-
CENTRES
Progammes & Centres
Location
The eradication of AIDS by 2030 appears a formidable challenge as social barriers stand in the way of equitable access to healthcare

In the policy domain, perceiving crisis through an intersectional lens can comprehensively tackle issues by recognising and addressing the root causes. The World AIDS Day (1st December) theme ‘Equalise’ proposes the same through the creation of global solidarity to eliminate structural inequalities that halt access to HIV care. It calls for testing and prevention by strengthening the national public health systems through interconnected and multi-sectoral efforts. The transformative nature of this integrated approach to health security can enhance the current efforts in eliminating AIDS by 2030 by realising the SDGs. The current trends all over the world posit the question of the possibility of achieving the goals by 2030. The progress achieved through all these years was halted—many goals have also seen regression—due to the difficulties posed by the pandemic, coupled with instability triggered by multiple economic and humanitarian crises.
An increase in gender-based violence and being out of school and other contributing factors have increased the vulnerability and exposure of women and girls to HIV.
Structural inequalities during the pandemic, especially in low- and middle-income countries added to the existing vulnerabilities at all levels. An increase in gender-based violence and being out of school and other contributing factors have increased the vulnerability and exposure of women and girls to HIV. Around 54 percent of people who are infected with HIV are girls and women. While 80 percent of girls and women of above the age of 15with HIV are able to access antiretroviral treatment (ART), data shows that only 70 percent of the boys and men over 15 with HIV are accessing the treatment which makes us question the accessibility factor. A deeper look into this may bring forth the patriarchal norms acting as causation for harmful masculinity and non-adherence to safe sex and HIV test.
During the past two decades, expansion in HIV testing and treatment prevented 16.6 million deaths. Interventions among pregnant women living with HIV through ART drastically reduced infection among children by around 54 percent. A comparison of these developments in Asia, Latin America, African countries, and eastern European countries, however, show unequal progress. Recommendations in the report of the UN Secretary-General view potential solutions from an inequality lens which can tackle the root causes of infections and enhance prevention strategy by eliminating legal and policy barriers affecting the key populations.
In the Indian context, the HIV prevalence has decreased 0.55 percent in 2000 to 0.21 in 2021. Prevalence rate indicates the proportion of the population that has a health event at a point in time or at a specified period of time is different from incidence rate as the latter measures the frequency at which a new health event occurs on a particular time frame. The latest NACO Fact Sheet suggests that the adult HIV prevalence rate is higher among men than women. At state levels, the HIV prevalence rate is high in three northeastern states, the highest being Mizoram (2.7 percent), Nagaland (1.36 percent), and Meghalaya (.42 percent). In comparison with previous years, the prevalence rate shows a continuous increase in these states except Nagaland. The prevalence rate is high in the southern states of Andhra Pradesh (.67 percent), Karnataka (.46 percent) and Telangana (.47 percent) as well.
Prevalence rate indicates the proportion of the population that has a health event at a point in time or at a specified period of time is different from incidence rate as the latter measures the frequency at which a new health event occurs on a particular time frame.
A number of states and Union Territories (UTs) have recorded an adult HIV prevalence rate higher than the national values (.21 percent). These states are Delhi (.31 percent), Goa (.31 percent), Haryana (.22 percent), Maharashtra (.33 percent), Punjab (.28 percent), Tamil Nadu (.22 percent) and Puducherry (.31percent). HIV incidence rate is high in the states of Mizoram (1.31 percent), Nagaland (.51 percent), and Meghalaya (.37 percent). The incidence rate in Meghalaya is showing an increasing trend. These states also show a relatively higher prevalence of Injecting Drug Users (IDU). States like Delhi (.14 percent), Karnataka (.04 percent) and Tripura (.13 percent) show a minor increase in the incidence rates in comparison with the previous year. The HIV burden, as an absolute number, is highest in Maharashtra (3.94 Lakh) followed by Andhra Pradesh (3.21 Lakh) and Karnataka (2.76 Lakh). It shows a general decline across the years in these states. Mizoram, Nagaland, Meghalaya, Karnataka, Andhra Pradesh, and Telangana require special attention in addressing the prevalence of HIV among adults. Similar to the global level, HIV detection got hampered due to the pandemic. However, data suggest a steady decline in the spread of HIV in most states. The percentage change in annual new infections is increasing in some states and union territories of Mizoram, Dadra and Nagar Haveli, Sikkim, Andhra Pradesh, Meghalaya and Tripura, while other states show a declining trend (Refer Figure 1.)
Figure 1: Percentage change in Annual New Infections by State/UT,2010-2021
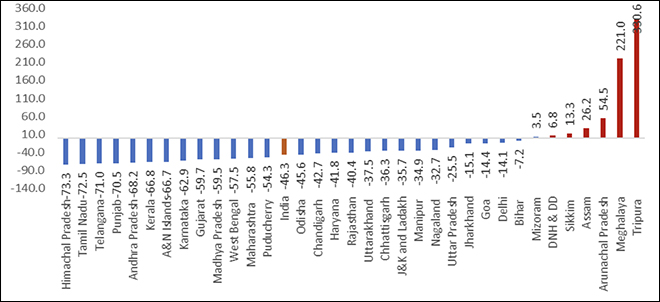 Source: NACO India HIV estimates Fact Sheet
Source: NACO India HIV estimates Fact Sheet
Curbing of infection lies at the heart of India’s National AIDS control programmes, and other collective efforts in gathering public response through civil society organisations. UNAIDS data show that 2.4 million people in India live with HIV and about 65 percent are receiving ART. Nearly 59 percent of the boys and men over 15 years with HIV are receiving ART while 70 percent of the girls and women in the same age group with HIV are receiving the same. Given the challenge of access, a joint effort to bridge the gap by addressing the root cause of social barriers is crucial. UNAIDS aims to achieve 95-95-95 percentage rates for HIV testing, treatment, and viral suppression by 2025. India has achieved progress across the years in certain areas of intervention as shown in
Figure 2: State/UT-wise progress on 95-95-95, 2018-19 to 2021-22
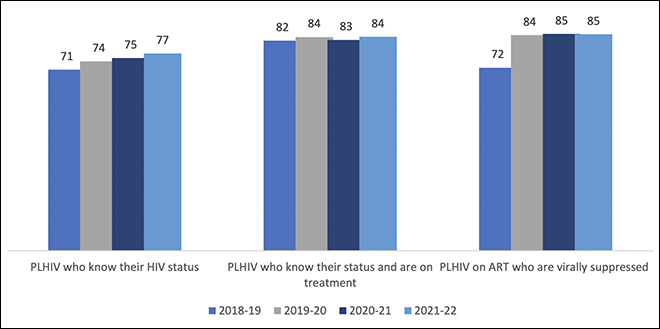 Source: NACO India HIV Fact Sheet | Note: PLHIV means People Living with HIV
Source: NACO India HIV Fact Sheet | Note: PLHIV means People Living with HIV
India’s efforts in assisting the international community through production and distribution of generic HIV medicines holds immense significance. One of the pertinent developments in legal and policy development with reference to recognition of constitutional rights of sex workers right to life, liberty, and dignity would open door for safe access to HIV care for the affected key population. The Supreme Court ruling in Budhadev Karmaskar versus the State of West Bengal, Criminal Appeal No.135 in 2022 appealed for protection and support for those facing sexual violence and survivor-friendly practices in the sector. Further, it reiterates the need to ensure awareness about legal rights of the sex workers. These legal decisions can achieve policy goals through community-led efforts and eradicate stigmatisation in accessing healthcare as well as increase social protection. In the public health system, community-led integrated projects like Ashodaya Pre-Exposure Prophylaxis (PrEP) demonstration project for female sex workers in Mysore are considered to be efficient and successful. These interventions were successful due to mobilisation and outreach at community levels. A national expansion of these interventions to key populations is essential to achieve the elimination of AIDS by 2030 as committed in the United Nations General Assembly High-Level Meeting on ending AIDS.
Inequalities stand in the way of realisation of the recommendations like equitable access to medicines and health technologies. UNAIDS report suggests that in countries such as Ethiopia, Cameroon, and Zambia, the gap between rich and poor in terms of viral suppression is unacceptably high.
The UN Secretary General’s report recommends a cohesive list of actions to be followed to end social barriers to achieve the goals by 2030. One among them is community-led responses by fully funding and engaging with the people living with HIV and key populations. The lack of funding from bilateral donors is a major barrier to efficiently implement this. Data shows that the United States (US) funding has reduced by 57 percent during the past decade. Inequalities stand in the way of realisation of the recommendations like equitable access to medicines and health technologies. UNAIDS report suggests that in countries such as Ethiopia, Cameroon, and Zambia, the gap between rich and poor in terms of viral suppression is unacceptably high.
Bridging these gaps may require a substantial amount of time and therefore, the eradication of AIDS by 2030 appears a formidable challenge. Prophylaxis options are available in high income countries, and expansion of this to key populations across the globe is a need at the moment. In sum, a concerted effort across legal and policy domains along with community-led responses to foster gender equality and sustainable financing through global partnerships is essential to tackle the inequalities and impediments in question. Moreover, as the theme suggests, efficaciousness of interventions will depend on the ability in improving equity and adopting a gender transformative, rights-based and intersectional approach in recognising and addressing inequalities.
Adithya M (Masters in Public Policy, NLSIU) is an intern with the ORF Health Initiative.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.