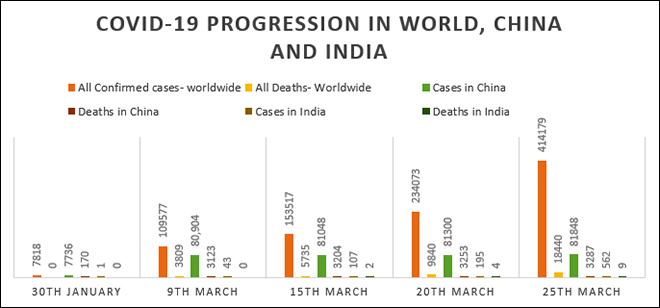
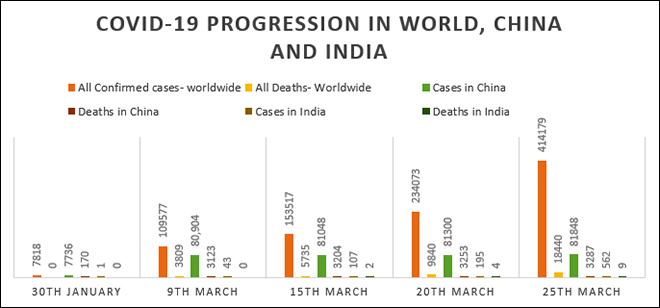
Having played havoc around the world in just a matter of weeks, the COVID19 pandemic needs no introduction. With some of the most advanced economies struggling to contain the virus, “Is India doing too little, too late?” is a question that has no easy answer. The world woke up to the reality of novel corona virus by the first week of 2020 when China contacted the World Health Organisation on 30 December 2019 about the ‘pneumonia of unknown cause.’ One month later, on 30 January, the first case of imported coronavirus was found in Kerala — the person reportedly had travel history to Wuhan. By that time, there were 7,818 cases reported globally, out of which only 82 cases were from 18 countries other than China. There were zero deaths in other countries while 70 deaths had occurred in China. The world was coming to terms with this rapidly spreading virus, which showed low mortality rate.
Progression
On 9 March 2020, Maharashtra reported its first case. By then, the world had witnessed 3,809 deaths, over 1 lakh infections and the disease had spread to over 104 countries. India had 43 total cases and no fatalities by that day.
Experts believe that India has already started walking on the exponential multiplication phase of the virus.
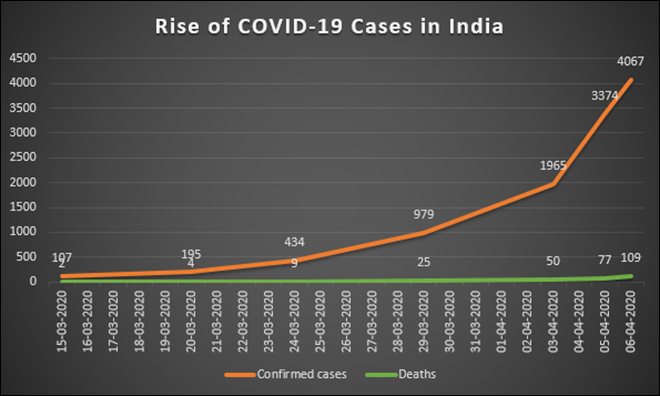
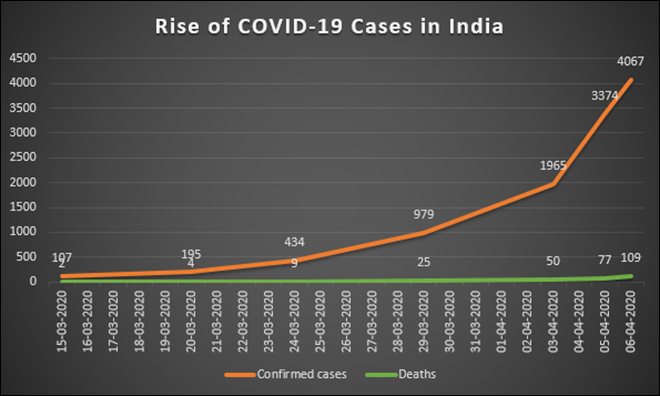
It took India to reach 40 days to have its 50th case. After that, just it took just five days to reach 100 cases (15 March) and five more days to 200 cases (19 March). We crossed 500 cases on 24 March, 1,000 cases by 29 March, 2,000 cases on 3 April and over 4,000 cases on 4 April. Currently, the number of cases in India are doubling every 4 days. Experts believe that India has already started walking on the exponential multiplication phase of the virus. ICMR, while ruling out community transmission scenario in India, did acknowledge indications by AIIMS director that there have been cases of localised and limited, yet community transmission in certain pockets in India.
Figure 1. Rise of COVID19 cases and mortality in India
With the development of a vaccine still a mystery, the government of India responded with the only reliable tool at its disposal — by announcing a 21-day nationwide lockdown. But for the movement of men engaged in emergency and essential services and goods, India was put under a state-mandated curfew. Several states invoked Section 144 of the Code of Criminal Procedure the to ensure that police action could be initiated if five or more people gathered publicly. Despite the lockdown now in its third week, however, the graph of positive cases has been rising by the day. Will such a lockdown — even if it is extended beyond the 21-day period — enough to arrest the spread of the virus in India?
Figure 2. COVID19 Progression in world, China and India
Projections
To answer that question, one needs to look at the projections for spread and mortality in India. Indian Council of Medical Research (ICMR) estimates that symptomatic cases would be about 1.5 million in Delhi, with around 500,000 each in Mumbai, Bengaluru and Kolkata, adding that such a situation would peak over a period of 200 days, beginning February. In the pessimistic scenario, the symptomatic cases would be about 10 million in Delhi and four million in Mumbai, which will peak in just 50 days starting February. Behind every mortality, the ICMR estimates India to have 8-10 severe patients and 40-50 non-severe ones. The Centre for Disease Dynamics, Economics and Policy estimates that in the age group 0-19 and 20-64, around 6% of population will require hospitalisation. The same in the case of age group above 64 is 28%.
Behind every mortality, the ICMR estimates India to have 8-10 severe patients and 40-50 non-severe ones.
The World Health Organisation (WHO), too, has been advising all the countries to step up the testing of citizens and to focus on social isolation. As on 24 March, the ICMR published a list of 104 government and 24 private laboratories that can conduct testing for SARS-COVID19. ICMR director general in a press conference on 22 March indicated that India has been testing only around 5,000 samples a week, which was set to be taken up to 70,000. That means around 200,000 samples per month.
The ICMR’s current testing strategy targets lists the following criteria
i. All asymptomatic individuals who have undertaken international travel in the last 14 days: they should stay in home quarantine for 14 days. They should be tested only if they become symptomatic (fever, cough, difficulty in breathing). All family members living with a confirmed case should be home quarantined.
ii. All symptomatic contacts of laboratory confirmed cases.
iii. All symptomatic health care workers.
iv. All hospitalised patients with severe acute respiratory illness (fever and cough and/or shortness of breath).
v. Asymptomatic direct and high-risk contacts of a confirmed case should be tested once between day five and day 14 of coming in his/her contact. Direct and high-risk contact includes those who live in the same household with a confirmed case and healthcare workers who examined a confirmed case without adequate protection as per WHO recommendations.
Ammunition for war against COVID19
While testing is the key, an infected person may not exhibit symptoms for about a week and might even test negative for about 4-7 days before developing active symptoms. As the virus is quite illusive, more the number of testing, the better. Does India have the capacity to even test the lower-end of projected infections? The answer is no. Even with the newly available capacity of around 200,000 sample testing a month. ICMR plans to have 100,000 tests per day capacity in worst case scenario if the disease spreads prolifically. But developing this level of capacity might take at least a month, if not more. A vast majority of the cases in India might not even exhibit symptoms (asymptomatic carriers) and thereby might not even get detected before they pass on the virus to high risk individuals — those with compromised immune system, ones with pre-existing illness and patients over the age of 70.
In India, there is one doctor for every 1,457 people — much lower than the WHO recommended 1:1,000 ratio. For rural areas, it is 1:10,926.
The WHO issued a ‘Disease Commodity Package’ for medical facilities all over the world highlighting the surveillance, care and treatment protocol for treating COVID19 cases on 6 March. The package highlights the requirement of pulse oximeters and ventilators for intensive and critical care of patients. How are India’s hospitals prepared in this respect? India has only 40,000 ventilators. World over, it has been observed that of the infected cases, around 25-30 percent require intensive care for which ventilators are a must. Geographical distribution of ventilators in India is also quite problematic; vast majority of them are concentrated in urban areas. In India, there is one doctor for every 1,457 people — much lower than the WHO recommended 1:1,000 ratio. For rural areas, it is 1:10,926. The government has placed an order of another 40,000 ventilators to Indian players and has sought around 10,000 more from China. India may need a million ventilators at the peak of its war on COVID19 and we’re not even accounting for the ventilator support required for cases related to non-COVID19 medical emergencies. Moreover, COVID19 itself may take its toll on hospitals if the doctors and health workers get infected on large numbers as has recently happened in Mumbai.
Therefore, it is important that India steps up testing. The testing protocol needs to prioritise the high-risk group of individuals with travel history because they are the one that will primarily need intensive care if they get infected. South Korea stepped up testing and has flattened the curve quite quickly. Secondly, India also needs to quickly scale up the infrastructure facilities where the cases are going to increase. Makeshift hospitals in exhibition centers and stadium could be made near urban areas to treat the affected. It is difficult to predict the required capacity, but each state may need more than one dedicated COVID19 hospital that ICMR is planning.
Lastly, what can we expect before the lockdown could be completely lifted (whenever that may be)? All the coronavirus cases must have either been treated or at least completely isolated for treatment with zero new additions for at least a week preceding 14 April. Getting there too presents a huge challenge to our healthcare infrastructure. We might be in for a longer haul with limited healthcare infrastructure facilities strained to more than their capacities.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.



 PREV
PREV

