Today, 7
th April, is celebrated as World Health Day since 1950 to create global health awareness. This year the theme ‘Building a fairer, healthier world’ calls for action to eliminate health inequities and create an environment conducive to good health. ‘Health for all’ is a critical component in the United Nations' 2030 agenda for Sustainable Development Goals. The
Countdown to 2030 focuses on ‘universal health coverage, social, and environmental determinants, and in-country inequalities to ensure no one gets left behind’.
India is committed to providing
universal health coverage to ensure that everyone, everywhere, should have access to essential healthcare services without facing financial hardship. ‘
Ayushman Bharat’, India’s Health Mission launched in 2018 provides for free access to healthcare and financial risk protection to poor and vulnerable families through its two complementary schemes, Health and Wellness Centres and Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PMJAY).
Some of the key
health challenges in India are limited access, insufficient availability, sub-optimal quality of health services, and high out-of-pocket expenditure (OOPE).
Health expenditure due to OOPE, contributes 8.1 and 7.9 percent in rural and urban poverty respectively. A
study based on the National Sample Survey Data (1994–2014) estimates about 55 million people in India pushed to poverty due to OOPE on healthcare—among them 38 million fell below poverty line due to medicine purchases alone.
Survey data (2017–18) on household consumption related to health indicates just about 10.2 percent rural and 9.8 percent urban from poorst wealth quintile having any kind of health insurance. A
recent research indicates increase in the number of poor by 75 million in India due to pandemic-driven recession accounting for nearly 60 percent of global poverty increase. Comparing to China, the largest impact was in the low-income group and poverty remainedunchanged.
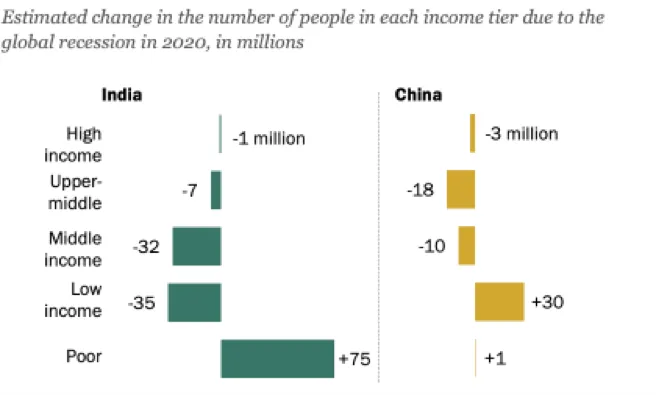
Figure 1: Estimated number of people as per wealth quintile due to pandemic recession.
Source: Pew Research Center
According to the
Global Burden of Disease study, India has improved in healthcare access and quality (HAQ) since 1990, however, it ranks at 145 among 195 countries on HAQ index. The data indicates widespread disparity among states with Uttar Pradesh and Assam scoring lowest (35.9) as compared to Kerala (68.9).
Estimates based on Global Health Database indicate a threefold increase in OOPE for India by 2050 (Figure 2). The figure 3 show a statistically significant increase (26.9 in 1990 to 42.1 percent in 2010) in provision of effective and essential health services in India, as compared to past decade with insignificant change.
*Based on past growth
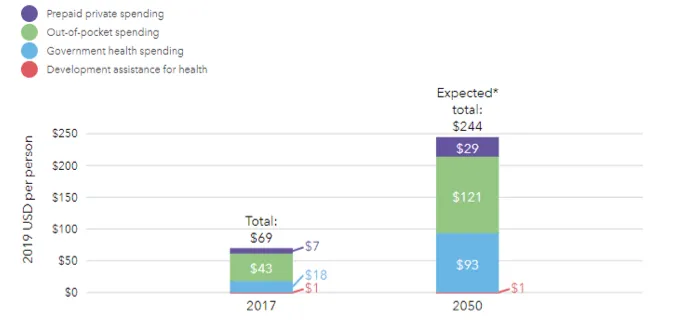
Figure 2: Spending on Health by India – now and in the future.
Source: IHME
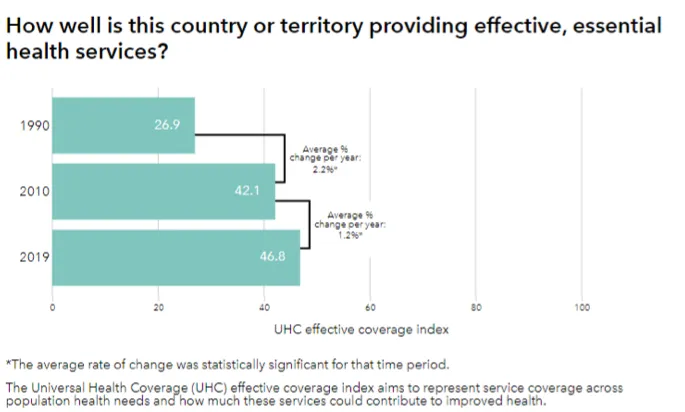
Figure 3: The Universal Health Coverage index for India
Source: IHME
India’s diseases burden is changing from non-infectious to lifestyle diseases. In recent decade, non-communicable diseases (NCDs) have caused significant threat to public health, with top 3 causes of deaths attributable to NCDs (Figure 4). The reasons range from genetic predisposition, unhealthy eating to sedentary lifestyle.
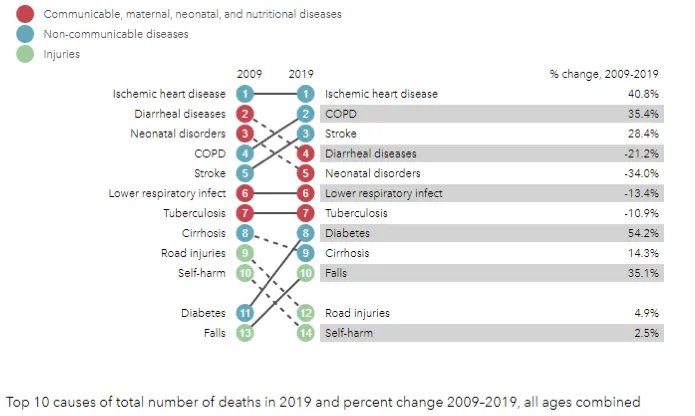
Figure 4: Top 10 causes of death for India
Source: IHME
Despite progress in delivery of maternal and child health services, the infant (
32/1000 live births) and maternal mortality (
113 per 100,000 live births) rate remain high for India.
Evidence suggests vast inequality in reporductive, maternal, and child health services coverage amongst the poorest and rural residents.
Studies indicate inequality in many maternal and child health indicators with
disadvantaged group getting low healthcare access and coverage leading to worsening of health outcomes.
Analysis of the 5
th round data of National Family Health Survey released for 21 states/UTs indicate mixed trends for health and nutrition. On one hand, we see worsening trend for nutrition indicators, on the other,
health outcome and health service delivery have shown improvement. Almost all states/UTs have performed poorly in one or more indicators of malnutrition—stunting, wasting, underweight and overweight along with increasing anemia prevalance. However, the health indicators—proportion of institutional births, total fertility rate, and full immunization coverage have shown consistent increase across many states. A uniform improvement in infant mortality rate (IMR) and under five mortality rate has been observed across many states. As
data indicates improvement in some of the nutrition-sensitive indicators—access to toilet, safe drinking water, or women empowerment in terms of education or owning a bank account, the gains seems to be refuted by decreasing trends of child feeding practices and access to adequate and diverse diets leading to food insecurity.
Review points out to gradual imporvement of health indicators, however, large inequities by geography, gender, wealth, religion, and region exist. According to the
United Nations, ‘universal health coverage is a political investment and implementation opportunity to advance the health of women, children and adolescents’ and cannot be universalised unless everyone is reached, including those in fragile settings. UHC cannot be universal unless everyone is reached, including those in fragile settings.
At the current pace, Ayushman Bharat could miss the target of operationalising 1.5 lakh health and wellness centres (HWCs) by December 2022 according to
NITI Aayog. All states need to address the human resource gaps and ensure implementation of services to reach the target. The pandemic has further hit all countries with adverse impact on vulnerable communities and populations more prone to diseases and poor access to healthcare services. The
Economic Survey 2020-21 suggests increase in public spending on healthcare from 1 to 2.5-3 percent to reduce the OOPE from 65 to 35 percent. Learning from the pandemic, it suggests India’s healthcare policy to focus on its long-term healthcare priorities.
The
way forward lies in re-designing and strengthening the health system. For effective implementation requires increased government investment on health along with scaling up of ongoing initiatives. To achieve universal health coverage, requires a multisectoral approach and innovative policies and porgrams. The
pandemic has forced healthcare systems to review and adapt models of care to the evolving situation. The role of technology enabled platforms like e-Sanjeevani along with digitization and artificial intelligence at-scale can help meet the last-mile challenges of healthcare delivery. With the National Digital Health Mission rollout will further stregthen the implementation and coverage of the Ayushman Bharat scheme. A lot needs to be done to build a fairer, healthier nation.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.



 Today, 7th April, is celebrated as World Health Day since 1950 to create global health awareness. This year the theme ‘Building a fairer, healthier world’ calls for action to eliminate health inequities and create an environment conducive to good health. ‘Health for all’ is a critical component in the United Nations' 2030 agenda for Sustainable Development Goals. The
Today, 7th April, is celebrated as World Health Day since 1950 to create global health awareness. This year the theme ‘Building a fairer, healthier world’ calls for action to eliminate health inequities and create an environment conducive to good health. ‘Health for all’ is a critical component in the United Nations' 2030 agenda for Sustainable Development Goals. The 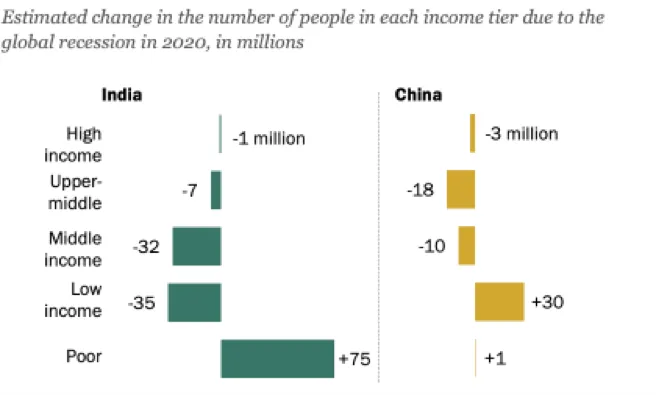 Figure 1: Estimated number of people as per wealth quintile due to pandemic recession.
Source: Pew Research Center
According to the
Figure 1: Estimated number of people as per wealth quintile due to pandemic recession.
Source: Pew Research Center
According to the 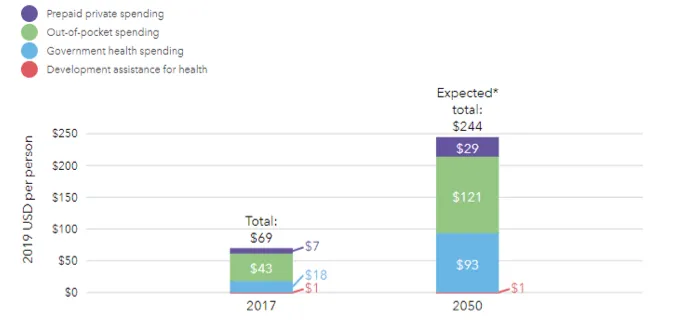 Figure 2: Spending on Health by India – now and in the future.
Source:
Figure 2: Spending on Health by India – now and in the future.
Source: 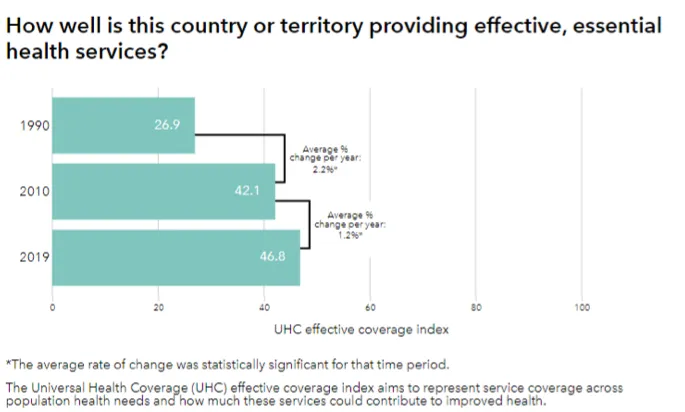 Figure 3: The Universal Health Coverage index for India
Source: IHME
India’s diseases burden is changing from non-infectious to lifestyle diseases. In recent decade, non-communicable diseases (NCDs) have caused significant threat to public health, with top 3 causes of deaths attributable to NCDs (Figure 4). The reasons range from genetic predisposition, unhealthy eating to sedentary lifestyle.
Figure 3: The Universal Health Coverage index for India
Source: IHME
India’s diseases burden is changing from non-infectious to lifestyle diseases. In recent decade, non-communicable diseases (NCDs) have caused significant threat to public health, with top 3 causes of deaths attributable to NCDs (Figure 4). The reasons range from genetic predisposition, unhealthy eating to sedentary lifestyle.
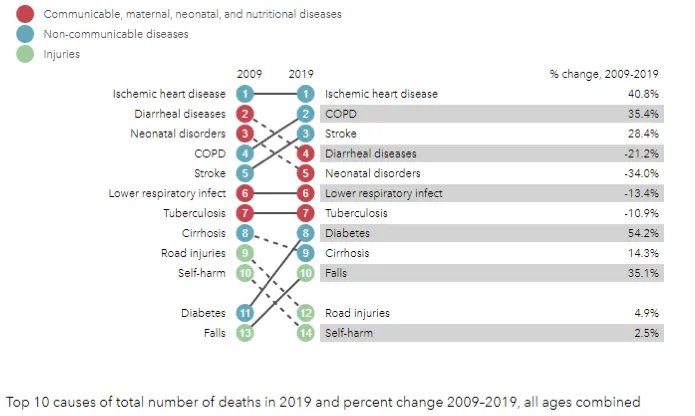 Figure 4: Top 10 causes of death for India
Source:
Figure 4: Top 10 causes of death for India
Source:  PREV
PREV