-
CENTRES
Progammes & Centres
Location
Bridging maternal and child nutrition gaps is crucial to ending preventable deaths and securing global well-being

Image Source: Getty
This essay is part of the series: World Health Day 2025: Healthy Beginnings, Hopeful Futures
Maternal and newborn health disparities must be urgently addressed for children to have a brighter future, especially in low-resource settings where issues such as food insecurity, inadequate healthcare, and socioeconomic inequalities persist. These barriers undermine development and hinder sustainable growth. According to the World Health Organization (WHO), 287,000 women die annually during pregnancy or childbirth, 4.9 million children die of largely preventable causes before their fifth birthday, and there are 1.9 million stillbirths. The Lancet identifies maternal education as a key predictor of child undernutrition, even though its precise impact remains under exploration. Addressing maternal and child nutrition is pivotal in achieving Sustainable Development Goal (SDG) 2, which aims to eliminate hunger, enhance nutrition, and ensure food security. Additionally, bridging gaps in maternal and child nutrition is essential for achieving SDG 3, which promotes good health and well-being for all.
Addressing maternal and child nutrition is pivotal in achieving Sustainable Development Goal (SDG) 2, which aims to eliminate hunger, enhance nutrition, and ensure food security.
Poor maternal health, often linked to malnutrition, is a primary contributor to complications during pregnancy, childbirth, and infancy. Research highlights that suboptimal dietary intake is a significant cause of poor maternal nutrition, leading to adverse outcomes for both mothers and children. Barriers such as food unavailability, economic hardship, lack of nutritional counselling, food taboos, and gender norms restrict access to proper nutrition.
Gender inequality significantly affects maternal and neonatal health, particularly in low-income countries. Women’s limited decision-making power within the household and the community often results in delayed or inadequate access to essential healthcare services. A recent meta-analysis underscores the value of investing in women's economic empowerment in low and middle-income countries. Economic empowerment programmes have been shown to positively impact various human development indicators, both monetary and non-monetary. These programmes enable beneficiaries to increase investments in health and education, ultimately leading to improved physical health outcomes.
Economic empowerment programmes have been shown to positively impact various human development indicators, both monetary and non-monetary.
Furthermore, interventions to improve maternal diets could include food-based programmes, behaviour-change communication, and nutrition-sensitive agriculture. Malnutrition is another factor impacting mental health, contributing to postpartum depression. According to recent research, a mother's mental and emotional health is integral to the child’s development. Poor maternal mental health can disrupt caregiving, creating a cycle of disadvantages for both mother and child.
In many regions, pregnant women face nutritional deficits due to limited access to nutrient-rich food and supplements, heightening the risk of pregnancy complications. Food insecurity exacerbates maternal and child malnutrition, aggravated by rising food prices, ongoing conflicts, and climate change. A cross-sectional study across 94 Low and Middle-Income Countries (LMICs) found an overall stunting prevalence of 32 percent among children aged 0–59 months. The study noted that older children showed higher stunting rates, likely due to prolonged exposure to undernutrition and recurrent infections.
Therefore, programmes promoting exclusive breastfeeding, social behaviour change initiatives, and micronutrient supplementation for expectant mothers are crucial to improving maternal and child health outcomes.
Proper maternal nutrition is vital in determining birth outcomes and children’s long-term cognitive and physical development. A global systematic review identified several key factors hindering improvements in maternal nutrition in LMICs. These include inadequate household food availability, financial constraints, lack of knowledge about appropriate weight gain and dietary intake during pregnancy, and insufficient dietary counselling. Addressing these issues is essential for improving maternal healthcare in regions with high malnutrition rates.
Many initiatives have made significant strides in maternal and child health by providing resources and advocating for stronger healthcare policies.
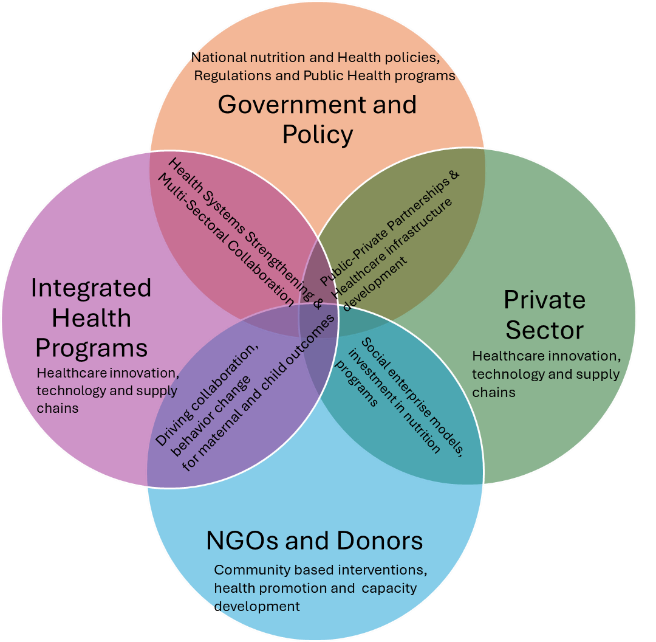
A long-term, sustainable solution requires a multi-sectoral approach that combines economic development, education, healthcare, and agriculture. Many initiatives have made significant strides in maternal and child health by providing resources and advocating for stronger healthcare policies. In regions with limited resources, sustainability is key to ensuring long-lasting change.
Social safety nets, such as food aid and cash transfers provide immediate support to vulnerable populations, particularly during crises. A systematic review also found that including mothers in comprehensive care packages for small and nutritionally at-risk infants under six months could significantly improve health outcomes.

Despite the availability of policies and programmes to improve maternal and child health, many fail to reach vulnerable populations due to implementation gaps. According to a study, key challenges in low-resource settings often include inadequate infrastructure, limited resources, and weak monitoring and evaluation systems. To address these, policies must prioritise inclusiveness and sustainability, be adaptable to local contexts, and involve strong community engagement. Effective implementation requires coordinated efforts across stakeholders to ensure resources reach the last mile.
Furthermore, improving maternal health outcomes also requires robust healthcare systems that provide adequate prenatal care. Governments and investors must prioritise funding maternal health programmes and enhance their focus on food security initiatives. A recent study reveals that women from low-income backgrounds face higher maternal mortality rates, primarily due to limited access to quality healthcare, inadequate nutrition, and poor living conditions. In rural areas, community health workers play a critical role in providing tailored advice based on local customs, promoting nutrition monitoring, counselling on infant care, and encouraging exclusive breastfeeding. By identifying high-risk groups, data-driven strategies can help implement targeted interventions that meet the needs of vulnerable populations. The prevalence of malnutrition can be significantly reduced when pregnant women and their families are educated about healthy eating, the importance of breastfeeding, and balanced infant diets.
Supporting agricultural projects and food delivery systems that guarantee access to nutritious food for pregnant women is imperative.
Community education on newborn care and maternal nutrition is essential for improving health outcomes. Supporting agricultural projects and food delivery systems that guarantee access to nutritious food for pregnant women is imperative. This can be achieved through subsidies, improved agricultural infrastructure, and policies stabilising food prices. These programmes are particularly effective when they respect the social and cultural contexts of the communities they serve. Local community-driven programmes integrating familiar foods into dietary recommendations and collaborating with trusted community leaders often see higher participation rates and more lasting outcomes. These grassroots initiatives ensure that nutritional interventions are culturally appropriate, leading to better acceptance and a sustained behaviour change.
Global cooperation is not enough. It is imperative to close the gaps in maternal and child nutrition. The combined efforts of international organisations, governments, and local communities are crucial to addressing the root causes of malnutrition, improving food security, and strengthening healthcare systems. By focusing on sustainable, long-term solutions such as improving agricultural infrastructure, providing targeted healthcare, and fostering community-driven education programmes, we can ensure that vulnerable populations have the resources they need to thrive.
The combined efforts of international organisations, governments, and local communities are crucial to addressing the root causes of malnutrition, improving food security, and strengthening healthcare systems.
However, the real challenge is transforming these initiatives into widespread, scalable actions that create lasting change. The key lies in collaboration across all sectors working in tandem. Together, they can build a holistic, interconnected system where each part supports and strengthens the other. With focused investments, a commitment to immediate relief, and long-term sustainability, we can ensure that no mother or child is left behind.
Through global solidarity and a unified approach, a healthier, more prosperous future for mothers, children, and upcoming generations can be forged. Now is the time to act, as every healthy start to life contributes to a brighter future, both for the individual and for the entire world.
Rohini Saran is the Head of Key Verticals at Vedanta Group
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

With 18 years of experience, Rohini Saran leads nutrition-sensitive programs focused on maternal and child health across diverse sectors. Expertise in strategic communications, policy advocacy, ...
Read More +