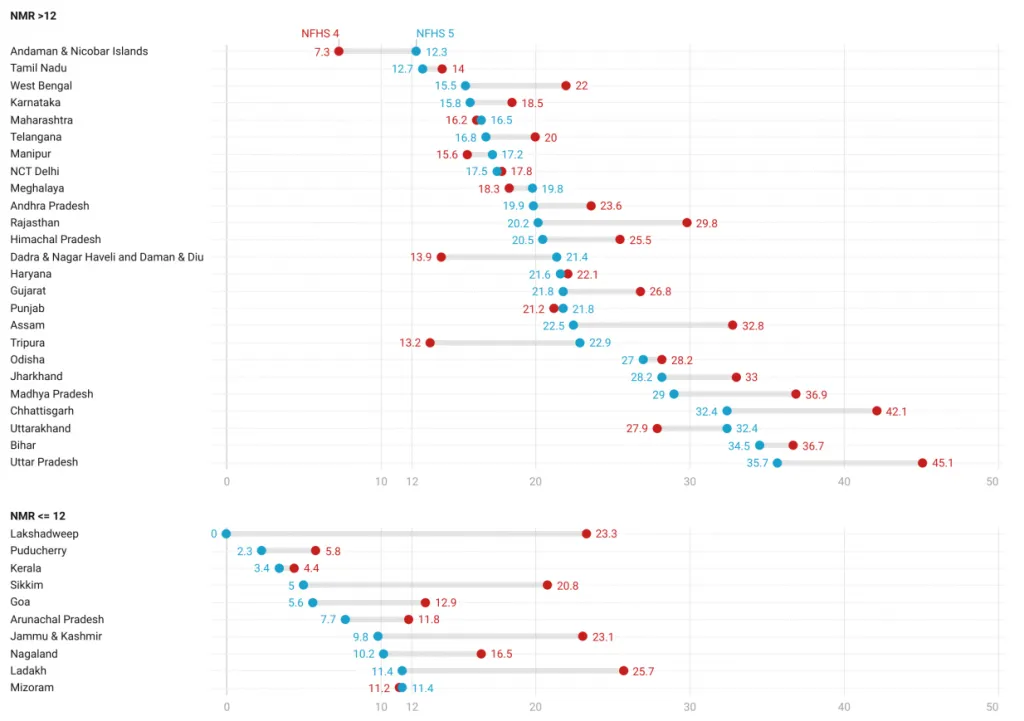 Source: National Family Health Survey, Round 4 & 5
Source: National Family Health Survey, Round 4 & 5
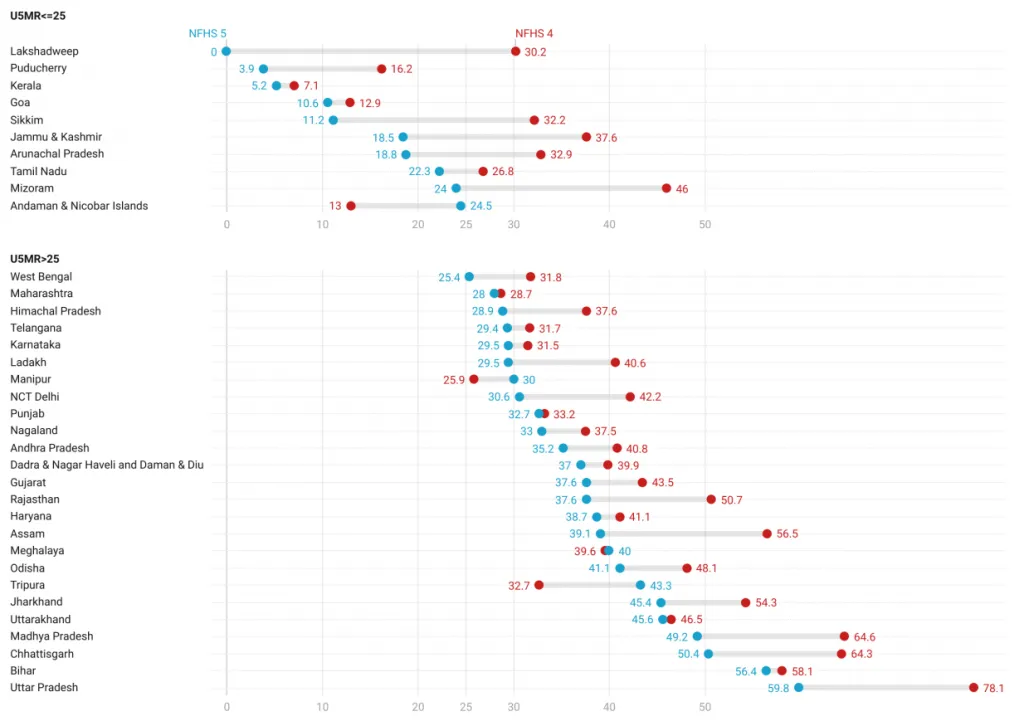
According to the latest National Family Health Survey (NFHS) data, the NMR and U5MR in India are 24.9 and 41.9 respectively. These rates are higher than the SDG targets and are a cause for concern. Figure 1 shows that the decrease in NMR varies across different regions, with only 10 states having an NMR lower than the SDG target. States with a high population such as Uttar Pradesh, Bihar, and Madhya Pradesh, which make up a significant portion of the country's population, are still behind in terms of progress. A similar trend is observed for the U5MR as well, as shown in Figure 2.
Fig 2. Under 5 mortality rate (U5MR) across the states of India
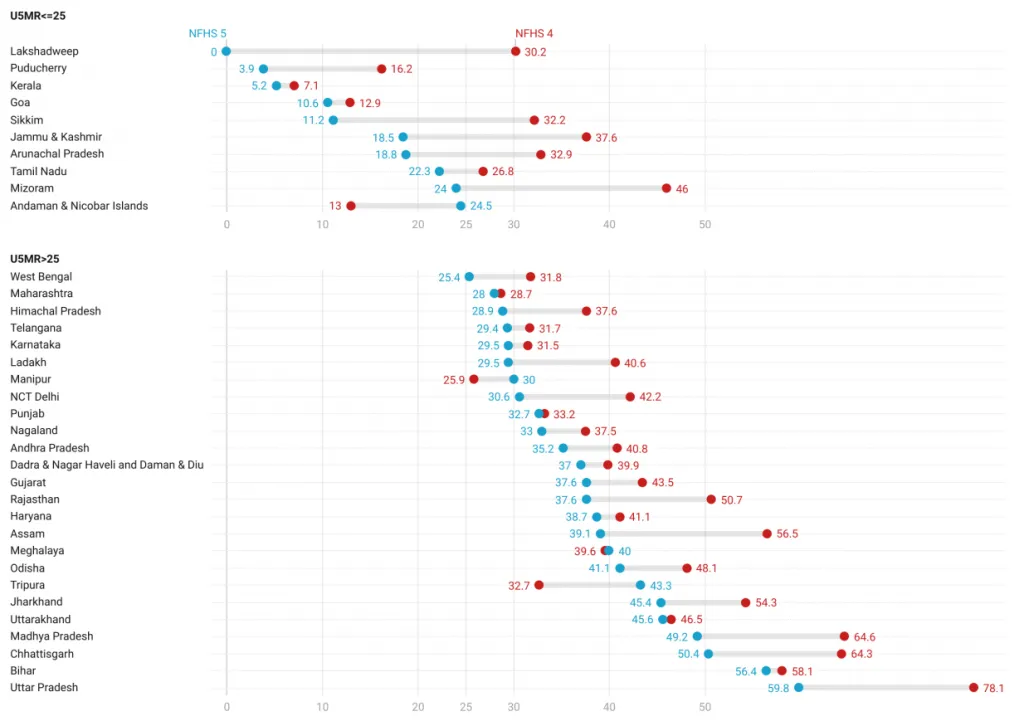 Source: National Family Health Survey, Round 4 & 5
Source: National Family Health Survey, Round 4 & 5
Another challenge is the lack of access to healthcare for many women and children in India. Many rural and remote areas lack basic healthcare facilities, and even when facilities are available, they may not be staffed with qualified healthcare providers. Additionally, cultural and societal barriers can prevent women and children from accessing healthcare.
Despite these challenges, there have been some positive developments in maternal and child health in India in recent years. The government has implemented several programs and policies aimed at reducing maternal and infant mortality, such as the Janani Suraksha Yojana (JSY) and the Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA) which provides cash incentives for pregnant women to deliver in health facilities and free health check-up respectively. There have also been efforts to increase the number of healthcare facilities in rural and remote areas and to improve the quality of care provided at these facilities.
In addition, India has also been working on using technology to improve maternal and child health. For example, telemedicine has been implemented in remote areas, and the government has also launched an application, RCH ANMOL, for tracking pregnant women, infants and children for their health, vaccination, and nutrition status. Other digital initiatives include the Draft Health Data Management Policy, Health Data Retention Policy, Unified Health Interface, and Health Facility Registry.
< style="color: #163449">Potential applications of AI
One of the most promising applications of AI in maternal and child health is in the area of predictive modeling. By analysing large amounts of medical data, AI algorithms can identify risk factors for maternal and fetal complications and predict the likelihood of certain outcomes. This can help healthcare providers to identify high-risk pregnancies early on and take steps to mitigate the risks.
Malnutrition is a major contributor to high maternal, neonatal, and infant mortality rates in India, with about 68 percent of child deaths being linked to malnutrition. Malnutrition is also responsible for lowering newborn immunity to infections and diseases. Predicting birth weight for newborns can aid doctors and parents to adopt putative measures such as effective utilisation of Nutrition Rehabilitation Centres (NRCs) pre-emptively. In low- and middle-income countries like India, low birth weight is a leading cause of death in the first month of life. Prematurity and low birth weight account for 45.5 percent of deaths during the first 29 days of a newborn in India. Accurately predicting the birth weight of a newborn using features of the mother would enable health workers to take remedial measures encompassing complete ANC check-ups, improvement in public facility-based delivery, providing iron supplementation, and uptake of balanced energy-protein diet among targeted pregnant mothers to bring down the IMR subsequently. Presently, around 18.2 percent of children reported having low birth weight. The model proposed by Hussain et. al. has the potential to be scaled and incorporated as a component into handheld applications used by health workers (ANMs). These applications would provide notifications about pregnant women who have a high likelihood of delivering a newborn with low birth weight. While a nationwide implementation might result in class imbalance issues, these can be easily resolved, making this module a crucial part of future reproductive and child health (RCH) applications.
< style="color: #0069a6">By analysing large amounts of medical data, AI algorithms can identify risk factors for maternal and fetal complications and predict the likelihood of certain outcomes. This can help healthcare providers to identify high-risk pregnancies early on and take steps to mitigate the risks.
Another area where AI can make a big impact is in the detection of fetal abnormalities. In LMICs, access to ultrasound technology is often limited, and the quality of images may be poor. By using AI to analyse ultrasound images, healthcare providers can improve the accuracy of diagnoses and detect abnormalities that may otherwise be missed. To maximise benefits, standardising the way images are taken, regulating the qualifications and performance of those who operate and interpret them, integrating clinical information, and providing feedback on performance will be essential.
In addition to its diagnostic applications, AI can also be used to improve access to care. Virtual care technologies, such as AI-powered chatbots and virtual assistants, can provide expectant mothers in LMICs with information and support. It has been demonstrated that sending personalised, timed voice messages about pregnancy via mobile phone can positively impact maternal healthcare practices and improve maternal health outcomes. However, more research is needed to determine if voice messaging is more effective at motivating behaviour change compared to text messaging, particularly in areas with low literacy rates. These technologies can triage patients and direct them to the appropriate level of care, helping to reduce the burden on overworked healthcare systems.
AI can also be used to manage and analyse large amounts of data collected from electronic medical records and other sources. By identifying trends and patterns in this data, healthcare providers can make more informed decisions and improve outcomes for mothers and children.
< style="color: #163449">Challenges
There are several challenges to using AI to improve maternal and child health in India:
- Data availability and quality: One of the biggest challenges is data availability and quality. AI relies on large amounts of data to train models, however, in India, there is a lack of data on maternal and child health, and the data that is available may be of poor quality. This can make it difficult to develop accurate and reliable AI-based solutions.
- Limited infrastructure: Another challenge is limited infrastructure. In many parts of India, there is a lack of basic infrastructure such as electricity and internet connectivity, which makes it difficult to implement AI-based solutions. This can be a particular problem in rural areas where access to healthcare is already limited.
- Ethical concerns: Ethical concerns are also a major challenge. AI-based solutions raise a number of ethical concerns, including issues around privacy, bias, and accountability. It is important to address these concerns to ensure that AI-based solutions are used in a responsible and ethical manner.
- Language and dialects: India has a wide variety of languages and dialects, which can make it difficult to develop AI-based solutions that are accessible to everyone. The lack of data in certain languages or dialects can make it difficult to develop accurate and reliable AI-based solutions that are tailored to the specific needs of different linguistic communities.
- Socio-Economic status: Socio-economic status of the population can be a big challenge, as people living in poverty may not have access to the technology and services provided by AI-based solutions.
Despite these challenges, the potential benefits of AI in improving maternal and child health in India are too great to ignore. It is important to address these challenges and to work closely with local communities and healthcare providers to develop and implement effective AI-based solutions that are relevant, accessible, and appropriate for the local context.
< style="color: #163449">Conclusion
AI has the capability of bringing about a substantial difference in maternal and child health in India. Nevertheless, it is crucial to keep in mind that these innovative technologies should not be utilised as a substitute for conventional healthcare practices, but rather as an additional tool. The integration of AI with the already existing healthcare systems would bring about the best results. It is also essential to involve healthcare providers and local communities in the development and implementation process of AI-based solutions. This way, the solutions can be made more relevant, accessible, and in line with the local context, thereby, maximising their positive impact.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.




 PREV
PREV



