
“Test, test, test…” was the simple message delivered by the beleaguered WHO Director-General Dr. Tedros, 5 days after announcing coronavirus as a pandemic. Since then, Covid19 cases have reached 5 million with more than 300,000 deaths, globally.
While researchers and drug makers around the world have made unprecedented headway, it is estimated that we are around 12 to 18 months away from a vaccine being available for large scale deployment. In the absence of a medically approved treatment or vaccination, the best strategy to counter the pandemic is prevention, which is dependent on detection and isolation along with physical distancing measures.
Testing has indeed been the mainstay in the fight against the Coronavirus pandemic as, beyond the obvious benefits, it also provides insights into the spread of the disease and its evolving and locality specific characteristics. As countries phase-out of the Covid19 lockdowns and restart their respective economies, testing seems to be the most powerful measure to ensure safety of the citizens in a post-lockdown world.
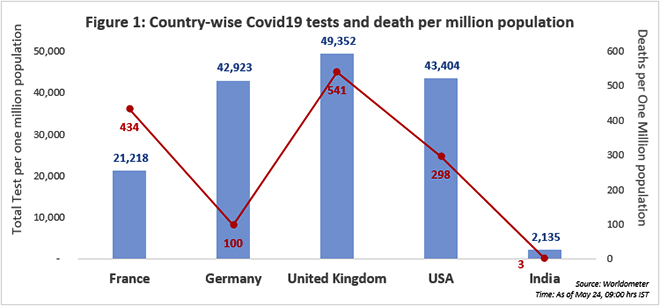
It is therefore not surprising that countries around the world have ramped up testing. One of the top Covid19 testers in the world, Germany has shown immense prowess in keeping the case fatality rate low with early and aggressive testing. By testing and contact tracing much earlier than its European counterparts, Germany was able to do better in the fight against the pandemic. Some argue that the high number of tests per million population has ensured that the deaths per million population has remained relatively low for Germany.
However, the UK, with a higher test per million population rate, constitutes Europe’s highest death toll. The difference, it seems, was in the timing. While Germany was proactive and used testing as a tool for prevention, UK started testing aggressively after considerable spread of the virus.
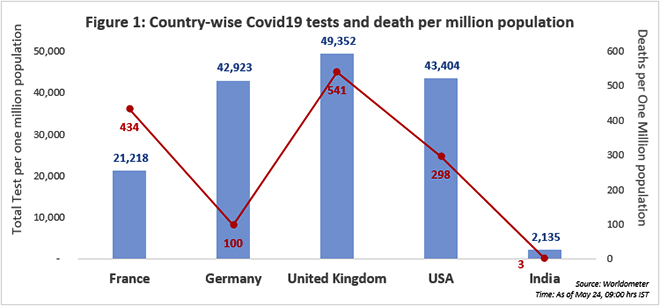
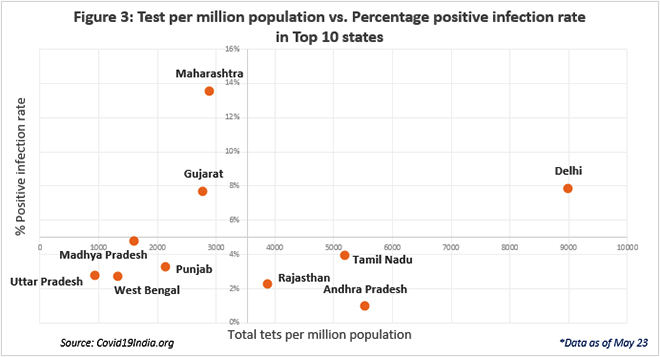
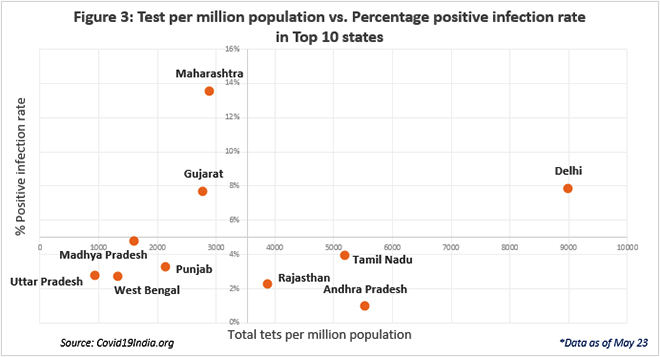
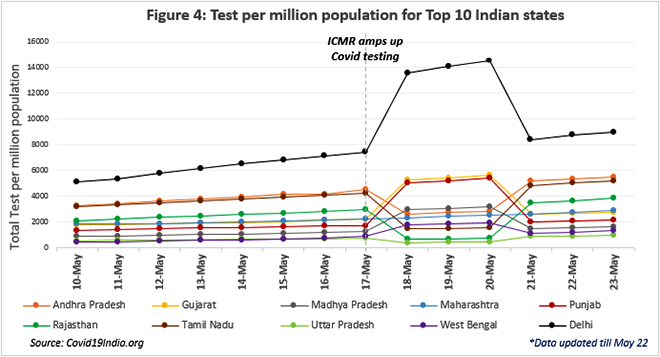
By May 20th, India’s reported Coronavirus cases had surpassed 100,000, making it the eleventh most infected country in the world. But, of the eleven most infected countries, India’s testing rate is the lowest. The past week saw an increase in Coronavirus testing in India to up to 100,000 per day. However, given the large population base, India’s test per million population remains very low and what is more worrisome is, that with increased testing, India has also witnessed an increase in the percentage of positive infections pointing to a larger asymptomatic spread.
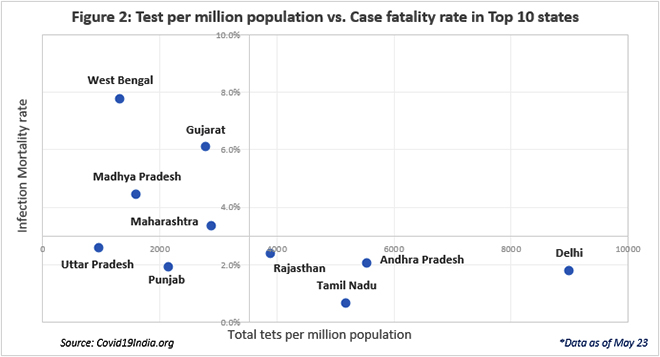
Surprisingly, while cases continue to rise, the case fatality rate in India remains low at 3 percent. The low mortality rate in India could be a result of the virus mostly affecting the working-age populations till now. Another puzzling observation is India’s relatively low test positivity rate, suggesting a limited spread of the virus, even within the smaller testing landscape
Trends from across the world have revealed that higher testing rates by themselves are unable to prevent deaths. This is observed in the case of USA, Italy and even within India, in Maharashtra. Like in the case of Germany, even the Kerala experience reveals that timely testing is most crucial in fighting this virus.
Kerala initiated early testing, intense contact tracing and isolation efforts. It was successful in mapping the extent as well as controlling the spread of the pandemic, with as low as 795 cases and 5 deaths, thereby ‘flattening the curve’. On the other hand, Maharashtra has one of the highest numbers of tests being conducted in any state in India. However, the testing data has only been successful in mapping the spread of the virus, rather than curtailing it. It was not aggressive with its testing programme early enough. At crossing 500 cases, Maharashtra’s test per million lagged behind at 132, while Kerala had already reached 883 tests per one million people tested when it crossed the 500 mark.
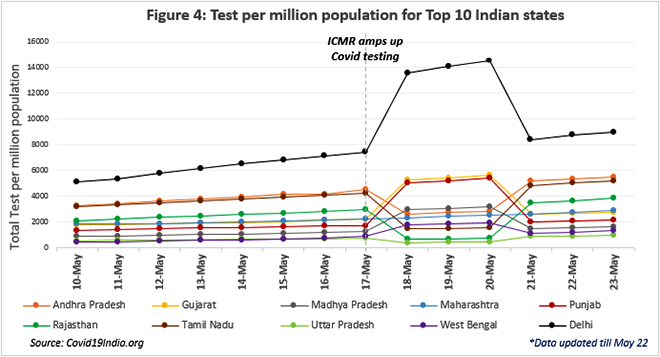
As India increased testing, Delhi witnessed a visible but temporary surge as well. Reports suggest that Delhi’s testing labs have been overwhelmed, leading to a long wait list even for serious and critical cases. Testing labs in the capital have expressed distress over increased administrative work, need for more staff and an overburdening of facilities.
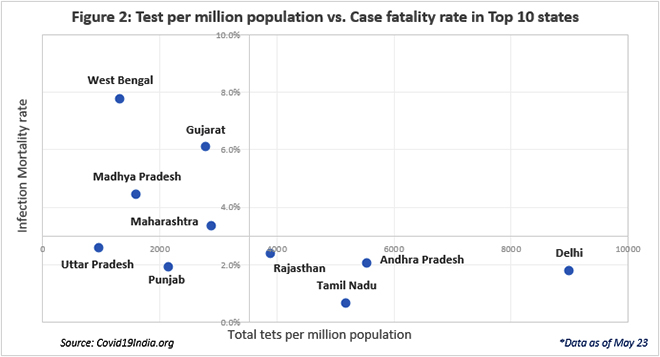
While Gujarat has observed an increase in testing rates, it has been accompanied by an increase in rate of positive infections and a higher fatality rate. Gujarat has conducted a relatively lower number of tests, with reports suggesting that the state may not be interested in mapping the real spread of the virus. This is borne by the fact that while testing rate in Gujarat has remained consistent, it has reduced in hotspots like Ahmedabad. This is a matter of grave concern.
West Bengal has the highest case fatality rate, with one of the lowest testing records. In addition to low testing, the high mortality rates in West Bengal have been attributed to the social stigma associated with the virus, which acts as a deterrent to a timely identification and treatment. While initially, the low tests could be attributed to the lack of testing laboratories or faulty testing kits, experts suggest that such issues have been resolved and that the state may be holding back for other reasons. Because of its initial delay, it is now imperative for West Bengal to reach out to communities to test the population to understand the dimensions of the pandemic.
One of the better performing states, with below average case fatality rates and above average testing, Tamil Nadu witnessed a mysterious but momentary fall in the test per million population. Tamil Nadu, which remains among the top Covid infected cases, has been testing at a significantly higher rate when compared with other states, successfully maintaining the lowest fatality rate of 0.7 percent.
In Contrast, Madhya Pradesh, with an increasing number of cases and high fatality rate, has observed one of the lowest rates of testing per million population. Recent reports suggest penetration of the infection in 52 of Madhya Pradesh’s 55 districts. The state seems to be struggling with shortage of testing kits and laboratories. Moreover, patchy leadership within the state has further hampered ability to correctly diagnose and prevent the spread.
While much of India’s Covid journey started more modestly and was controlled by the lockdown, the recent deluge of cases and fatalities have left the country with no choice but to ensure broad level testing of symptomatic people, asymptomatic people at risk, and people who the positive cases may have come in contact with. In order to resume social and economic life, the importance of testing cannot be overstated. Given the size and resource constraints, India will have to be strategic with testing even as it needs, to now, go way beyond the cautious expansion strategy that the Indian Council of Medical Research has followed. The pace of spread will soon outrun the ICMR roadmap.
Solutions towards a new normal
As India prepares itself to face the grim realities of the ‘With-Covid’ world, testing must become a norm. Taking into consideration the unique nature and spread of the virus, India requires the implementation of a customised sub-state level strategy. Global best practices highlight 5 key areas that India can leverage to successfully navigate this new normal:
- As the first line of defense, testing must become a part of our daily lives. Once the virus begins to subside, we must incorporate additional safety protocols in areas where a large number of people congregate. Large scale detection and screening are necessary to commence movement throughout the country, requiring an elaborate system of testing across all major facilities and transport hubs. Technologies such as thermal imaging cameras, rapid tests at airports, railway stations and bus depots are required to avoid resurgence.
- While India was lucky to avoid the high cost of low testing in terms of fatalities, it is faced with the economic damage from the prolonged lockdown. It has been estimated that restarting the economy in urban areas requires 21 tests per 1000 people per day, until vaccination is available. Currently, with 100,000 daily tests, India can only achieve 8 per 1000 people. A possible solution is the use of periodic antibody tests to effectively map the spread of the virus within key economic zones, followed by RT PCR testing to facilitate contact tracing, and isolation. Resuming economic activity necessitates a ‘selective and continued’ approach, focusing intensely on regions that contribute most to India’s GDP, which also happen to be the hotspots of infection.
- Another hotspot for Covid infections is hospitals. The contagious nature of the virus has burdened health facilities, infected medical professionals and hindered multiple non-Covid medical procedures. As we move ahead, a ‘test at home’ approach is necessary so only the essential cases are taken to hospitals. This also presents an opportunity for Indian biomedical organisations to produce cost-effective and highly accurate testing kits, for India and for the world under the ‘Make in India’ initiative.
- With inadequate health infrastructure, India requires an innovative approach to accelerate testing, while reducing the burden on laboratories. Pooled testing has presented a window of opportunity, especially in highly populated or rural areas in states such as Uttar Pradesh. Successfully incorporated in countries like Germany, pooled testing assists in increasing the testing rates substantially, while also identifying hotspots and tracking the spread of the virus. With the growing number of cases, expansion of pooled testing kits and expertise can help India in successfully phasing-out lockdowns, while keeping infections under check.
- India’s high population density leads to a higher probability of spread. Slums such as Dharavi in Mumbai have witnessed a quick escalation of cases, leaving authorities and medical professionals struggling. Once a certain threshold of people is infected, certain areas with high population density should consider reverse quarantine. This entails the protection of the higher risk population by keeping them in separate quarantine zones. After the high-risk population is safely repositioned, in areas where home-based quarantine is less effective, the policy should shift to keeping 'infected in' the containment zones, rather than keeping ‘infected out’. As economic activity progresses, with the help of periodic testing and aggressive community surveillance, restriction of infected people within strict containment zones will be necessary.
As we approach 10 weeks since the WHO formally announced the pandemic, there is little justification in not having strategies for testing, tracing and isolating. It has a safety dimension and it has a most urgent economic consideration. Indian states, cities and the central government must prepare and declare important protocols on this vital issue that will define our ‘with COVID’ existence for some time to come.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.




 PREV
PREV


